Laryngeal cancer pathophysiology
|
Laryngeal cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Laryngeal cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Laryngeal cancer pathophysiology |
|
Risk calculators and risk factors for Laryngeal cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Faizan Sheraz, M.D. [2]
Overview
Hypopharyngeal cancer arises from squamous cells, which are cells that are normally involved in protection of aerodigestive tract. Genes involved in the pathogenesis of hypopharyngeal cancer include p16, NOTCH1, cyclin D1, and TP53. Hypopharyngeal cancer is associated with sideropenic dysphagia and Paterson Brown Kelly syndrome. On gross pathology, flattened plaques, mucosal ulceration, and raised margins of the lesion are characteristic findings of hypopharyngeal cancer. On microscopic histopathological analysis, spindle cells, basaloid cells, and nuclear atypia are characteristic findings of hypopharyngeal cancer.[1]
Pathophysiology
Hypopharyngeal cancer arises from squamous cells, which are cells that are normally involved in protection of aerodigestive tract. Development of hypopharyngeal cancer is the result of multiple genetic mutations. These mutations lead to activation of oncogenes and inactivation of tumor suppression genes which ultimately results in deregulated cellular proliferation.
Genetics
Genes involved in the pathogenesis of hypopharyngeal cancer include:
Associated Diseases
Hypopharyngeal carcinoma is associated with:[1]
Gross Pathology
On gross pathology, hypopharyngeal cancer is characterized by:[1]
- Flattened plaques
- Raised margins of the lesion
- Mucosal ulceration
- Tumor spread to piriform sinus
Microscopic Pathology
On microscopic histopathological analysis, hypopharyngeal carcinoma is characterized by:[1]
- Spindle cells
- Basaloid cells
- Nuclear atypia
- Abundant chromatin
Overview
Pathophysiology
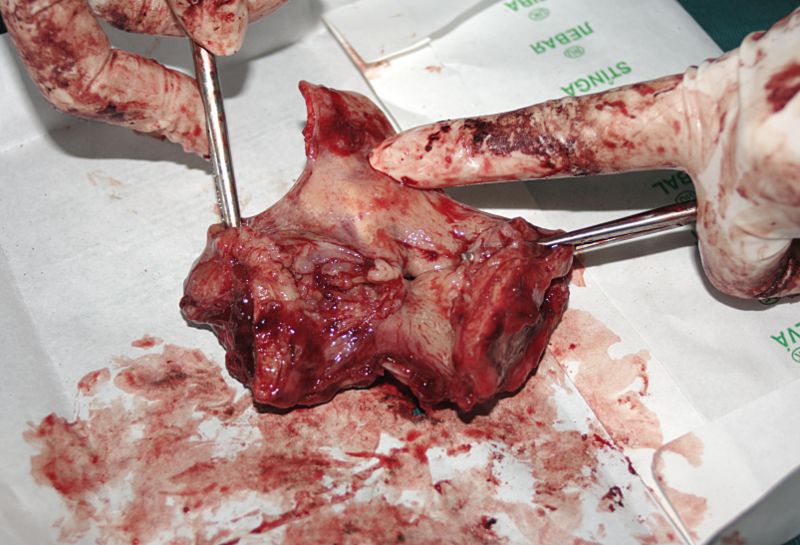
Gross Pathology
-
Gross pathology specimen of laryngeal cancer
Subclassification by site
It is generally divided the following way:[2]
| Laryngeal cancer | |||||||||||||||||||||||||||||||||
| Supraglottis | Glottis | Subglottis | |||||||||||||||||||||||||||||||
- Prevalence - glottis > supraglottis > subglottis.
- Glottic carcinoma tends to present earlier (as it affects phonation) and, therefore, has a better prognosis.
SCC is subdivided by the WHO into:[5]
- Keratinizing type (KT).
- Worst prognosis.
- Undifferentiated type (UT).
- Intermediate prognosis.
- EBV association.
- Nonkeratinizing type (NT).
- Good prognosis.
- EBV association.
Microscopic
Features based on classification:[5]
- KT subtype:
- Keratinization & intercellular bridges through-out most of the malignant lesion.
- UT:
- Non-distinct borders/syncytial pattern.
- Nucleoli.
- NT:
- Well-defined cell borders.
Invasion
Features:
- Eosinophilia.
- Extra large nuclei/bizarre nuclei.
- Inflammation (lymphocytes, plasma cells).
- Long rete ridges.
- Numerous beeds/blobs of epithelial cells that seem unlikely to be rete ridges.
Pitfalls:
- Tangential cuts.
- If you can trace the squamous cells from a gland to the surface it is less likely to be invasive cancer.
Notes on invasion:
- Nice review paper by Wenig.[6]
- See SCC of the cervix versus CIN III.
Images
-
Laryngeal squamous carcinoma (Intermediate Magnification)[7]
-
Laryngeal squamous carcinoma (High Magnification)[7]
-
Laryngeal squamous carcinoma (Very High Magnification)[7]
Overview of subtypes
There are several subtypes:[8]
- Basaloid - poor prognosis, usu. diagnosed by recognition of typical SCC.
- Warty (Condylomatous).
- Verrucous - good prognosis, rare.
- Papillary.
- Lymphoepithelial, rare.
- Spindle cell, a common spindle cell lesion of the H&N.
Verrucous squamous cell carcinoma
Features:
- Exophytic growth.
- Well-differentiated.
- "Glassy" appearance.
- Pushing border.
DDx: papilloma.
Spindle cell squamous carcinoma
- Key to diagnosis is finding a component of conventional squamous cell carcinoma.
IHC:
- Typically keratin -ve.
- p63 +ve.
DDx:
- Spindle cell melanoma.
- Mesenchymal neoplasm.
Basaloid squamous cell carcinoma
- May mimic adenoid cystic carcinoma.
- Classically base of tongue.[9]
- Typically poor prognosis.
Features:
- Need keratinization. (???)
DDx:
- Neuroendocrine tumour.
Lymphoepithelial (squamous cell) carcinoma
IHC
- p63 +ve.
- EBER -ve.
- Positive suggests nasopharyngeal carcinoma.
- p16 -ve.
- Positive suggests HPV-associated head and neck squamous cell carcinoma.
- Bcl2 +ve/-ve.
- Positive = poor prognosis.[10]
References
- ↑ 1.0 1.1 1.2 1.3 Helliwell TR (2003). "acp Best Practice No 169. Evidence based pathology: squamous carcinoma of the hypopharynx". J Clin Pathol. 56 (2): 81–5. PMC 1769882. PMID 12560383.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Larynx_11protocol.pdf. Accessed on: 2 May 2012.
- ↑ Template:Ref WMSP
- ↑ URL: http://www.health.am/cr/more/statistics-and-prognosis-for-cancer-of-the-larynx/. Accessed on: 2 May 2012.
- ↑ 5.0 5.1 Template:Ref Sternberg4
- ↑ Wenig BM (2002). "Squamous cell carcinoma of the upper aerodigestive tract: precursors and problematic variants" (PDF). Mod. Pathol. 15 (3): 229–54. doi:10.1038/modpathol.3880520. PMID 11904340. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 7.2 Head and neck SCC Librepathology. http://librepathology.org/wiki/index.php/Squamous_cell_carcinoma_of_the_head_and_neck Accessed on October 26, 2015
- ↑ URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970297-2. Accessed on: March 9, 2010.
- ↑ URL: http://www.biomedcentral.com/1471-2407/6/146. Accessed on: March 9, 2010.
- ↑ Nichols AC, Finkelstein DM, Faquin WC; et al. (2010). "Bcl2 and human papilloma virus 16 as predictors of outcome following concurrent chemoradiation for advanced oropharyngeal cancer". Clin. Cancer Res. 16 (7): 2138–46. doi:10.1158/1078-0432.CCR-09-3185. PMID 20233885. Unknown parameter
|month=ignored (help)
![Laryngeal squamous carcinoma (Intermediate Magnification)[7]](/images/c/ca/800px-Laryngeal_squamous_carcinoma_--_intermed_mag.jpg)
![Laryngeal squamous carcinoma (High Magnification)[7]](/images/e/e3/800px-Laryngeal_squamous_carcinoma_--_high_mag.jpg)
![Laryngeal squamous carcinoma (Very High Magnification)[7]](/images/f/f5/800px-Laryngeal_squamous_carcinoma_--_very_high_mag.jpg)