Lymphangioma pathophysiology: Difference between revisions
No edit summary |
|||
| (31 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Lymphangioma}} | {{Lymphangioma}} | ||
{{CMG}} {{AE}} {{HL}} | {{CMG}} {{AE}} {{Badria}} {{HL}} | ||
==Overview== | ==Overview== | ||
Lymphangioma arises from [[lymph]] vessels, which are normally involved in the re-circulation of excess body [[fluid]] back into the [[blood]] stream. The exact [[pathogenesis]] of [[lymphangioma]] is not fully understood. It is thought that [[lymphangioma]] is caused by either sequestration of [[lymph]] tissue, abnormal [[budding]] of [[lymph]] vessels, lack of fusion with the [[venous]] system, or obstruction of [[lymph]] vessels. [[Lymphangiomas]] most commonly develop at the [[head]] and [[neck]] regions. [[Lymphangioma]] is associated with a number of conditions that include [[Turner syndrome]] and [[Down syndrome]]. On gross pathology, characteristic findings of [[lymphangioma]] include a grey-white, well circumscribed, edematous mass with a variable size and consistency. On microscopic [[histopathological]] analysis, characteristic findings of [[lymphangioma]] include thin walled [[endothelial]] lining, [[intraluminal]] accumulation of [[eosinophilic]] deposits, and clusters of [[intraluminal]] [[lymphocyte]]s. | |||
==Pathogenesis== | ==Pathogenesis== | ||
* Lymphangioma arises from | * [[Lymphangioma]] arises from [[lymph]] vessels, which are normally involved in the re-circulation of excess body [[fluid]] back into the [[blood]] stream.<ref name="pmid18500536">{{cite journal |vauthors=Wiegand S, Eivazi B, Barth PJ, von Rautenfeld DB, Folz BJ, Mandic R, Werner JA |title=Pathogenesis of lymphangiomas |journal=Virchows Arch. |volume=453 |issue=1 |pages=1–8 |date=July 2008 |pmid=18500536 |doi=10.1007/s00428-008-0611-z |url=}}</ref> | ||
* The exact mechanism of development of abnormal [[malformations]] is not known. | |||
* The exact | * It is suggested that [[lymphangioma]] is formed as a result of one of four mechanisms: | ||
** Sequestration of [[lymph]] tissue. | |||
** Abnormal [[budding]] of [[lymph]] vessels. | |||
** Lack of fusion with the [[venous]] system. | |||
** Obstruction of [[lymph]] vessels. | |||
*Whimster describes [[pathogenesis]] of [[lymphangioma]] as the collection of [[Lymphatic drainage|lymphatic cisterns]] in the deep [[Subcutaneous tissue|subcutaneous]] plane which get detached from normal network, however they keep connected to [[superficial]] [[lymph]] vessels through short and dilated [[vessels]].<ref name="pmid27134953">{{cite journal |vauthors=Ersoy AO, Oztas E, Saridogan E, Ozler S, Danisman N |title=An Unusual Origin of Fetal Lymphangioma Filling Right Axilla |journal=J Clin Diagn Res |volume=10 |issue=3 |pages=QD09–11 |date=March 2016 |pmid=27134953 |pmc=4843338 |doi=10.7860/JCDR/2016/18516.7513 |url=}}</ref> | |||
* The cisterns originally [[Derived|derive]] from [[Primitive (integral)|primitive]] [[lymph]] sac, which fail to connect to normal [[Circulatory system|circulation]]. | |||
* These are covered with thick [[muscular]] coat, which on [[contraction]] increase external pressure. | |||
* Ultimately leads to dilated sacs which are visible on [[skin]] as out-pouchings.<ref name="pmid26967121">{{cite journal |vauthors=Chang MB, Newman CC, Davis MD, Lehman JS |title=Acquired lymphangiectasia (lymphangioma circumscriptum) of the vulva: Clinicopathologic study of 11 patients from a single institution and 67 from the literature |journal=Int. J. Dermatol. |volume=55 |issue=9 |pages=e482–7 |date=September 2016 |pmid=26967121 |doi=10.1111/ijd.13264 |url=}}</ref> | |||
* Whimster's description is proved with radio-graphic evidence as well.<ref name="pmid15149994">{{cite journal |vauthors=Levy AD, Cantisani V, Miettinen M |title=Abdominal lymphangiomas: imaging features with pathologic correlation |journal=AJR Am J Roentgenol |volume=182 |issue=6 |pages=1485–91 |date=June 2004 |pmid=15149994 |doi=10.2214/ajr.182.6.1821485 |url=}}</ref> | |||
** Which showed large multilobulated cisterns extend deep in the [[dermis]] and laterally beyond the clinical lesions. | |||
** These deep [[lymphangiomas]] had no connections with the adjacent normal lymphatics. | |||
* Some lymphangiomas may represent vascular malformations during [[embryonic development]] rather than as [[Neoplasms|true neoplasms]]. | |||
* For more information on vascular anamolies '''[[Vascular anomalies|click here]].''' | |||
* Development of [[lymphangiomas]] is mediated by [[Vascular endothelial growth factor|vascular endothelial growth factors]].<ref name="pmid163552142">{{cite journal |vauthors=Ferrara N, Kerbel RS |title=Angiogenesis as a therapeutic target |journal=Nature |volume=438 |issue=7070 |pages=967–74 |date=December 2005 |pmid=16355214 |doi=10.1038/nature04483 |url=}}</ref> | |||
==== Acquired [[lymphangiomas]] <ref name="pmid29186257">{{cite journal |vauthors=Oliveti A, Biasi TB, Funchal GDG |title=Lymphangioma secondary to irradiation after mastectomy |journal=An Bras Dermatol |volume=92 |issue=3 |pages=395–397 |date=2017 |pmid=29186257 |pmc=5514585 |doi=10.1590/abd1806-4841.20173952 |url=}}</ref> ==== | |||
Acquired [[lymphangiomas]] arise as a consequence of any interruption of previously normal lymphatic drainage such as:<ref name="pmid29186257" /> <ref name="pmid28913305">{{cite journal |vauthors=Hwang J, Lee YK, Burm JS |title=Treatment of Tongue Lymphangioma with Intralesional Combination Injection of Steroid, Bleomycin and Bevacizumab |journal=Arch Craniofac Surg |volume=18 |issue=1 |pages=54–58 |date=March 2017 |pmid=28913305 |pmc=5556746 |doi=10.7181/acfs.2017.18.1.54 |url=}}</ref> | |||
* Surgery | |||
* Trauma | |||
* Infection | |||
* Malignancy | |||
* Radiation therapy | |||
==Genetics== | ==Genetics== | ||
* [[Genetic mutation]]s involved in the [[pathogenesis]] of [[lymphangioma]] include: | |||
:* [[Trisomy 13]] | |||
:* [[Trisomy 18]] | |||
:* [[Trisomy 21]] | |||
==Associated Conditions== | ==Associated Conditions== | ||
* Lymphangioma is associated with a number of conditions that include:<ref name="EvansLonsdale2008">{{cite journal|last1=Evans|first1=D. G. R.|last2=Lonsdale|first2=R. N.|last3=Patton|first3=M. A.|title=Cutaneous lymphangioma and amegakaryocytic thrombocytopenia in Noonan syndrome|journal=Clinical Genetics|volume=39|issue=3|year=2008|pages=228–232|issn=00099163|doi=10.1111/j.1399-0004.1991.tb03017.x}}</ref> | |||
:* [[Turner syndrome]] | |||
:* [[Noonan syndrome]] | |||
:* [[Down syndrome]] | |||
==Gross Pathology== | ==Gross Pathology== | ||
* On gross pathology, characteristic findings of lymphangioma include:<ref name="pmid28877380">{{cite journal |vauthors=Chotai N, Fok E, Chan P, Ho B |title=Axillary lymphangioma in an asymptomatic adult female |journal=Breast J |volume=24 |issue=3 |pages=415–416 |date=May 2018 |pmid=28877380 |doi=10.1111/tbj.12915 |url=}}</ref> | |||
:* Grey-white mass | |||
:* Well circumscribed | |||
:* Edematous appearance | |||
:* Variable size (may be massive) | |||
:* Filled with [[serous]] fluid | |||
:* Smooth inner lining | |||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
* On microscopic [[histopathological]] analysis, characteristic findings of [[lymphangioma]] include:<ref name="pmid288773802">{{cite journal |vauthors=Chotai N, Fok E, Chan P, Ho B |title=Axillary lymphangioma in an asymptomatic adult female |journal=Breast J |volume=24 |issue=3 |pages=415–416 |date=May 2018 |pmid=28877380 |doi=10.1111/tbj.12915 |url=}}</ref> | |||
:* Thin walled channels lined by [[endothelium|endothelium.]] | |||
:* [[Intraluminal]] accumulation of [[eosinophilic]] deposits. | |||
:* Clusters of intraluminal [[lymphocyte]]s. | |||
:* No atypical [[vascular]] features. | |||
:* [[Nuclear]] [[atypia]]. | |||
:* [[Mitosis|Mitotic activity.]] | |||
:* [[Koilocytosis|Koilocytic]] changes. | |||
:* A mild to the moderate [[Inflammation|inflammatory]] infiltrate may be present. | |||
== Immunohistochemistry: == | |||
* On [[Immunohistochemistry|immunohistochemistry,]] characteristic findings of [[lymphangioma]] include: | |||
:* D2-40 +ve | |||
==Gallery== | ==Gallery== | ||
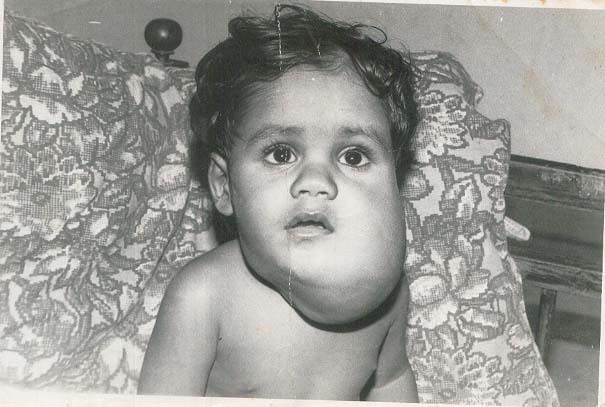
[[Image:Lymphangioma.jpg|500px|thumb|left|Image showing lymphangioma [https://upload.wikimedia.org/wikipedia/commons/2/2b/Lymphangioma.jpg Source:Wikipedia]]] | |||
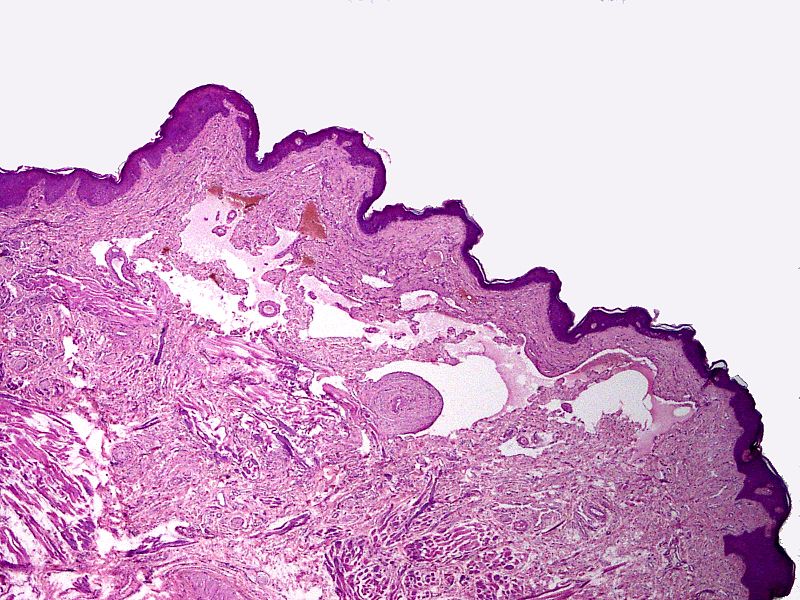
[[Image:Lympangioma 2.JPG|500px|thumb|left|Image showing lymphangioma [https://en.wikipedia.org/wiki/Lymphangioma#/media/File:SkinTumors-PB061069.JPG Source:Wikipedia]]] | |||
<br style="clear:left" /> | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
| Line 22: | Line 85: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Vascular medicine]] | |||
Latest revision as of 16:17, 18 January 2019
|
Lymphangioma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Lymphangioma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Lymphangioma pathophysiology |
|
Risk calculators and risk factors for Lymphangioma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Badria Munir M.B.B.S.[2] Haytham Allaham, M.D. [3]
Overview
Lymphangioma arises from lymph vessels, which are normally involved in the re-circulation of excess body fluid back into the blood stream. The exact pathogenesis of lymphangioma is not fully understood. It is thought that lymphangioma is caused by either sequestration of lymph tissue, abnormal budding of lymph vessels, lack of fusion with the venous system, or obstruction of lymph vessels. Lymphangiomas most commonly develop at the head and neck regions. Lymphangioma is associated with a number of conditions that include Turner syndrome and Down syndrome. On gross pathology, characteristic findings of lymphangioma include a grey-white, well circumscribed, edematous mass with a variable size and consistency. On microscopic histopathological analysis, characteristic findings of lymphangioma include thin walled endothelial lining, intraluminal accumulation of eosinophilic deposits, and clusters of intraluminal lymphocytes.
Pathogenesis
- Lymphangioma arises from lymph vessels, which are normally involved in the re-circulation of excess body fluid back into the blood stream.[1]
- The exact mechanism of development of abnormal malformations is not known.
- It is suggested that lymphangioma is formed as a result of one of four mechanisms:
- Whimster describes pathogenesis of lymphangioma as the collection of lymphatic cisterns in the deep subcutaneous plane which get detached from normal network, however they keep connected to superficial lymph vessels through short and dilated vessels.[2]
- The cisterns originally derive from primitive lymph sac, which fail to connect to normal circulation.
- These are covered with thick muscular coat, which on contraction increase external pressure.
- Ultimately leads to dilated sacs which are visible on skin as out-pouchings.[3]
- Whimster's description is proved with radio-graphic evidence as well.[4]
- Which showed large multilobulated cisterns extend deep in the dermis and laterally beyond the clinical lesions.
- These deep lymphangiomas had no connections with the adjacent normal lymphatics.
- Some lymphangiomas may represent vascular malformations during embryonic development rather than as true neoplasms.
- For more information on vascular anamolies click here.
- Development of lymphangiomas is mediated by vascular endothelial growth factors.[5]
Acquired lymphangiomas [6]
Acquired lymphangiomas arise as a consequence of any interruption of previously normal lymphatic drainage such as:[6] [7]
- Surgery
- Trauma
- Infection
- Malignancy
- Radiation therapy
Genetics
- Genetic mutations involved in the pathogenesis of lymphangioma include:
Associated Conditions
- Lymphangioma is associated with a number of conditions that include:[8]
Gross Pathology
- On gross pathology, characteristic findings of lymphangioma include:[9]
- Grey-white mass
- Well circumscribed
- Edematous appearance
- Variable size (may be massive)
- Filled with serous fluid
- Smooth inner lining
Microscopic Pathology
- On microscopic histopathological analysis, characteristic findings of lymphangioma include:[10]
- Thin walled channels lined by endothelium.
- Intraluminal accumulation of eosinophilic deposits.
- Clusters of intraluminal lymphocytes.
- No atypical vascular features.
- Nuclear atypia.
- Mitotic activity.
- Koilocytic changes.
- A mild to the moderate inflammatory infiltrate may be present.
Immunohistochemistry:
- On immunohistochemistry, characteristic findings of lymphangioma include:
- D2-40 +ve
Gallery
References
- ↑ Wiegand S, Eivazi B, Barth PJ, von Rautenfeld DB, Folz BJ, Mandic R, Werner JA (July 2008). "Pathogenesis of lymphangiomas". Virchows Arch. 453 (1): 1–8. doi:10.1007/s00428-008-0611-z. PMID 18500536.
- ↑ Ersoy AO, Oztas E, Saridogan E, Ozler S, Danisman N (March 2016). "An Unusual Origin of Fetal Lymphangioma Filling Right Axilla". J Clin Diagn Res. 10 (3): QD09–11. doi:10.7860/JCDR/2016/18516.7513. PMC 4843338. PMID 27134953.
- ↑ Chang MB, Newman CC, Davis MD, Lehman JS (September 2016). "Acquired lymphangiectasia (lymphangioma circumscriptum) of the vulva: Clinicopathologic study of 11 patients from a single institution and 67 from the literature". Int. J. Dermatol. 55 (9): e482–7. doi:10.1111/ijd.13264. PMID 26967121.
- ↑ Levy AD, Cantisani V, Miettinen M (June 2004). "Abdominal lymphangiomas: imaging features with pathologic correlation". AJR Am J Roentgenol. 182 (6): 1485–91. doi:10.2214/ajr.182.6.1821485. PMID 15149994.
- ↑ Ferrara N, Kerbel RS (December 2005). "Angiogenesis as a therapeutic target". Nature. 438 (7070): 967–74. doi:10.1038/nature04483. PMID 16355214.
- ↑ 6.0 6.1 Oliveti A, Biasi TB, Funchal G (2017). "Lymphangioma secondary to irradiation after mastectomy". An Bras Dermatol. 92 (3): 395–397. doi:10.1590/abd1806-4841.20173952. PMC 5514585. PMID 29186257. Vancouver style error: initials (help)
- ↑ Hwang J, Lee YK, Burm JS (March 2017). "Treatment of Tongue Lymphangioma with Intralesional Combination Injection of Steroid, Bleomycin and Bevacizumab". Arch Craniofac Surg. 18 (1): 54–58. doi:10.7181/acfs.2017.18.1.54. PMC 5556746. PMID 28913305.
- ↑ Evans, D. G. R.; Lonsdale, R. N.; Patton, M. A. (2008). "Cutaneous lymphangioma and amegakaryocytic thrombocytopenia in Noonan syndrome". Clinical Genetics. 39 (3): 228–232. doi:10.1111/j.1399-0004.1991.tb03017.x. ISSN 0009-9163.
- ↑ Chotai N, Fok E, Chan P, Ho B (May 2018). "Axillary lymphangioma in an asymptomatic adult female". Breast J. 24 (3): 415–416. doi:10.1111/tbj.12915. PMID 28877380.
- ↑ Chotai N, Fok E, Chan P, Ho B (May 2018). "Axillary lymphangioma in an asymptomatic adult female". Breast J. 24 (3): 415–416. doi:10.1111/tbj.12915. PMID 28877380.