Hospital readmissions
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Hospital readmission is the unplanned readmission for any cause to any acute care hospital within a certain period of time following the discharge from a hospitalization. Centers for Medicare and Medicaid Services (CMS) choose to measure unplanned readmission within 30 days instead of over longer time periods (such as 90 days), because readmissions over longer periods may be impacted by factors outside hospitals’ control such as other complicating illnesses, patients’ own behavior, or care provided to patients after discharge.
Epidemiology
Among Medicare patients in the United States receiving care in a fee-for-service setting during 2003-2004, 19.6% were rehospitalized within 30 days following their discharge from the hospital.[1]
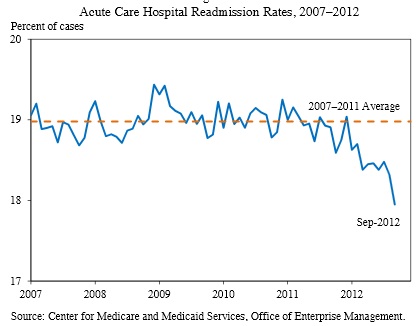
Shown below is an image depicting the hospital readmission rate in 2013 according to Centers for Medicare and Medicaid Services (CMS).
Causes
In a study of Medicare patients in the United States, most of the variation in rates of readmission are due to characteristics of patients.[2] A much smaller degree of variation is due to characteristics of hospitals or health care providers.[2]
A systematic review found that approximately 25% of readmissions are avoidable; however, rates varied widely among individual studies included within the review.[3]
Costs
Prediction
Physicians are specific in their predictors, but not sensitive[4].
A number of methods have been developed to predict which patients will be readmitted. Two or more italizations within a year is a simple predictor of readmission. A study of adult patients in the University of Pennsylvania Health System found that ≥ 2 inpatient admissions in the past 12 months had a sensitivity and specificity of 39% and 84%, respectively, for predicting readmission. In populations similar to those in this study which had a prevalence of ital readmission of 15%, the probabilities of ital readmission among patients with and without ≥ 2 inpatient admissions in the past 12 months were 30.0% and 11.0%, respectively.
Prevention
Adults
A meta-analysis of 42 randomized clinical trials found “interventions are effective at reducing readmissions, but more effective interventions are complex and support patient capacity for self-care.”[5] This review also reported that more recent trials showed less impact. Accordingly, two more recent trials were negative, but both had strong interventions in the control group. In one of the trials, a virtual ward reduced admissions by 4%, but this was not statistically significant.[6] Another subsequent trial reports an insignificant increase in readmissions or emergency department visits in the intervention group.[7] A more recent trial of an interprofessional intervention found benefit (about 50% had a transition of care visit within 7 days)[8].
Regarding telephone calls to patients after discharge, detailed, scripted phone calls may be effective[9]
The Camden Coalition of Healthcare Providers using the Camden Core Model and "hotspotting" was not able to reduce readmissions among superusers in a randomized controlled trial[10]. Limitations of the study included "a home visit within 5 days after hospital discharge and a visit to a provider’s office within 7 days after discharge — were achieved less than 30% of the time." Visit with a hphysician within 7 days occurred after 36% of hospitalizations.
Medication review
A medication review, if combined with other interventions, may reduce hospital readmissions according to a systematic review[11][12]
. Previously, regarding medication reconciliations, a meta-analysis by the Cochrane Collaboration found no clear benefit.[13]
The role of primary care
Notifying the primary care physician at the time of admission, using the hospital's HL7 Admission, discharge, and transfer system (ADT) message or feed may reduce readmissions[14].
.Regarding seeing a primary care provider within one week of discharge, a cohort of Medicaid patients found benefit[15]. However, among a cohort of patients who all have a primary care physician, the impact of the primary care physician is not certain[16].
The Beth Israel Deaconess Medical Center found that interventions have been able to increase outpatient follow-up visits (after 60% of hospitalizations), but the impact of this on preventing readmission is not certain[17]. interpretation of the results may have been limited by sample size as the readmission rate dropped by 2% but this was not statistically significant.
Phone calls from primary care sites to patients after discharge may help[18].
Follow-up visits after emergency department visits may also be important[19].
Regarding telephone calls to primary care providers by hospital providers, readmissions may not be reduced.[20].
Team-based care may reduce hospitalizations among veterans, although readmissions was not specifically studied[21].
Pediatrics
A systematic review of observational studies regarding the prevention of readmissions observed “patients receiving home visits, care coordination, chronic care-management, and continuity across settings had fewer preventable hospitalizations[22].” In addition, a proactive and coordinated effort of the pharmacy team during discharge planning may have a positive impact on patients obtaining medications according to a trial not included in the systematic review (intervention 84%, control 69%).[23] With regards to written patient information, those receiving both verbal and written information showed increased health-care related knowledge at follow-up visits compared with verbal discharge instructions alone (intervention 79%, control 73%).[24]
Hospital consultation from outpatient clinicians for medically complex children may reduce readmissions and hospital length of stay[25].
See also
References
- ↑ Jencks SF, Williams MV, Coleman EA (2009). "Rehospitalizations among patients in the Medicare fee-for-service program". N Engl J Med. 360 (14): 1418–28. doi:10.1056/NEJMsa0803563. PMID 19339721.
- ↑ 2.0 2.1 Singh S, Lin YL, Kuo YF, Nattinger AB, Goodwin JS (2014). "Variation in the risk of readmission among hospitals: the relative contribution of patient, hospital and inpatient provider characteristics". J Gen Intern Med. 29 (4): 572–8. doi:10.1007/s11606-013-2723-7. PMC 3965757. PMID 24307260.
- ↑ van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ (2011). "Proportion of hospital readmissions deemed avoidable: a systematic review". CMAJ. 183 (7): E391–402. doi:10.1503/cmaj.101860. PMC 3080556. PMID 21444623.
- ↑ Nguyen, O.K., Washington, C., Clark, C.R. et al. Man vs. Machine: Comparing Physician vs. Electronic Health Record–Based Model Predictions for 30-Day Hospital Readmissions. J GEN INTERN MED 36, 2555–2562 (2021). https://doi.org/10.1007/s11606-020-06355-3
- ↑ Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K; et al. (2014). "Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials". JAMA Intern Med. 174 (7): 1095–107. doi:10.1001/jamainternmed.2014.1608. PMID 24820131.
- ↑ Dhalla IA, O'Brien T, Morra D, Thorpe KE, Wong BM, Mehta R; et al. (2014). "Effect of a postdischarge virtual ward on readmission or death for high-risk patients: a randomized clinical trial". JAMA. 312 (13): 1305–12. doi:10.1001/jama.2014.11492. PMID 25268437.
- ↑ Goldman LE, Sarkar U, Kessell E, Guzman D, Schneidermann M, Pierluissi E; et al. (2014). "Support from hospital to home for elders: a randomized trial". Ann Intern Med. 161 (7): 472–81. doi:10.7326/M14-0094. PMID 25285540.
- ↑ Liss DT, Ackermann RT, Cooper A, Finch EA, Hurt C, Lancki N; et al. (2019). "Effects of a Transitional Care Practice for a Vulnerable Population: a Pragmatic, Randomized Comparative Effectiveness Trial". J Gen Intern Med. doi:10.1007/s11606-019-05078-4. PMID 31144279.
- ↑ Melton LD, Foreman C, Scott E, McGinnis M, Cousins M (2012). "Prioritized post-discharge telephonic outreach reduces hospital readmissions for select high-risk patients". Am J Manag Care. 18 (12): 838–44. PMID 23286612.
- ↑ Finkelstein A, Zhou A, Taubman S, Doyle J (2020). "Health Care Hotspotting - A Randomized, Controlled Trial". N Engl J Med. 382 (2): 152–162. doi:10.1056/NEJMsa1906848. PMID 31914242.
- ↑ Dautzenberg L, Bretagne L, Koek HL, Tsokani S, Zevgiti S, Rodondi N; et al. (2021). "Medication review interventions to reduce hospital readmissions in older people". J Am Geriatr Soc. doi:10.1111/jgs.17041. PMID 33576506 Check
|pmid=value (help). - ↑ Becker C, Zumbrunn S, Beck K, Vincent A, Loretz N, Müller J; et al. (2021). "Interventions to Improve Communication at Hospital Discharge and Rates of Readmission: A Systematic Review and Meta-analysis". JAMA Netw Open. 4 (8): e2119346. doi:10.1001/jamanetworkopen.2021.19346. PMC 8397933 Check
|pmc=value (help). PMID 34448868 Check|pmid=value (help). - ↑ Christensen M, Lundh A (2013). "Medication review in hospitalised patients to reduce morbidity and mortality". Cochrane Database Syst Rev. 2: CD008986. doi:10.1002/14651858.CD008986.pub2. PMID 23450593.
- ↑ Unruh MA, Jung HY, Kaushal R, Vest JR (2017). "Hospitalization event notifications and reductions in readmissions of Medicare fee-for-service beneficiaries in the Bronx, New York". J Am Med Inform Assoc. 24 (e1): e150–e156. doi:10.1093/jamia/ocw139. PMID 28395059.
- ↑ Wiest D, Yang Q, Wilson C, Dravid N (2019). "Outcomes of a Citywide Campaign to Reduce Medicaid Hospital Readmissions With Connection to Primary Care Within 7 Days of Hospital Discharge". JAMA Netw Open. 2 (1): e187369. doi:10.1001/jamanetworkopen.2018.7369. PMID 30681708.
- ↑ Singh S, Goodwin JS, Zhou J, Kuo YF, Nattinger AB (2019). "Variation Among Primary Care Physicians in 30-Day Readmissions". Ann Intern Med. 170 (11): 749–755. doi:10.7326/M18-2526. PMC 6743324 Check
|pmc=value (help). PMID 31108502. - ↑ Marcondes FO, Punjabi P, Doctoroff L, Tess A, O'Neill S, Layton T; et al. (2019). "Does Scheduling a Postdischarge Visit with a Primary Care Physician Increase Rates of Follow-up and Decrease Readmissions?". J Hosp Med. 14: E37–E42. doi:10.12788/jhm.3309. PMID 31532749.
- ↑ Tang N, Fujimoto J, Karliner L (2014). "Evaluation of a primary care-based post-discharge phone call program: keeping the primary care practice at the center of post-hospitalization care transition". J Gen Intern Med. 29 (11): 1513–8. doi:10.1007/s11606-014-2942-6. PMC 4238210. PMID 25055997.
- ↑ Lin MP, Burke RC, Orav EJ, Friend TH, Burke LG (2020). "Ambulatory Follow-up and Outcomes Among Medicare Beneficiaries After Emergency Department Discharge". JAMA Netw Open. 3 (10): e2019878. doi:10.1001/jamanetworkopen.2020.19878. PMC 7547366 Check
|pmc=value (help). PMID 33034640 Check|pmid=value (help). - ↑ Oduyebo I, Lehmann CU, Pollack CE, Durkin N, Miller JD, Mandell S; et al. (2013). "Association of self-reported hospital discharge handoffs with 30-day readmissions". JAMA Intern Med. 173 (8): 624–9. doi:10.1001/jamainternmed.2013.3746. PMC 3692004. PMID 23529278.
- ↑ Germack HD, Leung L, Zhao X, Zhang H, Martsolf GR (2021). "Association of Team-Based Care and Continuity of Care with Hospitalizations for Veterans with Comorbid Mental and Physical Health Conditions". J Gen Intern Med. doi:10.1007/s11606-021-06884-5. PMID 34027614 Check
|pmid=value (help). - ↑ Coller RJ, Nelson BB, Sklansky DJ, Saenz AA, Klitzner TS, Lerner CF; et al. (2014). "Preventing hospitalizations in children with medical complexity: a systematic review". Pediatrics. 134 (6): e1628–47. doi:10.1542/peds.2014-1956. PMID 25384492.
- ↑ Voirol P, Kayser SR, Chang CY, Chang QL, Youmans SL (2004). "Impact of pharmacists' interventions on the pediatric discharge medication process". Ann Pharmacother. 38 (10): 1597–602. doi:10.1345/aph.1E087. PMID 15328395.
- ↑ Jenkins HM, Blank V, Miller K, Turner J, Stanwick RS (1996). "A randomized single-blind evaluation of a discharge teaching book for pediatric patients with burns". J Burn Care Rehabil. 17 (1): 49–61. PMID 8808360.
- ↑ Mosquera RA, Avritscher EBC, Pedroza C, Bell CS, Samuels CL, Harris TS; et al. (2021). "Hospital Consultation From Outpatient Clinicians for Medically Complex Children: A Randomized Clinical Trial". JAMA Pediatr. 175 (1): e205026. doi:10.1001/jamapediatrics.2020.5026. PMID 33252671 Check
|pmid=value (help).