Lung mass imaging: Difference between revisions
| Line 8: | Line 8: | ||
==Imaging== | ==Imaging== | ||
Lung mass can be divided into 2 categories: | |||
:*'''Hyperdense pulmonary mass''' | :*'''Hyperdense pulmonary mass''' | ||
:*'''Cavitating pulmonary mass''' | :*'''Cavitating pulmonary mass''' | ||
*The evaluation of lung mass will depend on | '''Hyperdense pulmonary mass''' | ||
*Hyperdense pulmonary mass is defined as a pulmonary mass with internal calcification | |||
*The most common causes of hyerdense pulmonary mass, include: granuloma (most common), pulmonary hamartoma, bronchogenic carcinoma, carcinoid tumors, and pulmonary metastases. | |||
'''Cavitating pulmonary mass''' | |||
*Cavitating pulmonary mass is defined as a gas-filled area of the lung in the center of a nodule, mass or area of consolidation | |||
*It is also characterized by a thick wall (must be greater than 2-5 mm) | |||
*The most common causes of cavitating pulmonary mass, include malignancies, infections, inflammation processes, and congenital malformations. | |||
*The table below summarizes the most common causes of cavitating pulmonary mass | |||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 1000px" align=center | |||
|valign=top| | |||
|+ | |||
! style="background: #4479BA; width: 100px;" | {{fontcolor|#FFF|'''Cavitating causes'''}} | |||
! style="background: #4479BA; width: 300px;" | {{fontcolor|#FFF|'''Conditions'''}} | |||
! style="background: #4479BA; width: 300px;" | {{fontcolor|#FFF|'''Description'''}} | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" | Malignancy | |||
| style="padding: 5px 5px; background: #F5F5F5;"| | |||
Cancer | |||
*Primary bronchogenic carcinoma(especially squamous cell carcinoma) | |||
*Cavitating pulmonary metastases (especially squamous cell carcinoma, GI adenocarincoma, sarcoma) | |||
|style="padding: 5px 5px; background: #F5F5F5;"| | |||
Cancer | |||
*Thick wall | |||
*Irregular shape | |||
*Disort of adjacent structures | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" | Infection | |||
| style="padding: 5px 5px; background: #F5F5F5;"| | |||
*Pulmonary bacterial abscess/cavitating pneumonia | |||
*Empyema | |||
*Post-pneumonic pneumatocoele | |||
*Septic pulmonary emboli | |||
*Pulmonary coccidioidomycosis | |||
*Pulmonary actinomycosis / thoracic actinomycosis | |||
*Pulmonary nocardiosis | |||
*Melioidosis | |||
*Pulmonary cryptococcosis | |||
|style="padding: 5px 5px; background: #F5F5F5;"| | |||
Abscess: | |||
*Round in all projections | |||
*Abruptly interrupts bronchovascular structures | |||
*May form a acute angle with the costal surface / chest wall | |||
*Abscesses have thick irregular walls | |||
*Abscesses usually have an acute angle (claw sign) | |||
Empyema: | |||
*Smoother margins | |||
*Lentiform shape | |||
*Distort and compresses adjacent lung | |||
*Empyemas have obtuse angles | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" | | |||
Non-infectious | |||
| style="padding: 5px 5px; background: #F5F5F5;"| | |||
*Granulomatosis with polyangitis | |||
*Rheumatoid nodules | |||
|style="padding: 5px 5px; background: #F5F5F5;"| | |||
*May be single or multiple | |||
*Size ranges from 0.5-7 cm 3,5 | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" | | |||
Vascular | |||
|style="padding: 5px 5px; background: #F5F5F5;"| | |||
*Pulmonary infarct | |||
|style="padding: 5px 5px; background: #F5F5F5;"| | |||
*Consolidation with internal air lucencies, | |||
*"Bubbly consolidation"; this represent non-infarcted aerated lung parenchyma | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" | | |||
Trauma | |||
|style="padding: 5px 5px; background: #F5F5F5;"| | |||
*Pneumatocoeles | |||
|style="padding: 5px 5px; background: #F5F5F5;"| | |||
*Smooth inner margins | |||
*Contain little if any fluid | |||
*Wall (if visible) is thin and regular | |||
*Persist despite absence of symtpoms | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" | Congenital | |||
| style="padding: 5px 5px; background: #F5F5F5;"| | |||
*Congenital cystic adenomatoid malformation (CCAM) | |||
*Pulmonary sequestration | |||
*Bronchogenic cyst | |||
|style="padding: 5px 5px; background: #F5F5F5;"| | |||
*Radiological features vary according to disease | |||
*To learn more about congenital lung cavitations, click in the blue links. | |||
|} | |||
==Imaging Evaluation== | |||
*The evaluation of lung mass will depend on 5 characteristics: calcification patterns, size, location, margins, and attenuation. | |||
'''Calcification''' | '''Calcification''' | ||
Revision as of 14:39, 23 March 2016
|
Lung Mass Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Lung mass imaging On the Web |
|
American Roentgen Ray Society Images of Lung mass imaging |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Maria Fernanda Villarreal, M.D. [2]
Overview
Computed tomography is the method of choice for the evaluation of lung mass. The evaluation of lung mass will depend on several characteristics, such as: calcification, margins, location, distribution, and attenuation. Further evaluation of lung mass, should include other diagnostic studies, such as: bronchoscopy, sputum cytology, or mediastinoscopy. Other imaging study useful for the malignancy evaluation of lung mass is PET scanning, which may be helpful for the detection of occult disease and malignancy assessment.[1]
Imaging
Lung mass can be divided into 2 categories:
- Hyperdense pulmonary mass
- Cavitating pulmonary mass
Hyperdense pulmonary mass
- Hyperdense pulmonary mass is defined as a pulmonary mass with internal calcification
- The most common causes of hyerdense pulmonary mass, include: granuloma (most common), pulmonary hamartoma, bronchogenic carcinoma, carcinoid tumors, and pulmonary metastases.
Cavitating pulmonary mass
- Cavitating pulmonary mass is defined as a gas-filled area of the lung in the center of a nodule, mass or area of consolidation
- It is also characterized by a thick wall (must be greater than 2-5 mm)
- The most common causes of cavitating pulmonary mass, include malignancies, infections, inflammation processes, and congenital malformations.
- The table below summarizes the most common causes of cavitating pulmonary mass
| Cavitating causes | Conditions | Description |
|---|---|---|
| Malignancy |
Cancer
|
Cancer
|
| Infection |
|
Abscess:
Empyema:
|
|
Non-infectious |
|
|
|
Vascular |
|
|
|
Trauma |
|
|
| Congenital |
|
|
Imaging Evaluation
- The evaluation of lung mass will depend on 5 characteristics: calcification patterns, size, location, margins, and attenuation.
Calcification
- Calcification patterns are commonly seen in granulomatous disease and hamartomas
- Calcification patterns are normally a sign of benignancy
- Characteristic benign calcification patterns of lung mass, include:
- Diffuse
- Central
- Laminated
- Popcorn
Size
- Any area of pulmonary opacification that measures more than 30 mm
Location
- Locations of lung mass, include:
- Pleural
- Endobronchial
- Parenchymal
Margins
- Different types of margins for lung mass, include:
- Lobulated or scalloped margins
- Intermediate malignancy probability
- Smooth margins
- Associated with benignancy
Attenuation
- Different types of attenuation for lung mass, include:
- Solid
- Malignancy rate of only 7%
- Calcified
- Partly solid
- Malignancy rate of 63%
- Ground glass
- Malignancy rate of 18%
Plain Radiograph
- On plain radiograph, characteristic findings of lung mass, include:[2]
- Rounded or spiculated mass
- Bulky hilum (representing the tumor and local nodal involvement)
- Lobar collapse
- Cavitation may be seen as an air-fluid level
- Pleural effusion
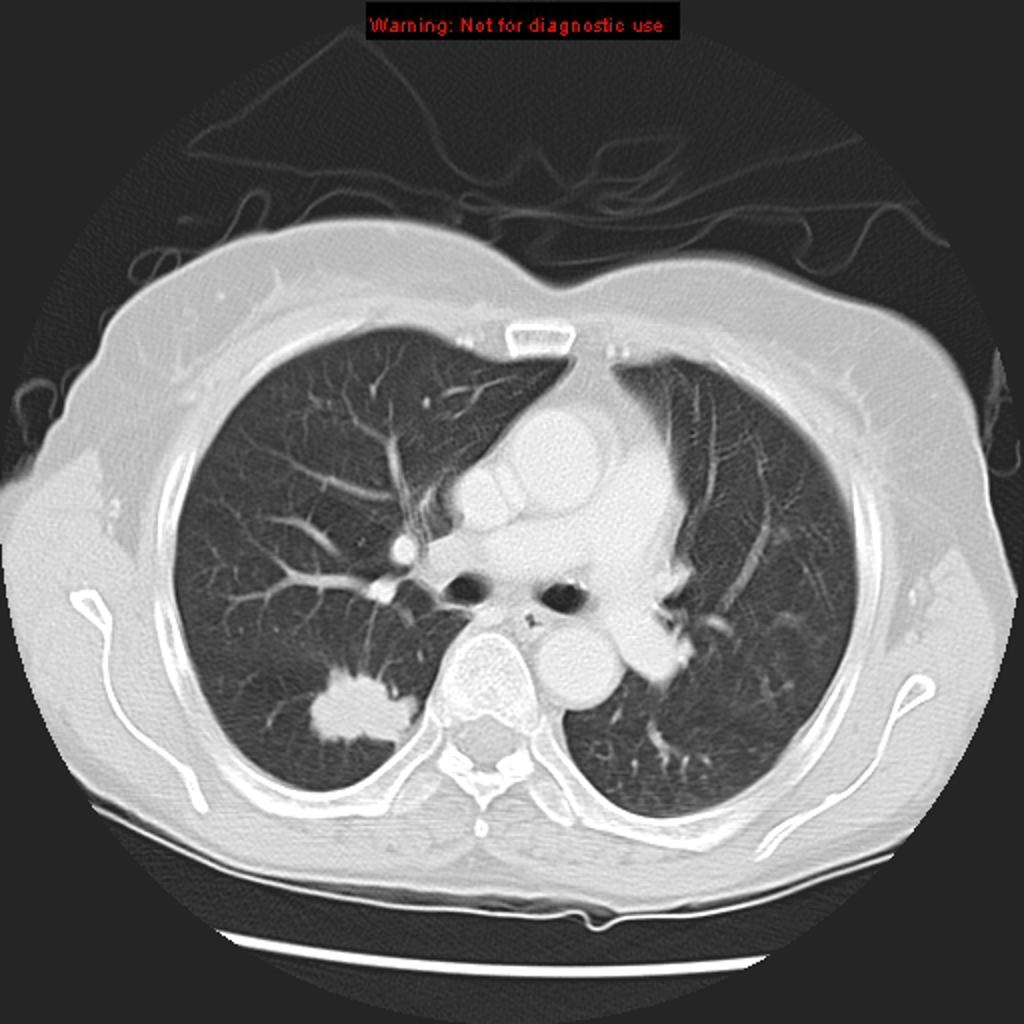
CT
- Computed tomography is the method of choice for the evaluation of lung mass
- On CT scan, characteristic findings of lung mass, include:
- Single pulmonary nodule or mass
- Localized area of parenchymal consolidation
- Bubble-like areas of low attenuation within the mass are a characteristic finding
- Hilar and mediastinal lymphadenopathy is uncommon
- Persistent peripheral consolidation
MRI
- On MRI, there are no characteristic findings of lung mass[3]
- MRI may be helpful for the assessment of mediastinal lymph nodes and diagnose distant metastasis (malignant lung masses)
Gallery
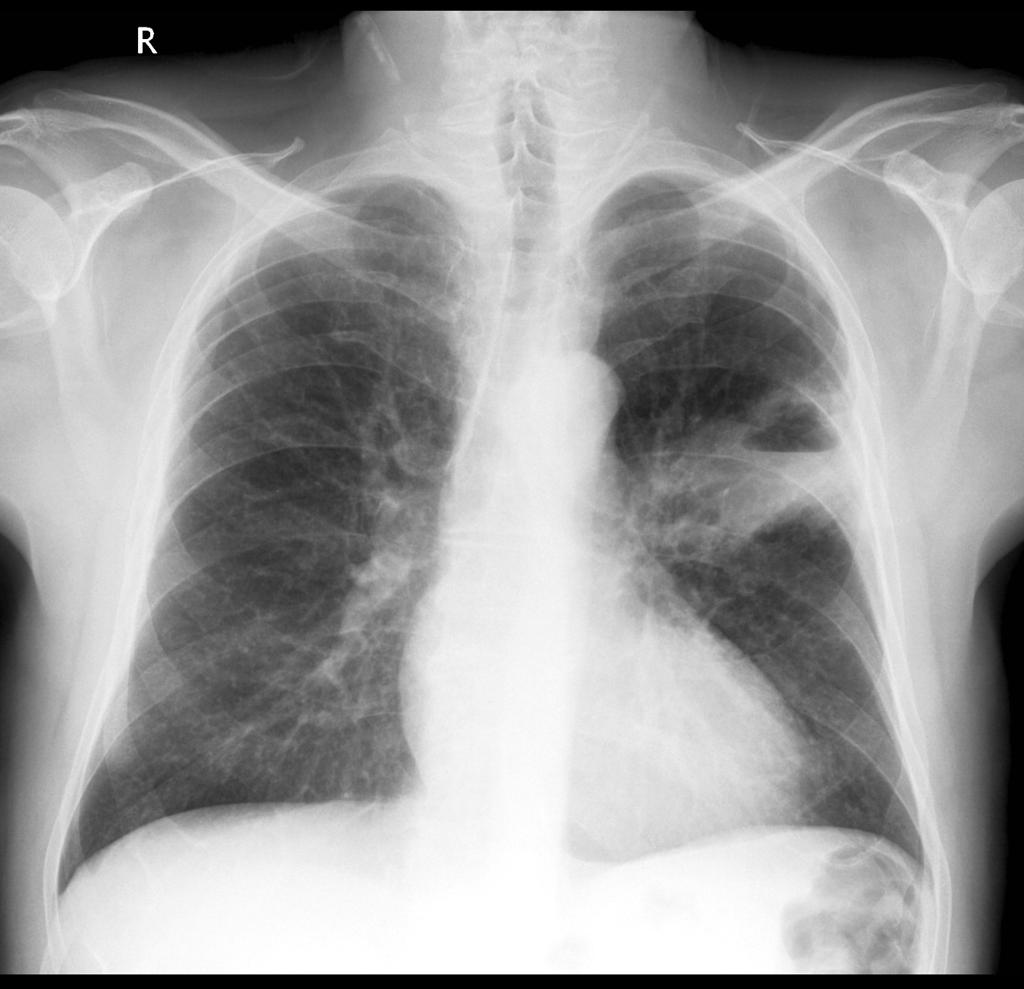
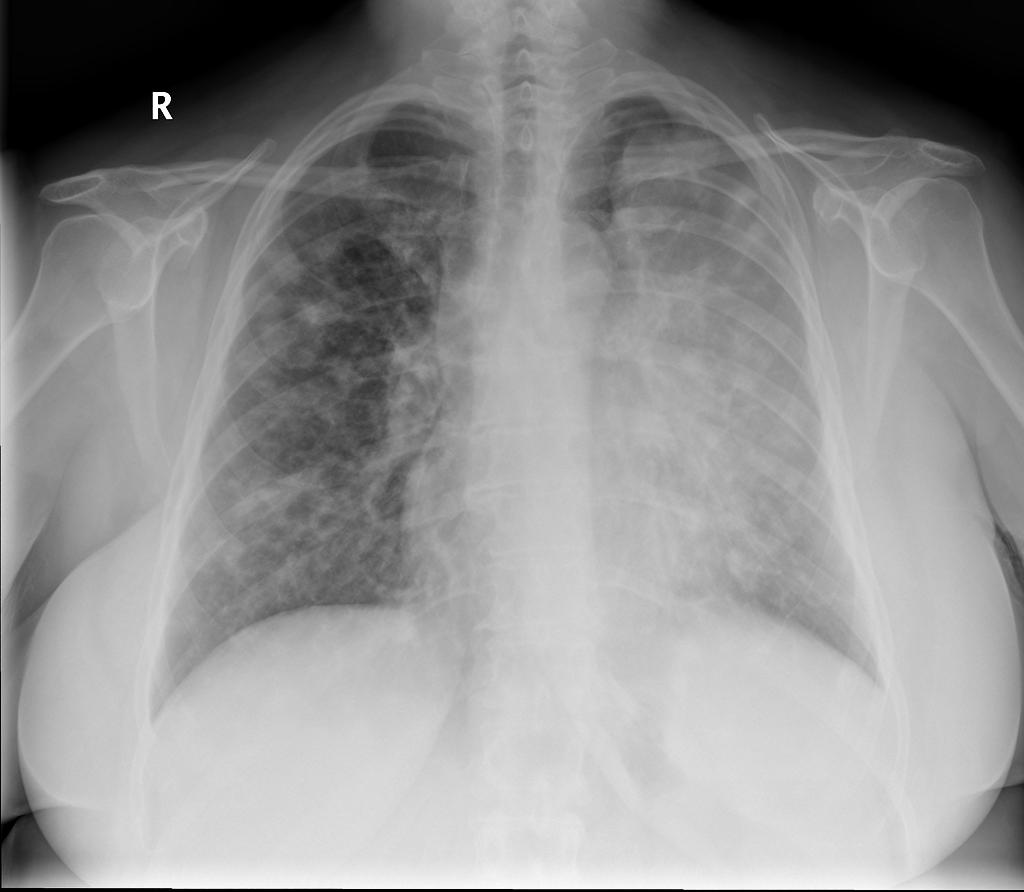
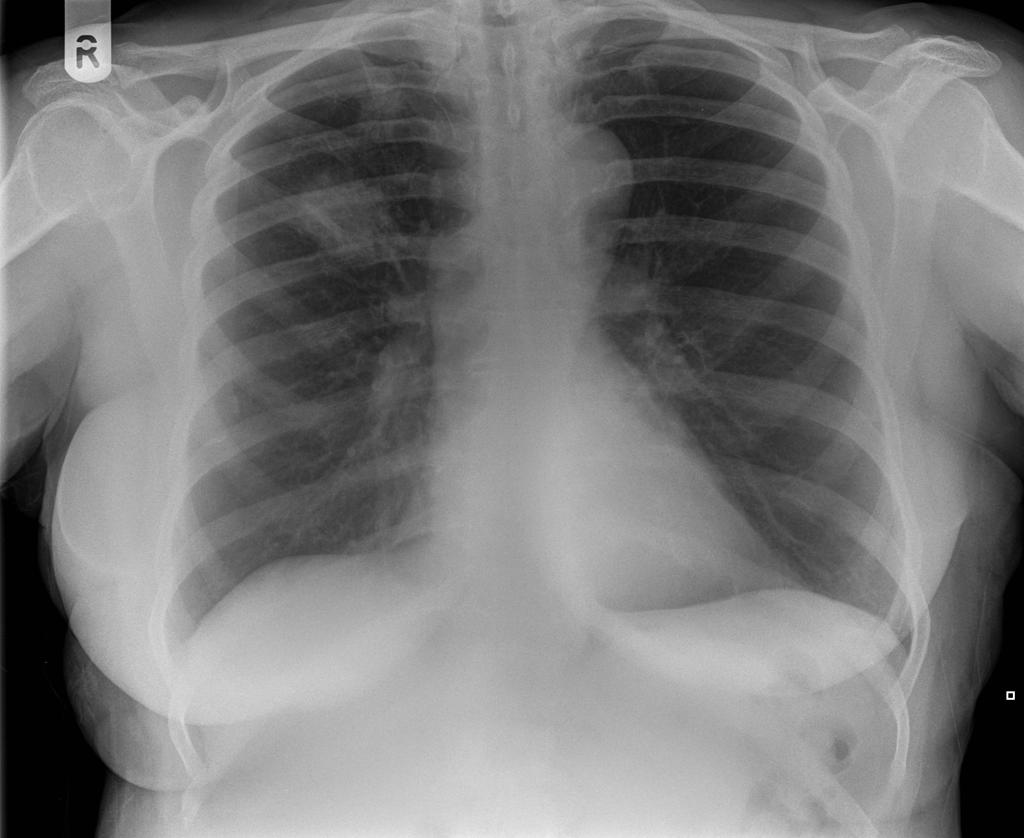
Plain Radiograph
-
Golden "S" Sign (or reverse "S" sign of Golden) : right upper lobar collapse (the right upper lobe appearing dense and shifting medially and upwards, with a central mass expanding the hilum
-
Squameous cell lung cancer: lung cavitating mass left upper lobe adjacent to the oblique fissure. The prominent air-fluid level is best seen on the lateral radiograph
-
Luftsichel sign: curvilinear opacity at the left apex represents compensatory hyperinflation of the left lower lobe
-
Coin lesion sign: round or oval, well-circumscribed lesion, compatible with primary lung cancer
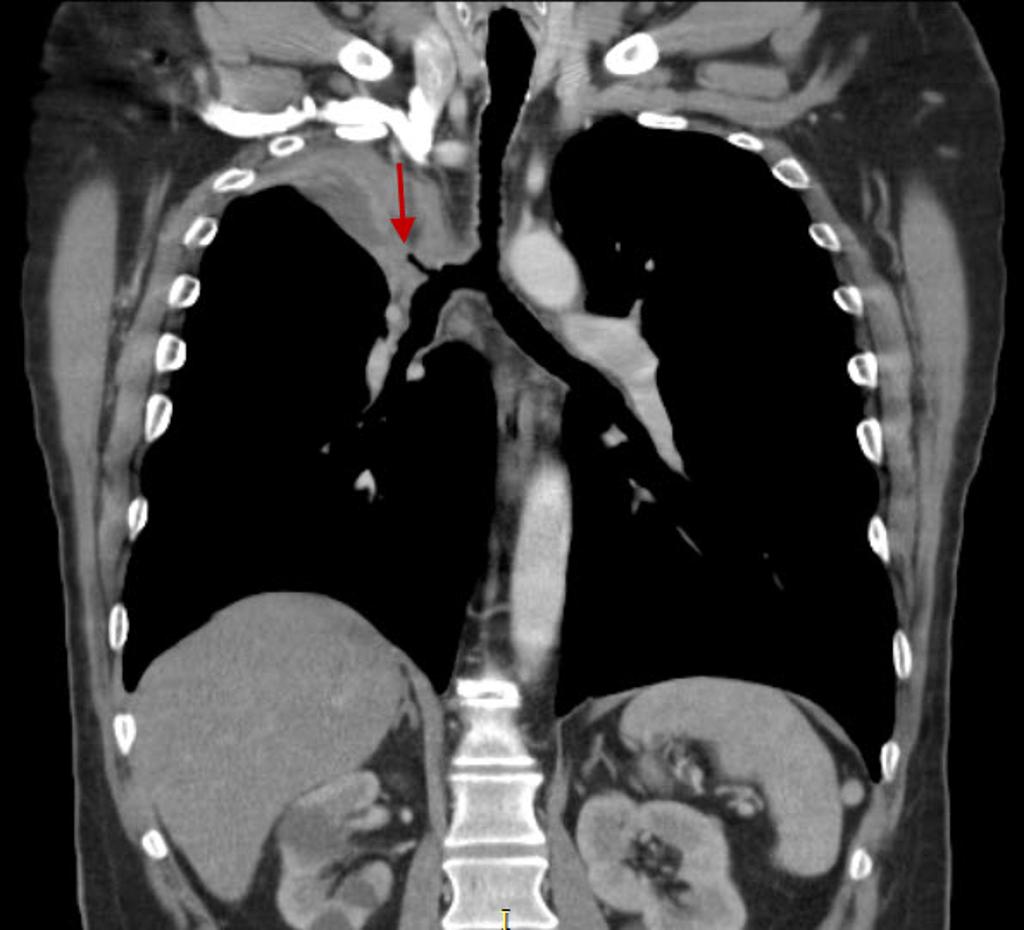
CT
Malignant Lung Mass
-
Bronchogenic lung carcincoma: upper lobe collapse
-
Bronchogenic lung carcincoma: upper lobe with lymphangitic spread
-
Adenocarcinoma of the lung: ground-glass attenuation corresponds to a lepidic growth pattern and the solid component correspond to invasive patterns.
-
Squamous cell lung carcinoma: Peripheral squamous cell lung carcinoma may be seen as a solid nodule/mass with or without an irregular border. The irregular margin can be attributed to a desmoplastic reaction or infiltrative growth
Benign Lung Mass
References
- ↑ Albert RH, Russell JJ (2009). "Evaluation of the solitary pulmonary nodule". Am Fam Physician. 80 (8): 827–31. PMID 19835344.
- ↑ Kundel HL (1981). "Predictive value and threshold detectability of lung tumors". Radiology. 139 (1): 25–9. doi:10.1148/radiology.139.1.7208937. PMID 7208937.
- ↑ Hochhegger B, Marchiori E, Sedlaczek O, Irion K, Heussel CP, Ley S, Ley-Zaporozhan J, Soares Souza A, Kauczor HU (2011). "MRI in lung cancer: a pictorial essay". Br J Radiol. 84 (1003): 661–8. doi:10.1259/bjr/24661484. PMC 3473490. PMID 21697415.