Hypocalcemia
For patient information, click here
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Hypocalcemia |
|
Articles |
|---|
|
Most recent articles on Hypocalcemia Most cited articles on Hypocalcemia |
|
Media |
|
Powerpoint slides on Hypocalcemia |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Hypocalcemia at Clinical Trials.gov Clinical Trials on Hypocalcemia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Hypocalcemia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Hypocalcemia Discussion groups on Hypocalcemia Patient Handouts on Hypocalcemia Directions to Hospitals Treating Hypocalcemia Risk calculators and risk factors for Hypocalcemia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Hypocalcemia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Hypocalcemia is the presence of low serum calcium levels in the blood, usually taken as less than 3.5 mmol/L or 8.8 mg/dl or an ionized calcium level of less than 1.1 mmol/L (4.5 mg/dL). It is a type of electrolyte disturbance. In the blood, about half of all calcium is bound to proteins such as serum albumin, but it is the unbound, or ionized, calcium that the body regulates. If a person has abnormal levels of blood proteins then the plasma calcium may be inaccurate. The ionized calcium level is considered more clinically accurate in this case.
Calcium is the most abundant mineral in the body. 99% of the body's calcium is stored in bone. Calcium is found in plasma and is either protein-bound or ionized and readily available.
Alkalosis
As blood plasma hydrogen ion concentration decreases, caused by respiratory or metabolic alkalosis, freely ionized calcium concentration decreases. This freely ionized calcium is the biologically active component of blood calcium. Since a portion of both hydrogen ions and calcium are bound to serum albumin, when blood becomes alkalotic, bound hydrogen ions dissociate from albumin, freeing up the albumin to bind with more calcium and thereby decreasing the freely ionized portion of total serum calcium. For every 0.1 increase in pH, ionized calcium decreases by about 0.05 mmol/l.
This hypocalcemia related to alkalosis is partially responsible for the cerebral vasoconstriction that causes the lightheadedness, fainting, and parasthesia often seen with hyperventilation.
Causes
Hypocalcemia can be the consequence of multiple disease processes, some of which will be mentioned in the following discussion. The most common cause is the inability to mobilize calcium from bone which is primarily induced by decreased levels of the parathyroid hormone (PTH) due to derangement of the parathyroid gland function (ie, the gland responsible of calcium homeostasis) or vitamin D deficiency.
- Hypoparathyroidism: It signifies diminished activity of the parathyroid gland due to multiple reasons: autoimmune destruction (included in the polyglandular autoimmune syndrome type I), resection of the glands as a possible complication of total thyroidectomy or genetic diseases affecting the gland's function. A second entity that should be mentioned is pseudohypoparathyroidism which is characterized by normal gland function but inability of the PTH-target organs (bone and kidney) to respond to PTH. Patients present with hypocalcemia but high PTH levels.
Complete Differential Diagnosis of the Causes of Hypocalcemia
(In alphabetical order)
- Absent active vitamin D
- Absent parathyroid hormone (PTH)
- Acquired hypoparathyroidism
- Acute pancreatitis
- Acute renal failure
- Adrenocortical hyperplasia
- Alcohol abuse
- Alkalosis
- Anticonvulsant therapy
- Breast cancer
- Bronchial cancer
- Burns
- Chelation therapy
- Chronic renal failure
- Cirrhosis
- Decreased dietary intake
- Decreased ultraviolet/sun (vitamin D deficiency)
- Defective Vitamin D metabolism
- Deficient PTH
- DiGeorge's syndrome
- Diuretic therapy
- Drugs
- Eating disorders
- Enemas, laxatives
- Enhanced bone formation
- Excessive secretion of calcitonin
- Exposure to hydrofluoric acid
- Familial hypocalcemia
- Following thyroidectomy
- Hereditary hypoparathyroidism
- "Hungry Bone Syndrome" following parathyroidectomy,
- Hyperphosphatemia
- Hyperventilation.
- Hypoalbuminemia (pseudohypocalcemia)
- Hypomagnesemia
- Hypoparathyroidism
- Hypoproteinemia
- Increased diuresis with physiologic saline solution
- Intestinal malabsorption
- Intravenous phosphate administration
- Kidney diseases with reduced formation of activated vitamin D
- Magnesium depletion
- Magnesium over supplementation
- Malabsorption
- Maldigestion
- Medullary carcinoma of the thyroid
- Neonatal tetany
- Nephrotic syndrome
- Osteitis fibrosa following parathyroidectomy
- Osteoblastic metastases
- Osteoporosis
- Pancreatitis
- Polyglandular autoimmune syndrome
- Postoperative
- Prolonged use of medications/laxatives containing magnesium
- Pseudohypoparathyroidism
- Renal failure
- Rhabdomyolysis
- Rickets
- Sepsis
- Septic shock
- Severe acute hyperphosphatemia
- Short bowel syndrome
- Steroid therapy
- Thyroid cancer
- Transfusion of citrated blood
- Tumor lysis syndrome
- Vitamin D deficiency
- Vitamin-D dependent rickets, type I
Complete Differential Diagnosis of the Causes of Hypocalcemia
(By organ system)
| Cardiovascular | No underlying causes |
| Chemical / poisoning | Alcohol abuse |
| Dermatologic | No underlying causes |
| Drug Side Effect | Anticonvulsant therapy, Chelation therapy, Diuretic therapy, Drugs, Enemas, laxatives, Steroid therapy |
| Ear Nose Throat | No underlying causes |
| Endocrine | Absent parathyroid hormone (PTH), Acquired hypoparathyroidism, Adrenocortical hyperplasia, Deficient PTH, Excessive secretion of calcitonin, Familial hypocalcemia, Following thyroidectomy, Hereditary hypoparathyroidism, "Hungry Bone Syndrome" following parathyroidectomy, Hypoparathyroidism, Hypoproteinemia, Medullary carcinoma of the thyroid, Osteitis fibrosa following parathyroidectomy, Osteoporosis, Pseudohypoparathyroidism, Thyroid cancer |
| Environmental | Decreased ultraviolet/sun (vitamin D deficiency), Defective Vitamin D metabolism, Exposure to hydrofluoric acid |
| Gastroenterologic | Acute pancreatitis, Cirrhosis, Decreased dietary intake, Eating disorders, Enemas, laxatives, Intestinal malabsorption, Malabsorption, Maldigestion, Pancreatitis, Rickets, Short bowel syndrome, Vitamin-D dependent rickets, type I |
| Genetic | DiGeorge's Syndrome, Familial hypocalcemia |
| Hematologic | Hypoalbuminemia (pseudohypocalcemia), Transfusion of citrated blood, Tumor lysis syndrome |
| Iatrogenic | No underlying causes |
| Infectious Disease | Sepsis, Septic shock |
| Musculoskeletal / Ortho | Enhanced bone formation, Excessive secretion of calcitonin, Neonatal tetany, Osteitis fibrosa following parathyroidectomy, Osteoporosis, Rickets, Vitamin-D dependent rickets, type I |
| Neurologic | No underlying causes |
| Nutritional / Metabolic | Absent active vitamin D, Decreased dietary intake, Hyperphosphatemia, Intestinal malabsorption, Intravenous phosphate administration, Magnesium depletion, Rickets, Vitamin D deficiency |
| Obstetric/Gynecologic | Breast cancer |
| Oncologic | Breast cancer, Bronchial cancer, Medullary carcinoma of the thyroid, Osteoblastic metastases, Thyroid cancer, Tumor lysis syndrome |
| Opthalmologic | No underlying causes |
| Overdose / Toxicity | Magnesium over supplementation, Prolonged use of medications/laxatives containing magnesium |
| Psychiatric | Eating disorders |
| Pulmonary | Bronchial cancer, Hyperventilation |
| Renal / Electrolyte | Acute renal failure, Alkalosis, Chronic renal failure, Hypomagnesemia, Hypoproteinemia, Increased diuresis with physiologic saline solution, Intravenous phosphate administration, Kidney diseases with reduced formation of activated vitamin D, Magnesium depletion, Magnesium over supplementation, Nephrotic syndrome, Renal failure, Rhabdomyolysis, Severe acute hyperphosphatemia |
| Rheum / Immune / Allergy | DiGeorge's Syndrome, Osteitis fibrosa following parathyroidectomy, Polyglandular autoimmune syndrome |
| Sexual | No underlying causes |
| Trauma | Burns |
| Urologic | Acute renal failure, Chronic renal failure, Hypoproteinemia, Renal failure |
| Miscellaneous | Postoperative, Transfusion of citrated blood |
Diagnosis
History and Symptoms
- Fatigue
- Weakness
- Muscle cramping and spasm
- Nausea and vomiting
- Abdominal pain
- Depression
- Irritability
- Delirium
- Psychosis
- Seizures (with severe hypocalcemia)
- Perioral tingling and parasthesia, 'pins and needles' sensation over the extremities of hands and feet. This is the earliest symptom of hypocalcemia.
Signs
- Tetany, carpopedal spasm are seen.
- Latent tetany
- Trousseau sign of latent tetany (eliciting carpal spasm by inflating the blood pressure cuff and maintaining the cuff pressure above systolic)
- Chvostek's sign (tapping of the inferior portion of the zygoma will produce facial spasms)
- Tendon reflexes are hyperactive
- Life threatening complications
Clinical Features Associated with Hypocalcemia
- Abdominal pain
- Alopecia
- Anxiety
- Atopic eczema
- Biliary colic
- Brittle nails
- Bronchial spasm
- Calcification of cerebral cortex or cerebellum
- Cardiomyopathy
- Choreoathetosis
- Chvostek's sign
- Coarse hair
- Confusion
- Congestive heart failure
- Delayed tooth eruption
- Disorientation
- Dry skin
- Dysphagia
- Dyspnea
- Dystonic spasms
- Enamel hypoplasia
- Exfoliative dermatitis
- Extrapyramidal signs due to calcification of basal ganglia
- Fatigue
- Impaired intellectual ability
- Impetigo herpetiformis
- Increased dental caries
- Increased intracranial pressure
- Irritability
- Laryngeal spasm
- Muscle cramps
- Nonspecific EEG changes
- Papilledema
- Paresthesia
- Parkinsonism
- Personality disturbances
- Polymyositis
- Prolonged QT interval in EKG
- Psoriasis
- Psychoneurosis
- Psychosis
- Seizures (focal, petit mal, grand mal)
- Shortened premolar roots
- Subcapsular cataracts
- Tetany
- Thickened lamina dura
- Trousseau's sign
- Wheezing
Laboratory Findings
Suggested initial laboratory studies include the following:
- Serum calcium
- Ionized calcium
- Complete blood count
- Blood urea nitrogen (BUN)/creatinine
- Magnesium
- Albumin
- Phosphorus
- Amylase/lipase
Additional laboratory studies to be obtained as part of a more complete evaluation include the following:
- Vitamin D levels
- Parathyroid hormone
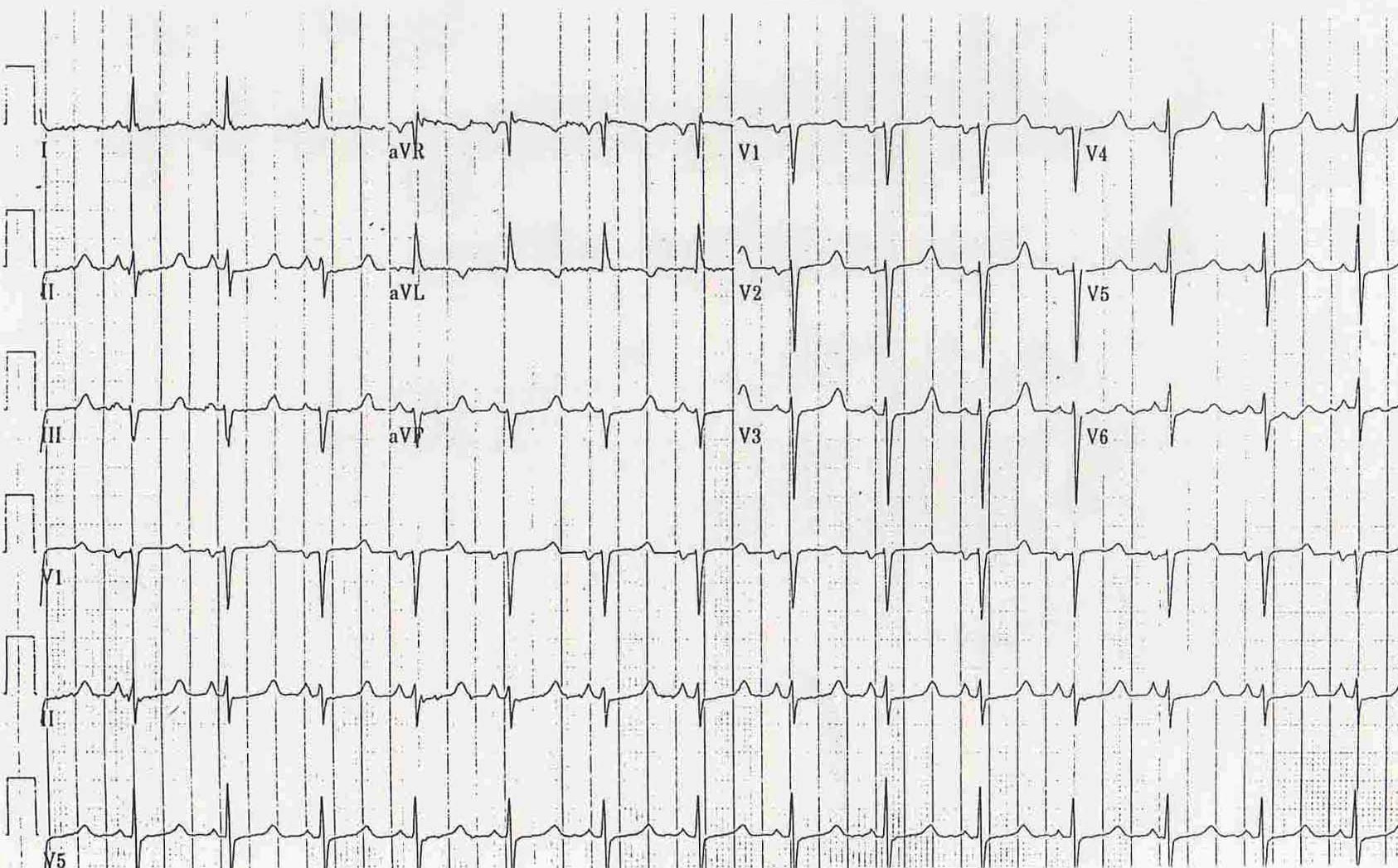
Electrocardiographic Findings
- Prolongation of the QTc interval is the major EKG finding
- There is a lengthening of the interval between the end of the QRS and the beginning of the T wave (i.e. ST-segment lengthening).
EKG examples
Management
- Two ampoules of intravenous calcium gluconate 10% is given slowly in a period of 10 minutes, or if the hypocalcemia is severe, calcium chloride is given instead.
- Maintenance doses of both calcium and vitamin-D (often as 1,25-(OH)2-D3, i.e. calcitriol)) are often necessary to prevent further decline.
References
Related chapters
- Calcium metabolism
- Hypercalcaemia
- Calcium deficiency (plant disorder)
- Hypomagnesemia with secondary hypocalcemia
Resources
- Cleveland Clinic Hypocalcemia chapter Online Medical Reference
- Endotext
- EKG abnormalities associated with hypocalcemia
- Seizures due to hypocalcaemia worsened by shifting towards alkalosis by bicarbonate therapy
- Electrolytes