Liver (2)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]

The liver is an organ present in vertebrates and some other animals. It plays a major role in metabolism and has a number of functions in the body, including glycogen storage, plasma protein synthesis, and detoxification. This organ also is the largest gland in the human body. It lies below the diaphragm in the thoracic region of the abdomen.It produces bile, an alkaline compound which aids in digestion, via the emulsification of lipids. It also performs and regulates a wide variety of high-volume biochemical reactions requiring specialized tissues.
Medical terms related to the liver often start in hepato- or hepatic from the Greek word for liver, hēpar (ήπαρ[1]).
Anatomy
The adult human liver normally weighs between 1.4 - 1.6 kilograms (3.1 - 3.5 pounds)[2], and it is a soft, pinkish-brown "boomerang shaped" organ. It is the second largest organ (the largest organ being the skin) and the largest gland within the human body. It is located on the right side of the upper abdomen below the diaphragm. The liver lies on the left of the stomach and makes a kind of bed for the gallbladder (which stores bile).
Flow of blood
The splenic vein, joins the inferior mesenteric vein, which then together join with the superior mesenteric vein to form the portal vein, bringing venous blood from the spleen, pancreas, small intestine, and large intestine, so that the liver can process the nutrients and byproducts of food digestion.
The hepatic veins drain directly into the inferior vena cava.
The hepatic artery is generally a branch from the celiac trunk, although occasionally some or all of the blood can be from other branches such as the superior mesenteric artery.
Approximately 60% to 80% of the blood flow to the liver is from the portal venous system, and 1/4 is from the hepatic artery.
Flow of bile
The bile produced in the liver is collected in bile canaliculi, which merge to form bile ducts.
These eventually drain into the right and left hepatic ducts, which in turn merge to form the common hepatic duct. The cystic duct (from the gallbladder) joins with the common hepatic duct to form the common bile duct.
Bile can either drain directly into the duodenum via the common bile duct or be temporarily stored in the gallbladder via the cystic duct. The common bile duct and the pancreatic duct enter the duodenum together at the ampulla of Vater.
The branchings of the bile ducts resemble those of a tree, and indeed the term "biliary tree" is commonly used in this setting.
Regeneration
The liver is among the few internal human organs capable of natural regeneration of lost tissue; as little as 25% of remaining liver can regenerate into a whole liver again.
This is predominantly due to the hepatocytes acting as unipotential stem cells (i.e. a single hepatocyte can divide into two hepatocyte daughter cells). There is also some evidence of bipotential stem cells, called oval cells, which can differentiate into either hepatocytes or cholangiocytes (cells that line the bile ducts).
Traditional (Surface) anatomy
Peritoneal ligaments
Apart from a patch where it connects to the diaphragm, the liver is covered entirely by visceral peritoneum, a thin, double-layered membrane that reduces friction against other organs. The peritoneum folds back on itself to form the falciform ligament and the right and left triangular ligaments.
These "ligaments" are in no way related to the true anatomic ligaments in joints, and have essentially no functional importance, but they are easily recognizable surface landmarks.
Lobes
Traditional gross anatomy divided the liver into four lobes based on surface features.
The falciform ligament is visible on the front (anterior side) of the liver. This divides the liver into a left anatomical lobe, and a right anatomical lobe.
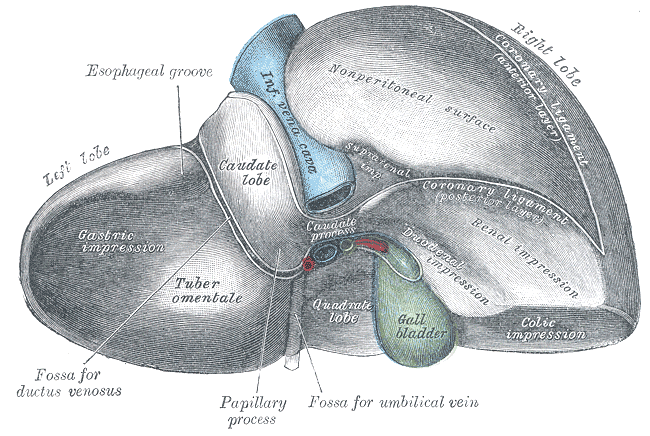
If the liver flipped over, to look at it from behind (the visceral surface), there are two additional lobes between the right and left. These are the caudate lobe (the more superior), and below this the quadrate lobe.
From behind, the lobes are divided up by the ligamentum venosum and ligamentum teres (anything left of these is the left lobe), the transverse fissure (or porta hepatis) divides the caudate from the quadrate lobe, and the right sagittal fossa, which the inferior vena cava runs over, separates these two lobes from the right lobe.
Each of the lobes is made up of lobules, a vein goes from the centre of each lobule which then joins to the hepatic vein to carry blood out from the liver.
On the surface of the lobules there are ducts, veins and arteries that carry fluids to and from them.
Modern (Functional) anatomy
The central area where the common bile duct, portal vein, and hepatic artery enter the liver is the hilum or "porta hepatis". The duct, vein, and artery divide into left and right branches, and the portions of the liver supplied by these branches constitute the functional left and right lobes.
The functional lobes are separated by a plane joining the gallbladder fossa to the inferior vena cava. This separates the liver into the true right and left lobes. The middle hepatic vein also demarcates the true right and left lobes. The right lobe is further divided into an anterior and posterior segment by the right hepatic vein. The left lobe is divided into the medial and lateral segments by the left hepatic vein. The fissure for the ligamentum teres (the ligamentum teres becomes the falciform ligament) also separates the medial and lateral segmants. The medial segment is what used to be called the quadrate lobe. In the widely used Couinaud or "French" system, the functional lobes are further divided into a total of eight subsegments based on a transverse plane through the bifurcation of the main portal vein. The caudate lobe is a separate structure which receives blood flow from both the right- and left-sided vascular branches.[3][4] The subsegments corresponding to the anatomical lobes are as follows:
| Segment* | Couinaud segments |
|---|---|
| Caudate | 1 |
| Lateral | 2, 3 |
| Medial | 4a, 4b |
| Right | 5, 6, 7, 8 |
- or lobe in the Caudate's case.
Each number in the list corresponds to one in the table.
- Caudate
- Superior subsegment of the lateral segment
- Inferior subsegment of the lateral segment
- Superior subsegment of the medial segment
- Inferior subsegment of the medial segment
- Inferior subsegment of the anterior segment
- Inferior subsegment of the posterior segment
- Superior subsegment of the posterior segment
- Superior subsegment of the anterior segment
Physiology
The various functions of the liver are carried out by the liver cells or hepatocytes.
- The liver produces and excretes bile (a greenish liquid) required for emulsifying fats. Some of the bile drains directly into the duodenum, and some is stored in the gallbladder.
- The liver performs several roles in carbohydrate metabolism:
- Gluconeogenesis (the synthesis of glucose from certain amino acids, lactate or glycerol)
- Glycogenolysis (the breakdown of glycogen into glucose) (muscle tissues can also do this)
- Glycogenesis (the formation of glycogen from glucose)
- The breakdown of insulin and other hormones
- The liver is responsible for the mainstay of protein metabolism.
- The liver also performs several roles in lipid metabolism:
- Cholesterol synthesis
- The production of triglycerides (fats).
- The liver produces coagulation factors I (fibrinogen), II (prothrombin), V, VII, IX, X and XI, as well as protein C, protein S and antithrombin.
- The liver breaks down haemoglobin, creating metabolites that are added to bile as pigment (bilirubin and biliverdin).
- The liver breaks down toxic substances and most medicinal products in a process called drug metabolism. This sometimes results in toxication, when the metabolite is more toxic than its precursor.
- The liver converts ammonia to urea.
- The liver stores a multitude of substances, including glucose in the form of glycogen, vitamin B12, iron, and copper.
- In the first trimester fetus, the liver is the main site of red blood cell production. By the 32nd week of gestation, the bone marrow has almost completely taken over that task.
- The liver is responsible for immunological effects- the reticuloendothelial system of the liver contains many immunologically active cells, acting as a 'sieve' for antigens carried to it via the portal system.
Currently, there is no artificial organ or device capable of emulating all the functions of the liver. Some functions can be emulated by liver dialysis, an experimental treatment for liver failure.
Diseases of the liver
Many diseases of the liver are accompanied by jaundice caused by increased levels of bilirubin in the system. The bilirubin results from the breakup of the hemoglobin of dead red blood cells; normally, the liver removes bilirubin from the blood and excretes it through bile.
- Hepatitis, inflammation of the liver, caused mainly by various viruses but also by some poisons, autoimmunity or hereditary conditions.
- Cirrhosis is the formation of fibrous tissue in the liver, replacing dead liver cells. The death of the liver cells can for example be caused by viral hepatitis, alcoholism or contact with other liver-toxic chemicals.
- Haemochromatosis, a hereditary disease causing the accumulation of iron in the body, eventually leading to liver damage.
- Cancer of the liver (primary hepatocellular carcinoma or cholangiocarcinoma and metastatic cancers, usually from other parts of the gastrointestinal tract).
- Wilson's disease, a hereditary disease which causes the body to retain copper.
- Primary sclerosing cholangitis, an inflammatory disease of the bile duct, autoimmune in nature.
- Primary biliary cirrhosis, autoimmune disease of small bile ducts.
- Budd-Chiari syndrome, obstruction of the hepatic vein.
- Gilbert's syndrome, a genetic disorder of bilirubin metabolism, found in about 5% of the population.
- Glycogen storage disease type II,The build-up of glycogen causes progressive muscle weakness (myopathy) throughout the body and affects various body tissues, particularly in the heart, skeletal muscles, liver and nervous system.
There are also many pediatric liver disease, including biliary atresia, alpha-1 antitrypsin deficiency, alagille syndrome, and progressive familial intrahepatic cholestasis, to name but a few.
A number of liver function tests are available to test the proper function of the liver. These test for the presence of enzymes in blood that are normally most abundant in liver tissue, metabolites or products.
Liver transplantation
Human liver transplant was first performed by Thomas Starzl in USA and Roy Calne in England in 1963 and 1965 respectively.
Liver transplantation is the only option for those with irreversible liver failure. Most transplants are done for chronic liver diseases leading to cirrhosis, such as chronic hepatitis C, alcoholism, autoimmune hepatitis, and many others. Less commonly, liver transplantation is done for fulminant hepatic failure, in which liver failure occurs over days to weeks.
Liver allografts for transplant usually come from non-living donors who have died from fatal brain injury. Living donor liver transplantation is a technique in which a portion of a living person's liver is removed and used to replace the entire liver of the recipient. This was first performed in 1989 for pediatric liver transplantation. Only 20% of an adult's liver (Couinaud segments 2 and 3) is needed to serve as a liver allograft for an infant or small child.
More recently, adult-to-adult liver transplantation has been done using the donor's right hepatic lobe which amounts to 60% of the liver. Due to the ability of the liver to regenerate, both the donor and recipient end up with normal liver function if all goes well. This procedure is more controversial as it entails performing a much larger operation on the donor, and indeed there have been at least 2 donor deaths out of the first several hundred cases. A recent publication has addressed the problem of donor mortality, and at least 14 cases have been found.[5] The risk of postoperative complications (and death) is far greater in right sided hepatectomy than left sided operations.
Development
The liver develops as an endodermal outpocketing of the foregut called the hepatic diverticulum. Its initial blood supply is primarily from the vitelline veins that drain blood from the yolk sac. The superior part of the hepatic diverticulum gives rise to the hepatocytes and bile ducts, while the inferior part becomes the gallbladder and its associated cystic duct.
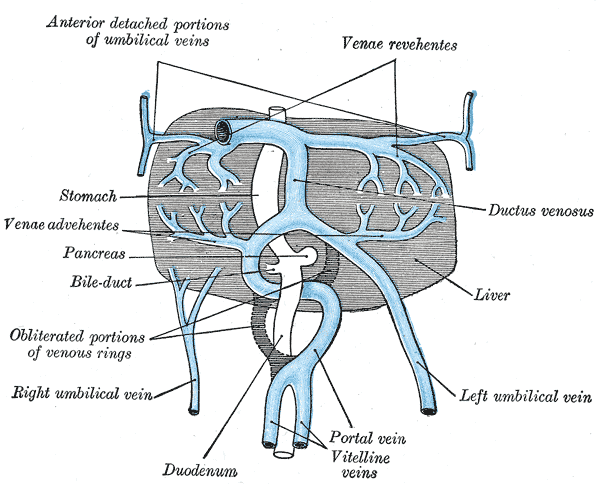
Fetal blood supply
In the growing fetus, a major source of blood to the liver is the umbilical vein which supplies nutrients to the growing fetus. The umbilical vein enters the abdomen at the umbilicus, and passes upward along the free margin of the falciform ligament of the liver to the inferior surface of the liver. There it joins with the left branch of the portal vein. The ductus venosus carries blood from the left portal vein to the left hepatic vein and then to the inferior vena cava, allowing placental blood to bypass the liver.
In the fetus, the liver develops throughout normal gestation, and does not perform the normal filtration of the infant liver. The liver does not perform digestive processes because the fetus does not consume meals directly, but receives nourishment from the mother via the placenta. The fetal liver releases some blood stem cells that migrate to the fetal thymus, so initially the lymphocytes, called T-cells, are created from fetal liver stem cells. Once the fetus is delivered, the formation of blood stem cells in infants shifts to the red bone marrow.
After birth, the umbilical vein and ductus venosus are completely obliterated two to five days postpartum; the former becomes the ligamentum teres and the latter becomes the ligamentum venosum. In the disease state of cirrhosis and portal hypertension, the umbilical vein can open up again.
Further reading
- The following are standard medical textbooks:
- Eugene R. Schiff, Michael F. Sorrell, Willis C. Maddrey, eds. Schiff's diseases of the liver, 9th ed. Philadelphia : Lippincott, Williams & Wilkins, 2003. ISBN 0-7817-3007-4
- Sheila Sherlock, James Dooley. Diseases of the liver and biliary system, 11th ed. Oxford, UK ; Malden, MA : Blackwell Science. 2002. ISBN 0-632-05582-0
- David Zakim, Thomas D. Boyer. eds. Hepatology: a textbook of liver disease, 4th ed. Philadelphia: Saunders. 2003. ISBN 0-7216-9051-3
- These are for the lay reader or patient:
- Sanjiv Chopra. The Liver Book: A Comprehensive Guide to Diagnosis, Treatment, and Recovery, Atria, 2002, ISBN 0-7434-0585-4
- Melissa Palmer. Dr. Melissa Palmer's Guide to Hepatitis and Liver Disease: What You Need to Know, Avery Publishing Group; Revised edition May 24, 2004, ISBN 1-58333-188-3. her webpage.
- Howard J. Worman. The Liver Disorders Sourcebook, McGraw-Hill, 1999, ISBN 0-7373-0090-6. his Columbia University web site, "Diseases of the liver"
See also
References
- ↑ The Greek word "ήπαρ" was derived from hēpaomai (ηπάομαι): to mend, to repair, hence hēpar actually means "repairable", indicating that this organ can regenerate itself spontaneously in the case of lesion.
- ↑ Robbins and Cotran Pathologic Basis of Disease, 7th Edition, p. 878
- ↑ http://dpi.radiology.uiowa.edu/nlm/app/livertoc/liver/liver.html
- ↑ http://www.uni-bonn.de/~umm705/quiz0403.htm
- ↑ Bramstedt K (2006). "Living liver donor mortality: where do we stand?". Am J Gastroenterol. 101 (4): 755–9. PMID 16494593.
Additional images
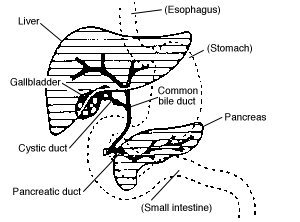
-
Accessory digestive system.
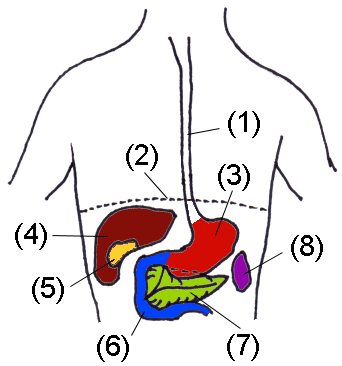
-
Digestive organs.
-
The liver and the veins in connection with it, of a human embryo, twenty-four or twenty-five days old, as seen from the ventral surface.
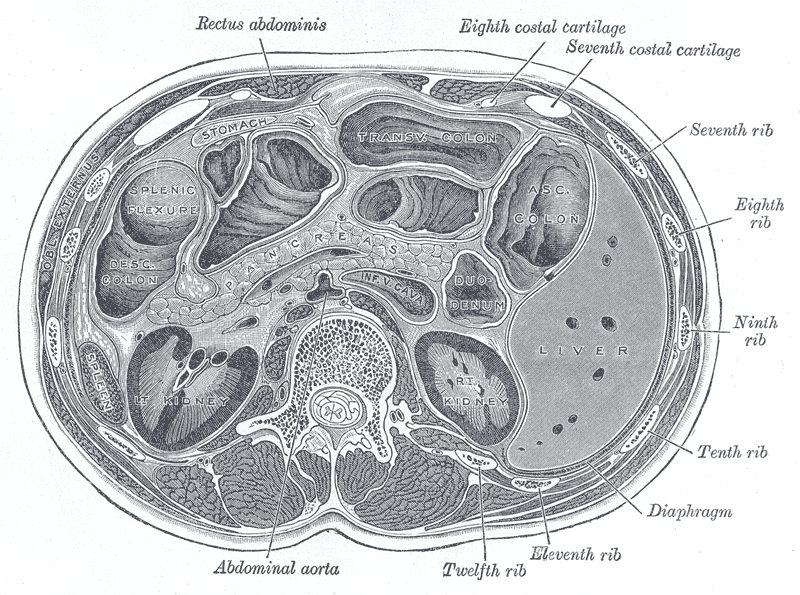
-
Transverse section through the middle of the first lumbar vertebra, showing the relations of the pancreas.
-
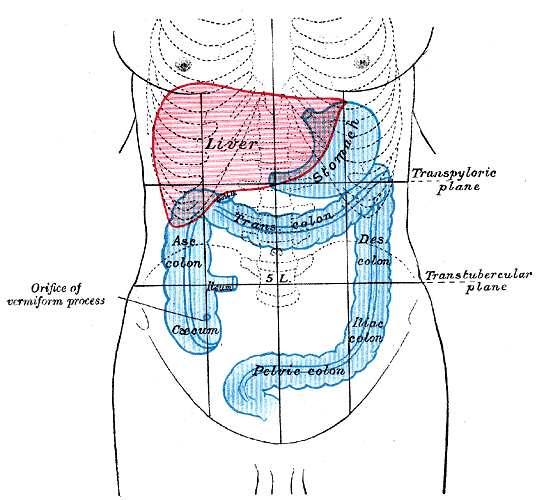
Front of abdomen, showing surface markings for liver, stomach, and great intestine
-
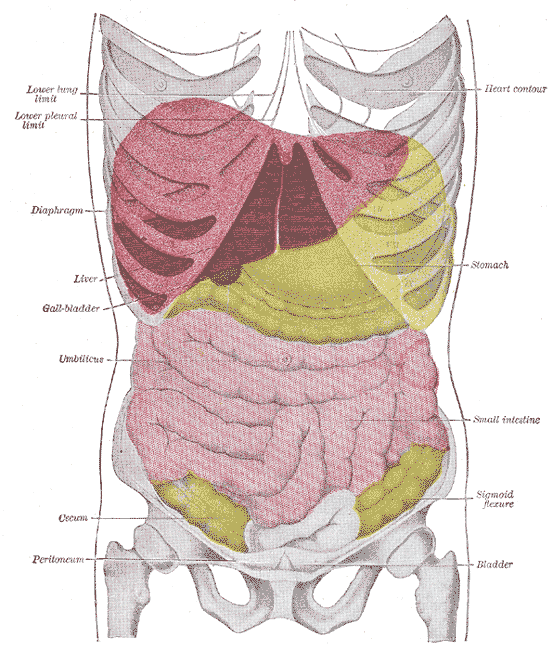
Topography of thoracic and abdominal viscera.
-
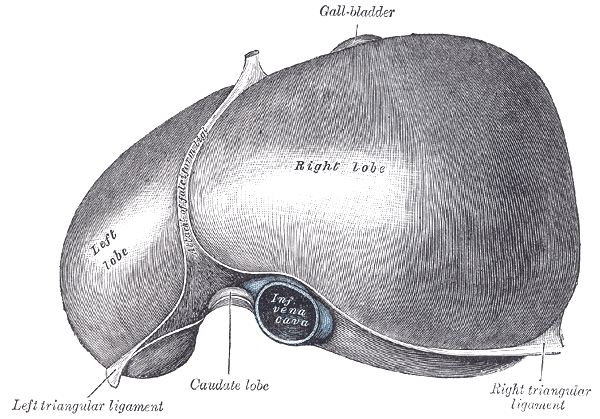
Frontal view from Gray's Anatomy (1918)
-
Back view from Gray's Anatomy (1918)
External links
- Children's Liver Association for Support Services, C.L.A.S.S. A large non-profit organization. An online Support Group full of resources, materials and stories; includes a Community Discussion Forum and Chat Room
- The American Liver Foundation
- American Association for the Study of Liver Diseases (AASLD)
- American Liver Society (ALS)
- WikiLiver — a wiki dedicated to the liver
- "It's Dangerous to Ignore Your Liver" — information provided by the American Liver Foundation
- "The Liver and its Diseases" — information at h2g2
- Liver Families — an online support group for families whose lives have been affected by pediatric liver disease and transplant issues
- Children's Liver Disease Foundation — an organisation dedicated to fighting childhood liver disease and supporting affected families
- Liver Specialists of Texas: a site designed for patients with liver disease, located in Houston, Texas USA
- Autoimmune immune liver disease
- British Liver Trust - includes patient info oriented to British situations.