Menopause: Difference between revisions
| Line 235: | Line 235: | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Primary care]] | |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Gynecology]] | [[Category:Gynecology]] | ||
Revision as of 21:27, 21 February 2013
For patient information, click here
| Menopause | |
 | |
|---|---|
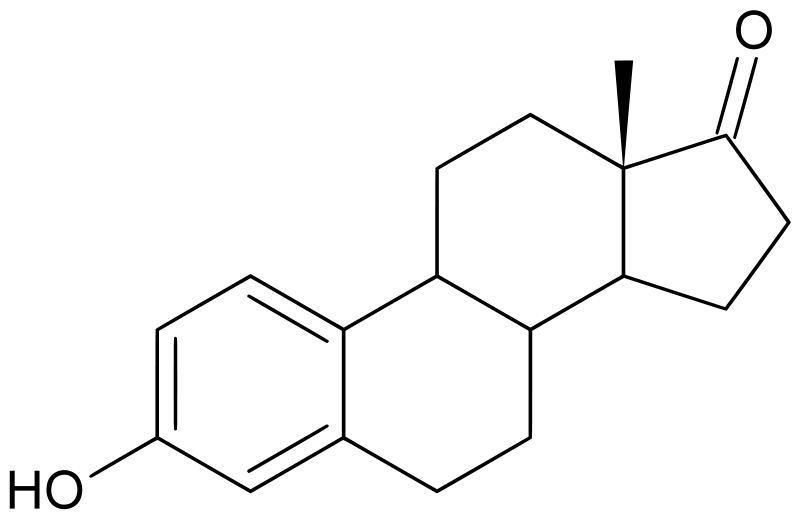
| The estrogen estrone. In postmenopausal women more estrone is present than estradiol. | |
| ICD-10 | E28.3, N95.1 |
| ICD-9 | 627 |
| DiseasesDB | 8034 |
| MedlinePlus | 000894 |
| MeSH | D008593 |
|
WikiDoc Resources for Menopause |
|
Articles |
|---|
|
Most recent articles on Menopause |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Menopause at Clinical Trials.gov Clinical Trials on Menopause at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Menopause
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Menopause Discussion groups on Menopause Directions to Hospitals Treating Menopause Risk calculators and risk factors for Menopause
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Menopause |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [6]
Overview
The word menopause literally means the permanent physiological, or natural, cessation of menstrual cycles, from the Greek roots 'meno-' (month) and 'pausis' (a pause, a cessation). In other words, menopause means the natural and permanent stopping of the monthly female reproductive cycles, which is usually manifest as a permanent absence of monthly periods or menstruation.
The word menopause is most often used in regard to human females, where menopause happens more or less in midlife, signaling the end of the fertile phase of a woman's life, and ushering in the third, traditionally wiser, part of a woman's life. Menopause is perhaps most easily understood as the opposite process to menarche.
Menopause in women cannot however simply be defined as the permanent "stopping of the monthly periods", because in reality what is happening to the uterus is quite secondary to the process. In fact the uterus can be surgically removed (hysterectomy) in a younger woman, and although the periods will cease permanently and the woman will technically be infertile, as long as the ovaries (or one ovary) are, or is, still functioning, the woman will not be in menopause, because ovulation, and the release of the sequence of reproductive hormones that are an essential part of the reproductive cycles, will continue until the normal time of menopause is reached.
Menopause is in fact triggered by the faltering and shutting down (or surgical removal of) of the ovaries, which are a part of the body's endocrine system of hormone production, in this case the hormones which make sexual behavior and reproduction possible.
The process of the ovaries shutting down is a phenomenon which involves the entire cascade of a woman's reproductive functioning from brain to skin, and this major physiological event usually has some effect on almost every aspect of a woman's body and life.
Menopause starts as the ovaries begin to fail to be able to produce an egg or ovum every month. Since the process of producing and ripening the egg is also what creates several of the key hormones involved in the monthly cycle, this in turn interrupts the regular pattern of the hormone cycles, and gradually leads to the somewhat chaotic and long-drawn out shutting down of the whole reproductive system.
The break-up in the pattern of the menstrual cycles not only causes the levels of most of the reproductive hormones to drop over time, but also causes the reproductive hormones to fall out of phase with one another, which often leads to extreme and unpredictable fluctuations in the levels, which itself can cause numerous different symptoms such as hot flashes, etc, in most women. After a number of years of erratic functioning, the ovaries almost completely stop producing hormones: estrogens, progestin and testosterone, and the reproductive system ceases to function.
Age of onset
The average age of menopause is 51 years, and the normal age range for last period ever is somewhere between age 45 to 55. Age 55 to 60 for last period ever is described as a "late menopause". An "early menopause" is defined as last period ever between the age of 40 to 45.
Some women reach menopause at a much younger age than average, especially if they have had cancer or another serious illness, and have undergone chemotherapy. This is sometimes referred to as a "chemical menopause".
Premature menopause (or premature ovarian failure) is defined as last period ever occurring before the age of 40; it occurs in 1% of women and is not viewed as being due to normal causes. Some known causes of spontaneous premature menopause include autoimmune disorders, thyroid disease, and diabetes mellitus, but often it is idiopathic or due to unknown causes.
Premature menopause is diagnosed or confirmed by measuring the levels of follicle stimulating hormone (FSH) and luteinizing hormone (LH); the levels of these hormones will be higher if menopause has occurred. Rates of premature menopause have been found to be significantly higher in fraternal and identical twins; approximately 5% of twins reach menopause before the age of 40. The reasons for this are not completely understood. Transplants of ovarian tissue between identical twins have been successful in restoring fertility.
Menopause in other species
Unlike humans, other mammals rarely experience menopause, but it does exist in some of the other few mammal species that experience menstrual cycles, such as rhesus monkeys[1] and some cetaceans.[2]
The possible significance of menopause in human evolution
The Grandmother hypothesis considers that the menopause may have been selected for in human evolution, because later life infertility could actually have conferred an evolutionary advantage by allowing older women to spend more time helping with the survival of their existing children and grandchildren.
Terminology, definitions and commentary
Menopause
Clinically speaking, menopause is a date: the day after a woman's last period ever finishes. In common everyday parlance however, the word "menopause" is usually not used to refer to one day, but to the whole of the menopause transition years. This span of time is also referred to as the change of life or the climacteric and more recently is known as "perimenopause", (literally meaning "around menopause").
Perimenopause
Perimenopause means the menopause transition years, the years both before and after the last period ever, when the majority of women find that they undergo at least some symptoms of hormonal change and fluctuation, such as hot flashes, mood changes, insomnia, fatigue, etc.
During perimenopause, the production of most of the reproductive hormones, including estrogens and progestin, diminishes and becomes more irregular, often with wide and unpredictable fluctuations in levels. During this period, fertility diminishes.
Symptoms of perimenopause can begin as early as age 35, although most women become aware of them about 10 years later than this. Perimenopause can last for a few years, or for ten years or even longer. In this respect it resembles puberty, a similar process that surrounds menarche. In fact menopause can usefully be compared to "puberty in reverse", and the psychological adjustments that take place over this time span can be compared to adolescence. The actual duration and severity of perimenopause in any individual woman cannot be predicted in advance or during the process.
Not every woman suffers symptoms during perimenopause. Approximately one third of all women get no noticeable symptoms other than their periods becoming erratic and then stopping. Another one third of women have moderate symptoms. The remaining one third of women have very strong symptoms which tend to have a longer duration. The tendency to have a very strong perimenopause may be inherited in some cases.
One piece of recent research appears to show that melatonin supplementation in perimenopausal women can produce a highly significant improvement in thyroid function and gonadotropin levels, as well as restoring fertility and menstruation and preventing the depression associated with the menopause[3].
Premenopause
Premenopause is a word used to describe the years leading up to the last period ever, when the levels of reproductive hormones are already becoming lower and more erratic, and symptoms of hormone withdrawal may be present.
Postmenopause
Postmenopause is all of the time in a woman's life that take place after her last period ever, or more accurately, all of the time that follows the point when her ovaries become inactive.
A woman who still has her uterus can be declared to be in post-menopause once she has gone 12 full months with no flow at all, not even any spotting. When she reaches that point, she is one year into post-menopause. The reason for this delay in declaring a woman post-menopausal is because periods become very erratic at this time of life, and therefore a reasonably long stretch of time is necessary to be sure that the cycling has actually ceased.
In women who have no uterus, and therefore have no periods, post-menopause can be determined by a blood test which can reveal the very high levels of Follicle Stimulating Hormone (FSH) that are typical of post-menopausal women.
A woman's reproductive hormone levels continue to drop and fluctuate for some time into post-menopause, so any hormone withdrawal symptoms that a woman maybe experiencing do not necessarily stop right away, but may take quite some time, even several years, to disappear completely.
The causes of menopause
A natural or physiological menopause is that which occurs as a part of a woman's normal aging process. It is the result of the eventual atresia of almost all oocytes in the ovaries. This causes an increase in circulating follicle stimulating hormone (FSH) and luteinizing hormone (LH) levels as there are a decreased number of oocytes responding to these hormones and producing estrogen. This decrease in the production of estrogen leads to the perimenopausal symptoms of hot flashes, insomnia and mood changes, as well as post-menopausal osteoporosis and vaginal atrophy.
However, menopause can be surgically induced by bilateral salpingo-oophorectomy (removal of both ovaries and both fallopian tubes), which is often, but not always, done in conjunction with hysterectomy. Cessation of menses as a result of removal of the ovaries is called "surgical menopause". The sudden and complete drop in reproductive hormone levels usually produces extreme hormone-withdrawal symptoms such as hot flashes, etc.
As mentioned above, removal of the uterus, hysterectomy, does not itself cause menopause, although pelvic surgery can sometimes precipitate a somewhat earlier menopause, perhaps because of a compromised blood supply to the ovaries. Removing the ovaries however, causes an immediate and powerful "surgical menopause", even if the uterus is left intact.
Cigarette smoking has been found to decrease the age at menopause by as much as one year, and women who have undergone hysterectomy with ovary conservation go through menopause 3.7 years earlier than average. However, premature menopause (before the age of 40) is generally idiopathic.
Symptoms of perimenopause, the menopause transition time
As the body adapts to the changing levels of natural hormones, vasomotor symptoms such as hot flashes and palpitations, psychological symptoms such as depression, anxiety, irritability, mood swings and lack of concentration, and atrophic symptoms such as vaginal dryness and urgency of urination appear. Together with these symptoms, the woman may also have increasingly erratic menstrual periods.
These perimenopause symptoms are caused by an overall drop, as well as dramatic but erratic fluctuations, in the levels of estrogens, progestin, and testosterone. Some of these symptoms such as formication etc, may be associated with the hormone withdrawal process.
Vasomotor instability
- hot flashes, hot flushes, including night sweats
- sleep disturbances
Urogenital atrophy
- itching
- dryness
- bleeding
- watery discharge
- urinary frequency
- urinary urgency
- urinary incontinence
Skeletal
- osteoporosis gradually developing over time
- joint pain, muscle pain
- back pain
Skin, soft tissue
- breast atrophy
- skin thinning
- decreased elasticity
- formication, a sensation of pins and needles, or ants crawling on or under the skin
Psychological
Sexual
- decreased libido
- vaginal dryness
- problems reaching orgasm
- dyspareunia
A cohort study found that menopause was associated with hot flushes; joint pain and muscle pain; and depressed mood.[4] Menopause was not associated with poor sleep, decreased libido, and vaginal dryness.[4]
Treatment of symptoms
While perimenopause is a natural stage of life, when the symptoms are severe, this may be alleviated through medical treatments. Hormone therapy (HT) provides the best relief, but certain forms appear to pose a small increase in health risks, especially in women who start HT after menopause.
Some other drugs afford limited relief from hot flashes. A woman and her doctor should carefully review her symptoms and relative risk before determining whether the benefits of HT or other therapies outweigh the risks. Until more becomes known, women who elect to use hormone replacement therapy are generally well advised to take the lowest effective dose of HRT for the shortest period possible and to investigate whether certain forms may pose fewer dangers of clots or cancer than others.
Hormone therapy
In addition to relief from hot flashes, hormone therapy (HT) remains an effective treatment for osteoporosis. In HT, estrogens, progesterone or other hormones are administered to compensate for the body's own insufficiency to produce them. There are several types of therapies, with various side effects.
Conjugated equine estrogens
Conjugated equine estrogens contain estrogen molecules conjugated to hydrophilic side groups (e.g. sulfate) and are produced from Equidae-animals (horses).
Adverse effects
Women had been advised for many years that hormone therapy after menopause might reduce their risk of heart disease and prevent various aspects of aging. However, a large, randomized, controlled trial (the Women's Health Initiative) found that women undergoing HT with conjugated equine estrogens (Premarin), whether or not used in combination with a progestin (Premarin plus Provera), had, statistically-speaking, a slightly increased risk of breast cancer, heart disease, stroke, and Alzheimer's disease sufficient to justify stopping the study.
After these results were reported in 2002, the number of prescriptions written for Premarin and PremPro in the United States dropped almost in half, as many women discontinued HT altogether. The sharp drop in prescriptions for Premarin and PremPro following the mid-2002 announcement of their dangers was followed by large and successively greater drops in new breast cancer diagnoses at six months, one year, and 18 months after that announcement, for a cumulative 15% drop by the end of 2003. Surprisingly, no similar drop in Canada's breast cancer rates was observed during the same period, though prescriptions of PremPro and Premarin were reduced in Canada as well. Studies designed to track the further progression of this trend after 2003 are underway, as well as to determine if the drop is related to the reduced use of HRT.
Other forms of hormone therapy
Due to the controversy about Premarin-based hormone therapy, a number of doctors are now moving patients who request hormone therapy to help them through perimenopause, to bioidentical hormone products such as Estrace, a form of the precursor to estrogen in the human body known as estradiol, which have produced fewer side effects than conjugated equine estrogens[5].
However, all hormone replacement therapies probably do carry some health risks, including high blood pressure, blood clots, and increased risks of breast and uterine cancers. Women who have had a hysterectomy seem to tolerate estrogen-only therapy better than mixed-hormone therapy, and reduce the breast cancer risk brought on by progestin supplementation.
The anti-seizure medication gabapentin (Neurontin) seems to be second only to HRT in relieving hot flashes.
Antidepressants
Antidepressants such as paroxetine (Paxil), Fluoxetine hydrochloride (Prozac), and Venlafaxine hydrochloride (Effexor) have been used with some success in the treatment of hot flashes, improving sleep, mood, and quality of life. Of these, Paxil has been the most studied and may provide the most consistent relief. There is a theoretical reason why SSRI antidepressants might help with memory problems-- they increase circulating levels of the neurotransmitter serotonin in the brain and restore hippocampal function. Prozac has been repackaged as Sarafem and is approved and prescribed for premenstrual dysphoric disorder (PMDD), a mood disorder often exacerbated during perimenopause and early menopause. PMDD has been found by PET scans to be accompanied by a sharp drop in serotonin in the brain and to respond quickly and powerfully to SSRIs.
Blood pressure medicines
About as effective as antidepressants for hot flashes, but without the other mind and mood benefits of antidepressants, are blood pressure medicines including clonidine (Catapres). These drugs may merit special consideration by women suffering both from high blood pressure and hot flashes.
Complementary and alternative therapies
It should be noted that medical non-hormone treatments provide less than complete relief, and each has side effects.
In the area of complementary and alternative therapies, acupuncture treatment is promising. There are some studies indicating positive effects, especially on hot flashes [6][7][8] but also others [9] showing no positive effects of acupuncture regarding menopause.
There are claims that soy isoflavones are beneficial concerning menopause. However, a study [10] indicated that soy isoflavones did not improve or appreciably affect cognitive functioning in postmenopausal women.
Other remedies that have proven no better than a placebo at treating hot flashes and other menopause symptoms include red clover isoflavone extracts and black cohosh. Black cohosh has potentially serious side-effects such as the stimulation of breast cancer, therefore prolonged administration is not recommended in any case.
Other therapies
Individual counseling or support groups may be helpful to handle sad, depressed, or confusing feelings women may be having as their bodies change. Vaginal moisturizers such as Vagisil or Replens, can help women with thinning vaginal tissue or dryness. Lubricants, such as K-Y Jelly or Astroglide, can help with lubrication difficulties that may be present during intercourse. Moisturizers and lubricants are different products for different types of issues. Some women feel dry apart from sex and they may do better with moisturizers all the time. Those who just need lubricants are fine just using the lubrication products during intercourse. Low-dose vaginal estrogen is generally a safe way to take estrogen to solve vaginal thinning and dryness problems while only minimally increasing the levels of estrogen in the blood.
Obvious measures, such as drinking cold liquids and removing excess clothing layers when hot flashes strike, and avoiding hot flash triggers such as spicy foods, may supplement or supplant the use of medications for some women.
Related Chapters
- Hormone replacement therapy
- Estrogen
- Atrophic vaginitis
- Andropause (male menopause)
- Louann Brizendine
References
- ↑ Walker ML (1995). "Menopause in female rhesus monkeys". Am J Primatol. 35: 59–71.
- ↑ McAuliffe K, Whitehead H (2005). "Eusociality, menopause and information in matrilineal whales". Trends Ecol Evolution. 20: 650.
- ↑ Bellipanni G, DI Marzo F, Blasi F, et al. Effects of melatonin in perimenopausal and menopausal women: our personal experience. 2005. Ann N Y Acad Sci 1057:393-402. DOI: 10.1196/annals.1356.030 PMID 16399909
- ↑ 4.0 4.1 Freeman EW, Sammel MD, Lin H; et al. (2007). "Symptoms associated with menopausal transition and reproductive hormones in midlife women". Obstetrics and gynecology. 110 (2 Pt 1): 230–40. doi:10.1097/01.AOG.0000270153.59102.40. PMID 17666595.
- ↑ "Bioidentical Hormones Come Of Age", Marcelle Pick, OB/GYN Nurse Practitioner; published March 24, 2004; updated June 7, 2007; retrieved June 13, 2007.
- ↑ [1] Nir Y, Huang MI, Schnyer R, Chen B, Manber R. Stanford University School of Medicine, United States. amiryael@gmail.com
- ↑ [2] Cohen SM, Rousseau ME, Carey BL. University of Pittsburgh, 440 Victoria Bldg, 3500 Victoria St, Pittsburgh, PA 15261, USA. cohensu@pitt.edu
- ↑ [3] Zaborowska E, Brynhildsen J, Damberg S, Fredriksson M, Lindh-Astrand L, Nedstrand E, Wyon Y, Hammar M. Division of Obstetrics and Gynecology, Department of Molecular and Clinical Medicine, Faculty of Health Sciences, University Hospital, Linköping, Sweden.
- ↑ [4] Vincent A, Barton DL, Mandrekar JN, Cha SS, Zais T, Wahner-Roedler DL, Keppler MA, Kreitzer MJ, Loprinzi C. Mayo Clinic College of Medicine, Rochester, MN 55905, USA.
- ↑ [5] Fournier LR, Ryan Borchers TA, Robison LM, Wiediger M, Park JS, Chew BP, McGuire MK, Sclar DA, Skaer TL, Beerman KA. Department of Psychology, Washington State University, Pullman, WA 99164-4820, USA. Fournier@wsunix.wsu.edu
Template:Reproductive physiology
de:Menopause eo:Menopaŭzo ko:갱년기 io:Menopauzo id:Menopause it:Menopausa lt:Menopauzė mk:Менопауза ml:ആര്ത്തവ വിരാമം nl:Menopauze no:Menopause fi:Vaihdevuodet sv:Klimakterium uk:Менопауза