Hodgkin's lymphoma pathophysiology
|
Hodgkin's lymphoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hodgkin's lymphoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Hodgkin's lymphoma pathophysiology |
|
Risk calculators and risk factors for Hodgkin's lymphoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Overview
Pathophysiology
Gross Pathology
Affected lymph nodes (most often, laterocervical lymph nodes) are enlarged, but their shape is preserved because the capsule is not invaded. Usually, the cut surface is white-grey and uniform; in some histological subtypes (e.g. nodular sclerosis) may appear a nodular aspect
Microscopic Pathology
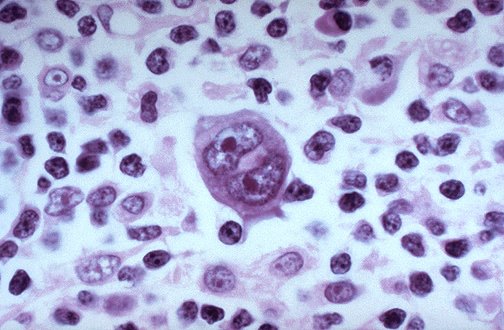
Microscopic examination of the lymph node biopsy reveals complete or partial effacement of the lymph node architecture by scattered large malignant cells known as Reed-Sternberg cells (typical and variants) admixed within a reactive cell infiltrate composed of variable proportions of lymphocytes, histiocytes, eosinophils, and plasma cells. The Reed-Sternberg cells are identified as large often bi-nucleated cells with prominent nucleoli and an unusual CD45-, CD30+, CD15+/- immunophenotype. In approximately 50% of cases, the Reed-Sternberg cells are infected by the Epstein-Barr virus.
Characteristics of classic Reed-Sternberg cells include large size (20–50 micrometres), abundant, amphophilic, finely granular/homogeneous cytoplasm; two mirror-image nuclei (owl eyes) each with an eosinophilic nucleolus and a thick nuclear membrane (chromatin is distributed at the cell periphery).
Variants:
- Hodgkin's cell (atypical mononuclear RSC) is a variant of RS cell, which has the same characteristics, but is mononucleated.
- Lacunar RSC is large, with a single hyperlobated nucleus, multiple, small nucleoli and eosinophilic cytoplasm which is retracted around the nucleus, creating an empty space ("lacunae").
- Pleomorphic RSC has multiple irregular nuclei.
- "Popcorn" RSC (lympho-histiocytic variant) is a small cell, with a very lobulated nucleus, small nucleoli.
- "Mummy" RSC has a compact nucleus, no nucleolus and basophilic cytoplasm. [2]
Hodgkin's lymphoma can be sub-classified by histological type. The cell histology in Hodgkin's lymphoma is not as important as it is in non-Hodgkin's lymphoma: the treatment and prognosis in Hodgkin's lymphoma depend on the stage of disease rather than the histotype.
Staging
After Hodgkin's lymphoma is diagnosed, a patient will be staged: that is, they will undergo a series of tests and procedures which will determine what areas of the body are affected. These procedures will include documentation of their histology, a physical examination, blood tests, chest X-ray radiographs, computed tomography (CT) scans or magnetic resonance imaging (MRI) scans of the chest, abdomen and pelvis, and a bone marrow biopsy. Positron emission tomography (PET) scan is now used instead of the gallium scan for staging. In the past, a lymphangiogram or surgical laparotomy (which involves opening the abdominal cavity and visually inspecting for tumors) were performed. Lymphangiograms or laparotomies are very rarely performed, having been supplanted by improvements in imaging with the CT scan and PET scan.
On the basis of this staging, the patient will be classified according to a staging classification (the Ann Arbor staging classification scheme is a common one):
- Stage I is involvement of a single lymph node region (I) or single extralymphatic site (Ie);
- Stage II is involvement of two or more lymph node regions on the same side of the diaphragm (II) or of one lymph node region and a contiguous extralymphatic site (IIe);
- Stage III is involvement of lymph node regions on both sides of the diaphragm, which may include the spleen (IIIs) and/or limited contiguous extralymphatic organ or site (IIIe, IIIes);
- Stage IV is disseminated involvement of one or more extralymphatic organs.
The absence of systemic symptoms is signified by adding 'A' to the stage; the presence of systemic symptoms is signified by adding 'B' to the stage.