Membranous glomerulonephritis pathophysiology
|
Membranous glomerulonephritis Microchapters |
|
Differentiating Membranous glomerulonephritis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Membranous glomerulonephritis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Membranous glomerulonephritis pathophysiology |
|
Directions to Hospitals Treating Membranous glomerulonephritis |
|
Risk calculators and risk factors for Membranous glomerulonephritis pathophysiology |
- Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
Overview
It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
Pathophysiology
- MGN is caused by immune complex formation in the glomerulus. The immune complexes are formed by binding of antibodies to antigens in the glomerular basement membrane. The antigens may be part of the basement membrane, or deposited from elsewhere by the systemic circulation.
- The immune complex serves as an activator that triggers a response from the complement system and form a membrane attack complex which stimulates release of proteases and oxidants by the mesangial and epithelial cells, damaging the capillary walls and causing them to become "leaky".
Phospholipase A2 receptor
- The M-type PLA2R is the major antigen in human idiopathic MN. It is expressed in glomerular podocytes.
- There was no colocalization of PLA2R in secondary MN biopsies.
- PLA2R antigen detected within immune deposits by immunofluorescence of the biopsy specimen. [26]
- Detection of the immune complex specificity is 100 percent.
Thrombospondin type-1
- THSD7A has been found in patients with idiopathic MN who are negative for anti-PLA2R antibodies.
Neutral endopeptidase
- Anti-neutral endopeptidase antibodies caused MN in the neonates.
- It resolves months after birth.
- The T helper-2 predominates in MN and minimal change disease.
Genetics
Associated Conditions
Gross Pathology
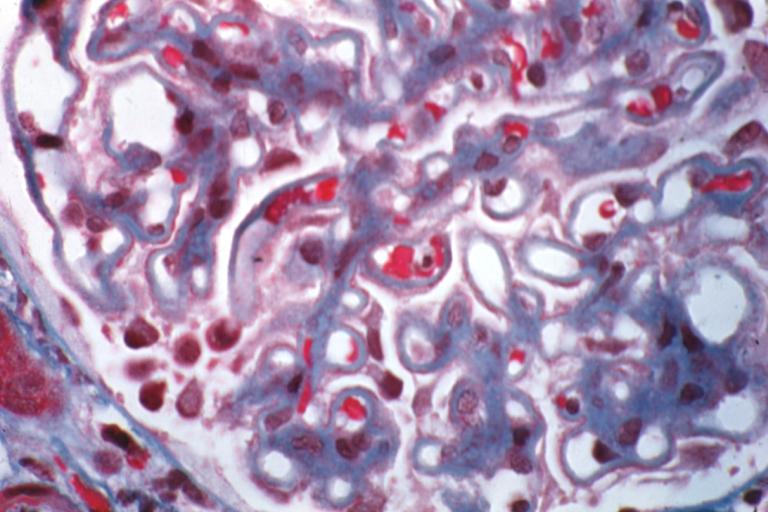
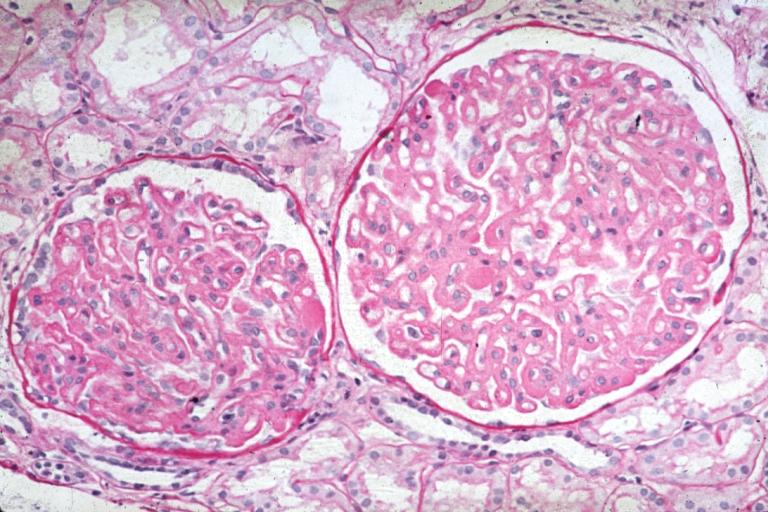
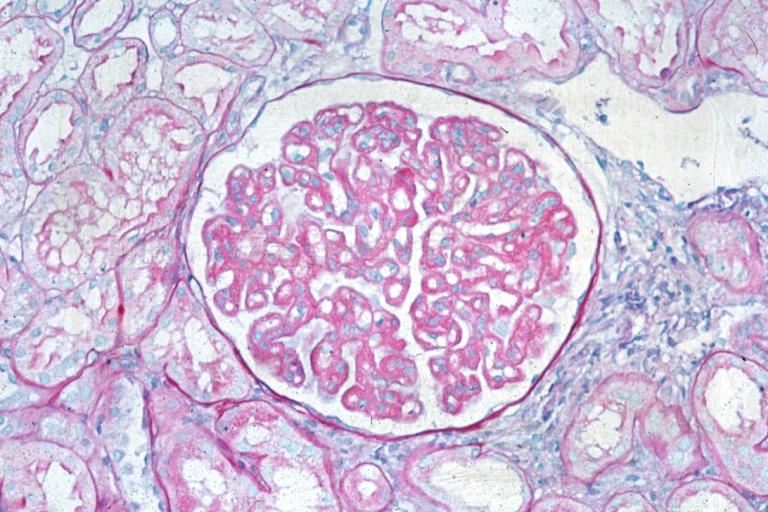
Microscopic Pathology
- Early biopsies may be normal
- Later: uniform diffuse capillary wall thickening without hypercellularity, without mesangial sclerosis and without inflammatory cells
- Proximal convoluted tubules contain hyaline droplets, reflecting protein reabsorption
- With progression, get membrane thickening, narrow capillary lumina, mesangial sclerosis and glomerulosclerosis
Immunofluorescence
- Granular diffuse peripheral deposits, usually IgG and C3, also C5b-C9 and occasionally IgM or IgA
- C4d immunostaining may be diagnostic (Histol Histopathol 2011;26:1391)
Stages
- Stage I: LM - normal for slightly thickened BM, slight GMB vacuolization; IF - fine granular IgG, C3; EM - scattered small subepithelial electron dense deposits, no foot process effacement or spikes
- Stage II: LM - moderately thickened BM with spikes and vacuolization; IF - moderate sized, granular IgG, C3; EM - diffuse spikes due to subepithelial deposits, diffuse foot process effacement
- Stage III: LM - markedly thickened GBM, residual spikes and vacuoles, chain like appearance; IF - coarsely granular IgG, C3; EM - intramembranous deposits, spikes, neomembrane formation and diffuse foot process effacement
- Stage IV: LM - markedly thickened GBM, few spikes, vacuoles and glomerulosclerosis; IF - focal IgG, C3; EM - sclerotic GBM, few deposits and lacunae
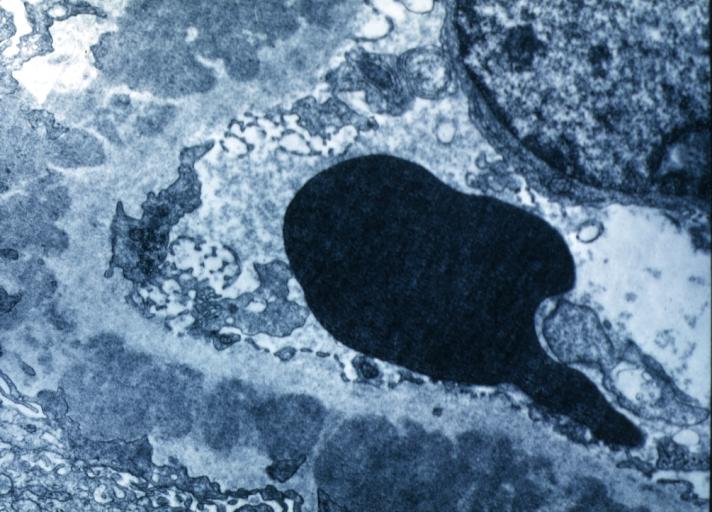
Electron microscopy
- Subepithelial deposits that nestle against the glomerular basement membrane seems to be the cause of the thickening.
- The podocytes lose their foot processes.
- As the disease progresses, the deposits will eventually be cleared, leaving cavities in the basement membrane.
References
-
Membranous Glomerulonephritis: Electron micrography. An excellent example to show thickened basement membrane and immune complexes.
-
Membranous Glomerulonephritis: Micro trichrome high mag excellent to show thickened capillary basement membranes
-
Membranous Glomerulonephritis: Micro PAS high mag excellent example of this lesion
-
Membranous Glomerulonephritis: Micro PAS med mag