Left ventricular aneurysm: Difference between revisions
(/* ACC/AHA Guidelines (DO NOT EDIT){{cite journal |author=Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Fa...) |
(/* 2004 ACC/AHA Guidelines for the management of patients with ST-Elevation Myocardial Infarction (DO NOT EDIT){{cite journal |author=Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mull...) |
||
| Line 62: | Line 62: | ||
==2004 ACC/AHA Guidelines for the management of patients with ST-Elevation Myocardial Infarction (DO NOT EDIT)<ref name="pmid15339869">{{cite journal |author=Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK |title=ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) |journal=Circulation |volume=110 |issue=9 |pages=e82–292 |year=2004 |month=August |pmid=15339869 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=15339869}}</ref>== | ==2004 ACC/AHA Guidelines for the management of patients with ST-Elevation Myocardial Infarction (DO NOT EDIT)<ref name="pmid15339869">{{cite journal |author=Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK |title=ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) |journal=Circulation |volume=110 |issue=9 |pages=e82–292 |year=2004 |month=August |pmid=15339869 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=15339869}}</ref>== | ||
{ | {| class="wikitable" | ||
== | |- | ||
| colspan="1" style="text-align:center; background:LemonChiffon"| [[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
1. It is reasonable that patients with [[STEMI]] who develop a ventricular aneurysm associated with intractable [[ventricular tachyarrhythmia]]s and/or [[pump failure]] unresponsive to medical and catheterbased therapy be considered for [[LV]] aneurysmectomy and [[CABG]] surgery. ''(Level of Evidence: B)'' | |- | ||
| bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''1.''' It is reasonable that patients with [[STEMI]] who develop a ventricular aneurysm associated with intractable [[ventricular tachyarrhythmia]]s and/or [[pump failure]] unresponsive to medical and catheterbased therapy be considered for [[LV]] aneurysmectomy and [[CABG]] surgery. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B]])''<nowiki>"</nowiki> | |||
|} | |||
==Sources== | ==Sources== | ||
Revision as of 22:58, 20 January 2013
| Left ventricular aneurysm | |
 |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Left ventricular aneurysm (LVA) is a sequela to myocardial infarction which occurrs in 10% to 30% of patients surviving an acute myocardial infarction.
Classification
Left ventricular aneurysms are classified as true and false aneurysms. While both true aneurysms and false (pseudo) ventricular aneurysms are the sequelae of myocardial infarction, their etiology, pathologic findings, diagnostic findings, and treatment are different.
True Left Ventricular Aneurysm
A true left ventricular aneurysm has an aneurysmal sac which contains the endocardium, epicardium, and thinned fibrous tissue (scar) that is a remnant of the left ventricular muscle. A true left ventricular aneurysm, particularly if small, may cause few or any symptoms and is compatible with prolonged survival. Rupture of a true aneurysm is relatively uncommon. Surgical resection is therefore only necessary when refractory angina pectoris, congestive heart failure, systemic embolization, or refractory arrhythmias are present.
False Left Ventricular Aneurysm or Pseudoaneurysm
Unlike a true aneurysm, which contains some myocardial elements in its wall, the walls of a false aneurysm are composed of organized hematoma and pericardium and lack any element of the original myocardial wall. A false aneurysmal sac represents a pericardium that contains a ruptured left ventricle. In contrast to true aneurysms, false aneurysms have a greater tendency to rupture and require surgical repair.
Pathophysiology
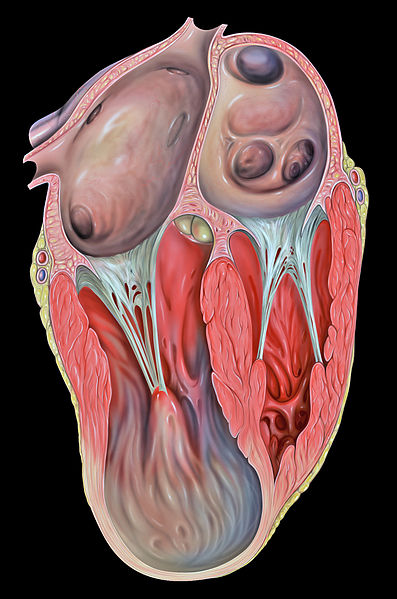
Gross Pathology
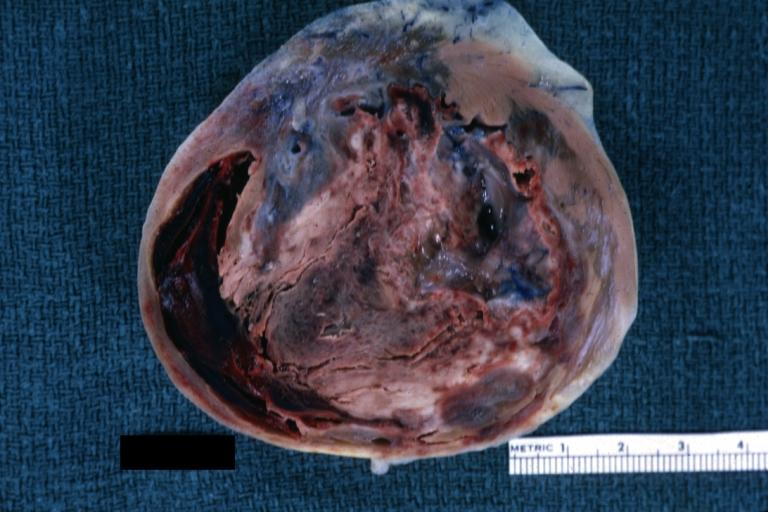
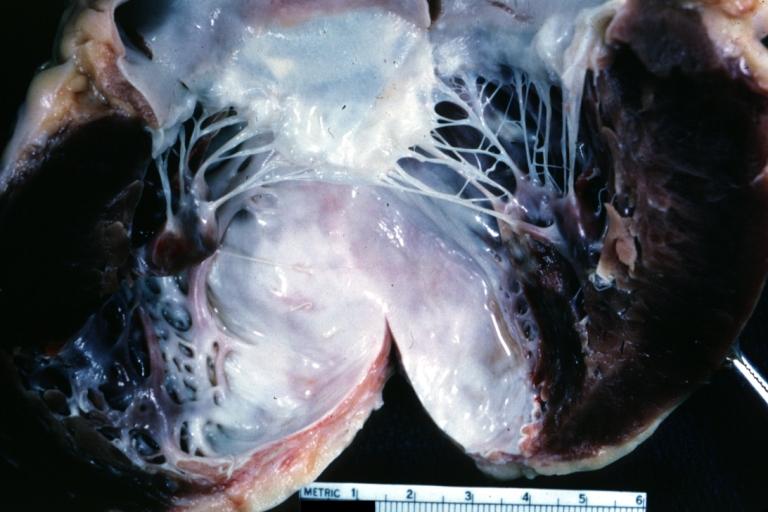
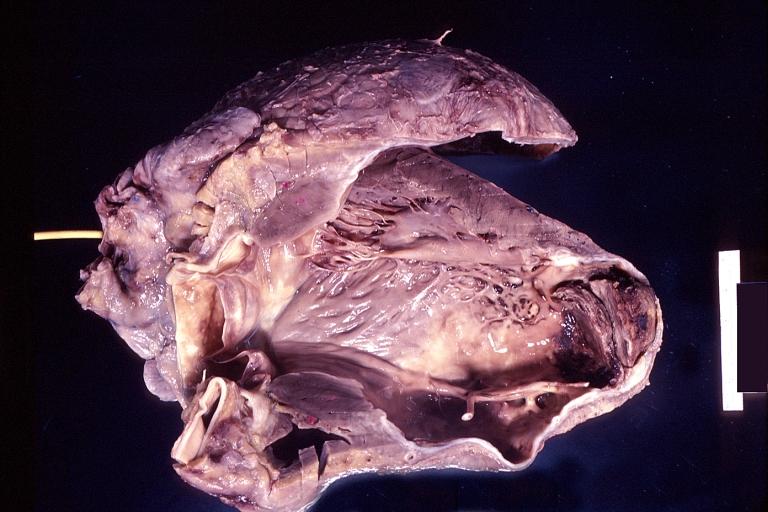
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Left ventricular aneurysm
-
Left Ventricle Aneurysm: Gross natural color horizontal section apex of left ventricle with aneurysmal dilation and mural thrombus. A large scar tissue in myocardium.
-
Left ventricular aneurysm.
-
Heart; old myocardial infarction with aneurysm formation
Diagnosis
Electrocardiogram
Shown below is an example of an EKG of a person with a left ventricular aneurysm. Note the ST elevation in the anterior leads.
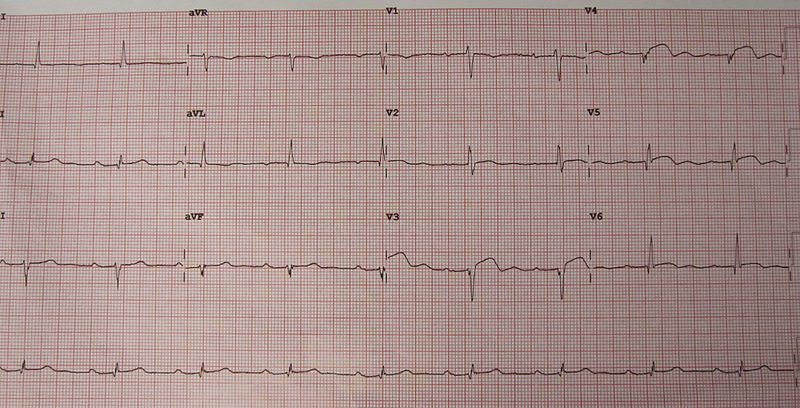
True aneurysms distort the shape of the left ventricle during both diastole and systole, and the motion of the aneurysmal segment is paradoxical. This can be associated with ST changes including ST elevation, particularly at high heart rates as might be encountered during exercise.
Imaging
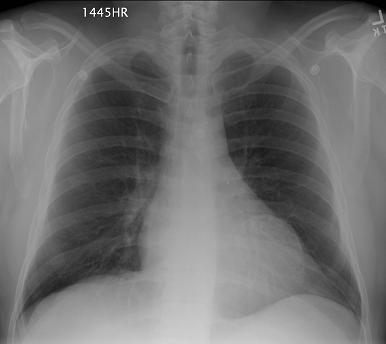
(Radiological Images Courtesy of RadsWiki)
Chest X Ray
The presence of a discrete bulge in the heart anteriorly is suggestive of a true aneurysm.
-
Calcified left ventricular aneurysm
-
Calcified left ventricular aneurysm
-
Ventricular aneurysm
Chest CT Scan
- True aneurysms will often have a wide neck and are often apical in location.
- False aneurysms will often have a narrow neck and are often posterior diaphragmatic in loccation.
-
Calcified left ventricular aneurysm
-
Calcified left ventricular aneurysm
-
Calcified left ventricular aneurysm
2004 ACC/AHA Guidelines for the management of patients with ST-Elevation Myocardial Infarction (DO NOT EDIT)[1]
| Class IIa |
| "1. It is reasonable that patients with STEMI who develop a ventricular aneurysm associated with intractable ventricular tachyarrhythmias and/or pump failure unresponsive to medical and catheterbased therapy be considered for LV aneurysmectomy and CABG surgery. (Level of Evidence: B)" |
Sources
- The 2004 ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction [1]
- The 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction [2]
References
- ↑ 1.0 1.1 Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK (2004). "ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction)". Circulation. 110 (9): e82–292. PMID 15339869. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Hand M, Armstrong PW; et al. (2008). "2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee". Circulation. 117 (2): 296–329. doi:10.1161/CIRCULATIONAHA.107.188209. PMID 18071078. Unknown parameter
|month=ignored (help)