Hookworm infection

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Risk Factors
People who have direct contact with soil that contains human feces in areas where hookworm is common are at high risk of infection. Children --because they play in dirt and often go barefoot-- are at high risk. Since transmission of hookworm infection requires development of the larvae in soil, hookworm cannot be spread person to person. Contact among children in institutional or child care settings should not increase the risk of infection.
Pathophysiology & Etiology
Etiologic agents:
The human hookworms include two nematode (roundworm) species, Ancylostoma duodenale and Necator americanus. (Adult females: 10 to 13 mm (A. duodenale), 9 to 11 mm (N. americanus); adult males: 8 to 11 mm (A. duodenale), 7 to 9 mm (N. americanus). A smaller group of hookworms infecting animals can invade and parasitize humans (A. ceylanicum) or can penetrate the human skin (causing cutaneous larva migrans), but do not develop any further (A. braziliense, A. caninum, Uncinaria stenocephala). Occasionally A. caninum larva may migrate to the human intestine causing eosinophilic enteritis; this may happen when larva is ingested rather than through skin invasion.
Life cycle:

Eggs are passed in the stool 1, and under favorable conditions (moisture, warmth, shade), larvae hatch in 1 to 2 days. The released rhabditiform larvae grow in the feces and/or the soil 2, and after 5 to 10 days (and two molts) they become become filariform (third-stage) larvae that are infective 3. These infective larvae can survive 3 to 4 weeks in favorable environmental conditions. On contact with the human host, the larvae penetrate the skin and are carried through the veins to the heart and then to the lungs. They penetrate into the pulmonary alveoli, ascend the bronchial tree to the pharynx, and are swallowed 4. The larvae reach the small intestine, where they reside and mature into adults. Adult worms live in the lumen of the small intestine, where they attach to the intestinal wall with resultant blood loss by the host 5. Most adult worms are eliminated in 1 to 2 years, but longevity records can reach several years. Some A. duodenale larvae, following penetration of the host skin, can become dormant (in the intestine or muscle). In addition, infection by A. duodenale may probably also occur by the oral and transmammary route. N. americanus, however, requires a transpulmonary migration phase.
Can animals transmit hookworm infection to me?
Yes, but not directly. Puppies and kittens are especially likely to have hookworm infections. Animals that are infected pass hookworm eggs in their stools. The eggs can hatch into larvae, and both eggs and larvae may be found in dirt where animals have been. Eggs or larvae can get into your body when you accidentally eat or have direct contact with contaminated dirt. For example, this can happen if a child is walking barefoot or playing in an area where dogs or cats have been (especially puppies or kittens).
Diagnosis
History and Symptoms
Iron deficiency anemia (caused by blood loss at the site of intestinal attachment of the adult worms) is the most common symptom of hookworm infection, and can be accompanied by cardiac complications. Gastrointestinal and nutritional/metabolic symptoms can also occur. In addition, local skin manifestations ("ground itch") can occur during penetration by the filariform (L3) larvae, and respiratory symptoms can be observed during pulmonary migration of the larvae.
Laboratory Diagnosis:
Microscopy:
Microscopic identification of eggs in the stool is the most common method for diagnosing hookworm infection. The recommended procedure is as follows:
- Collect a stool specimen.
- Fix the specimen in 10% formalin.
- Concentrate using the formalin–ethyl acetate sedimentation technique.
- Examine a wet mount of the sediment.
Where concentration procedures are not available, a direct wet mount examination of the specimen is adequate for detecting moderate to heavy infections. For quantitative assessments of infection, various methods such as the Kato-Katz can be used.
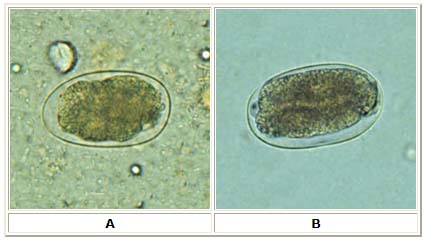
A, B: Hookworm eggs examined on wet mount (eggs of Ancylostoma duodenale and Necator americanus cannot be distinguished morphologically).
Diagnostic characteristics:
- Size 57 to 76 µm by 35 to 47 µm
- Oval or ellipsoidal shape
- Thin shell
The embryo in B has begun cellular division and is at an early (gastrula) developmental stage.
Examination of the eggs cannot distinguish between N. americanus and A. duodenale. Larvae can be used to differentiate between N. americanus and A. duodenale, by rearing filariform larvae in a fecal smear on a moist filter paper strip for 5 to 7 days (Harada-Mori). Occasionally, it may be necessary to distinguish between the rhabditiform larvae (L2) of hookworms and those of Strongyloides stercoralis.
Risk Stratification and Prognosis
The most serious results of hookworm infection are the development of anemia and protein deficiency caused by blood loss. When children are continuously infected by many worms, the loss of iron and protein can retard growth and mental development, sometimes irreversibly. Hookworm infection can also cause tiredness, difficulty breathing, enlargement of the heart, and irregular heartbeat. Sometimes hookworm infection is fatal, especially among infants.
Treatment
In countries where hookworm is common and reinfection is likely, light infections are often not treated.
Pharmacotherapy
In the United States, hookworm infections are generally treated with albendazole. Mebendazole or pyrantel pamoate can also be used.
Primary Prevention
Do not walk barefoot or contact the soil with bare hands in areas where hookworm is common or there is likely to be feces in the soil or sand.
References
- http://www.cdc.gov/ncidod/diseases/submenus/sub_hookworm.htm
- http://www.dpd.cdc.gov/dpdx/HTML/Hookworm.htm
- http://www.cdc.gov/healthypets/diseases/hookworm.htm
- http://www.cdc.gov/ncidod/dpd/parasites/hookworm/default.htm
- http://www.cdc.gov/ncidod/dpd/parasites/hookworm/factsht_hookworm.htm
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson, M.S., M.D.