Hodgkin's lymphoma natural history, complications and prognosis: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (46 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Hodgkin's lymphoma}} | {{Hodgkin's lymphoma}} | ||
{{CMG}}; {{AE}} {{AS}} | {{CMG}}; {{AE}} {{AS}} {{M.B}} | ||
==Overview== | ==Overview== | ||
The early stage of the Hodgkin's lymphoma is associated with the most favorable prognosis | Hodgkin's lymphoma has a [[Bimodal distribution|bimodal age distribution]] and both children and adult may be affected. The early peak occurs in the middle-to-late 20's and the second peak after the age of 50. [[Treatment Planning|Treatment]] outcomes of Hodgkin’s lymphoma are excellent and five-year [[Survival rate|survival rates]] are more than 80%. Owing to modern therapies, the natural history of untreated Hodgkin’s lymphoma is actually difficult to determine. Survivors are at risk for relapse, second primary malignancies, cardiovascular [[Complication (medicine)|complications]] and other treatment-related [[Toxicity|toxicities]]. [[Prognosis]] is based on the stage of the disease and other prognostic factors. The early stage of the Hodgkin's lymphoma is associated with the most favorable prognosis and the 5-year survival rate of patients with Hodgkin's lymphoma varies with the stage of the disease. | ||
== Natural History == | |||
* Hodgkin's lymphoma has a [[Bimodal distribution|bimodal age distribution]] and both children and adult may be affected. The most common symptom of classic Hodgkin's lymphoma includes painless localized peripheral lymphadenopathy. | |||
* Owing to modern therapies, the natural history of untreated Hodgkin’s lymphoma is actually difficult to determine. | |||
* If left untreated, Hodgkin's lymphoma develop complications depend on site and size of mass, including [[Breathing|breathing problem]], [[hypoxemia]], [[chest pain]], significant [[weight loss]], and a [[tracheoesophageal fistula]] and eventually significant decrease in the overall survival.<ref name="Greco1974">{{cite journal|last1=Greco|first1=Ralph S.|title=Hodgkin Disease in Connecticut From 1935 to 1962|journal=Archives of Internal Medicine|volume=134|issue=6|year=1974|pages=1039|issn=0003-9926|doi=10.1001/archinte.1974.00320240073007}}</ref> | |||
== Complications == | |||
* The main complications of Hodgkin lymphoma are due to side effects of chemotherapy and/or radiotherapy, table below provides these general side effects: | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | |||
|+ '''Complications of Medical Therapy''' | |||
| style="background: #4479BA;; color:#FFF;" | Complications of Chemotherapy<ref name="Cancer.ca">Hodgkin-lymphoma. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/hodgkin-lymphoma/treatment/?region=ab Accessed on September 10, 2015</ref> | |||
| style="background: #4479BA;; color:#FFF;" | Complications of Radiotherapy<ref name="Cancer.ca">Hodgkin-lymphoma. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/hodgkin-lymphoma/treatment/?region=ab Accessed on September 10, 2015</ref> | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Skin reactions | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Skin changes | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Nausea]] and [[vomiting]] | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Nausea and vomiting | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Sore throat]] and painful swallowing | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Sore mouth | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Taste changes | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Loss of appetite]] | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Fatigue]] | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Fatigue]] | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Diarrhea]] | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Diarrhea | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Bone marrow suppression]] | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Bone marrow suppression | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Dental cavities]] | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Constipation]] | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Thyroid problems | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Hair loss]] | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Fertility problems | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Cystitis]] | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Heart and lung problems | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Muscle and joint pain | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Second cancers | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Second cancers | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Pain at the injection site | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Inflammation of the vein | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Allergic reactions]] | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Organ damage | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | [[Fluid retention]] | |||
|} | |||
* Leading complications in Hodgkin lymphoma survivors are second primary malignancies and cardiovascular toxicities. Cardiovascular complications of radiation therapy (RT) include [[pericarditis]], [[Myocardium|myocardial]] [[ischemia]] or [[infarction]], [[cardiomyopathy]], [[heart failure]], [[Valvular heart disease|valvular abnormalities]], or [[Conduction system disease|conduction abnormalities]]. <ref>{{Cite journal | |||
| author = [[Shira L. Galper]], [[James B. Yu]], [[Peter M. Mauch]], [[Jon F. Strasser]], [[Barbara Silver]], [[Ann Lacasce]], [[Karen J. Marcus]], [[Mary Ann Stevenson]], [[Ming Hui Chen]] & [[Andrea K. Ng]] | |||
| title = Clinically significant cardiac disease in patients with Hodgkin lymphoma treated with mediastinal irradiation | |||
| journal = [[Blood]] | |||
| volume = 117 | |||
| issue = 2 | |||
| pages = 412–418 | |||
| year = 2011 | |||
| month = January | |||
| doi = 10.1182/blood-2010-06-291328 | |||
| pmid = 20858859 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Andrea K. Ng]], [[Ann LaCasce]] & [[Lois B. Travis]] | |||
| title = Long-term complications of lymphoma and its treatment | |||
| journal = [[Journal of clinical oncology : official journal of the American Society of Clinical Oncology]] | |||
| volume = 29 | |||
| issue = 14 | |||
| pages = 1885–1892 | |||
| year = 2011 | |||
| month = May | |||
| doi = 10.1200/JCO.2010.32.8427 | |||
| pmid = 21483015 | |||
}}</ref> | |||
* Breast, lung, and colon cancer are the majority of second cancers in Hodgkin’s lymphoma survivors. <ref>{{Cite journal | |||
| author = [[Michael Schaapveld]], [[Berthe M. P. Aleman]], [[Anna M. van Eggermond]], [[Cecile P. M. Janus]], [[Augustinus D. G. Krol]], [[Richard W. M. van der Maazen]], [[Judith Roesink]], [[John M. M. Raemaekers]], [[Jan Paul de Boer]], [[Josee M. Zijlstra]], [[Gustaaf W. van Imhoff]], [[Eefke J. Petersen]], [[Philip M. P. Poortmans]], [[Max Beijert]], [[Marnix L. Lybeert]], [[Ina Mulder]], [[Otto Visser]], [[Marieke W. J. Louwman]], [[Inge M. Krul]], [[Pieternella J. Lugtenburg]] & [[Flora E. van Leeuwen]] | |||
| title = Second Cancer Risk Up to 40 Years after Treatment for Hodgkin's Lymphoma | |||
| journal = [[The New England journal of medicine]] | |||
| volume = 373 | |||
| issue = 26 | |||
| pages = 2499–2511 | |||
| year = 2015 | |||
| month = December | |||
| doi = 10.1056/NEJMoa1505949 | |||
| pmid = 26699166 | |||
}}</ref> | |||
* [[Leukemia]] and [[non-Hodgkin lymphoma]] ([[Non-Hodgkin lymphoma|NHL)]] are less common. Most leukemias that occur after the treatment are [[acute myeloid leukemia]] ([[AML]]) related to [[Alkylating antineoplastic agent|alkylating agent]] exposure. <ref>{{Cite journal | |||
| author = [[J. M. Kaldor]], [[N. E. Day]], [[E. A. Clarke]], [[F. E. Van Leeuwen]], [[M. Henry-Amar]], [[M. V. Fiorentino]], [[J. Bell]], [[D. Pedersen]], [[P. Band]] & [[D. Assouline]] | |||
| title = Leukemia following Hodgkin's disease | |||
| journal = [[The New England journal of medicine]] | |||
| volume = 322 | |||
| issue = 1 | |||
| pages = 7–13 | |||
| year = 1990 | |||
| month = January | |||
| doi = 10.1056/NEJM199001043220102 | |||
| pmid = 2403650 | |||
}}</ref> | |||
* The [[relative risk]] of non-Hodgkin lymphoma increases among Hodgkin lymphoma survivors, and this risk increases with follow-up time. <ref>{{Cite journal | |||
| author = [[M. Henry-Amar]] | |||
| title = Second cancer after the treatment for Hodgkin's disease: a report from the International Database on Hodgkin's Disease | |||
| journal = [[Annals of oncology : official journal of the European Society for Medical Oncology]] | |||
| volume = 3 Suppl 4 | |||
| pages = 117–128 | |||
| year = 1992 | |||
| month = September | |||
| pmid = 1450072 | |||
}}</ref> <ref>{{Cite journal | |||
| author = [[F. E. van Leeuwen]], [[W. J. Klokman]], [[M. B. Veer]], [[A. Hagenbeek]], [[A. D. Krol]], [[U. A. Vetter]], [[M. Schaapveld]], [[P. van Heerde]], [[J. M. Burgers]], [[R. Somers]] & [[B. M. Aleman]] | |||
| title = Long-term risk of second malignancy in survivors of Hodgkin's disease treated during adolescence or young adulthood | |||
| journal = [[Journal of clinical oncology : official journal of the American Society of Clinical Oncology]] | |||
| volume = 18 | |||
| issue = 3 | |||
| pages = 487–497 | |||
| year = 2000 | |||
| month = February | |||
| doi = 10.1200/JCO.2000.18.3.487 | |||
| pmid = 10653864 | |||
}}</ref> | |||
==Prognosis== | ==Prognosis== | ||
===Prognostic factors for early Hodgkin's lymphoma<ref | ===Prognostic factors for early (Stage I and II) Hodgkin's lymphoma<ref>Hodgkin-lymphoma. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/hodgkin-lymphoma/diagnosis/?region=ab Accessed on September 16, 2015</ref>=== | ||
* | * Hodgkin lymphoma is considered as curable cancer, with stages I and II considered early stage. In addition, other [[clinical]] [[Features (pattern recognition)|features]], such as age, absence or presence of [[B symptoms]], number of involved sites, and size of [[lymphadenopathy]] are used by experts to stratify Hodgkin's lymphoma into favorable and unfavorable subtypes. | ||
=== | ====== The definitions of favorable disease are proposed by the European Organization for the Research and Treatment of Cancer (EORTC) are following:<ref>{{Cite journal | ||
| author = [[J. M. Cosset]], [[M. Henry-Amar]], [[J. H. Meerwaldt]], [[P. Carde]], [[E. M. Noordijk]], [[J. Thomas]], [[J. M. Burgers]], [[R. Somers]], [[M. Hayat]] & [[M. Tubiana]] | |||
| title = The EORTC trials for limited stage Hodgkin's disease. The EORTC Lymphoma Cooperative Group | |||
| journal = [[European journal of cancer (Oxford, England : 1990)]] | |||
| volume = 28A | |||
| issue = 11 | |||
| pages = 1847–1850 | |||
| year = 1992 | |||
| month = | |||
| pmid = 1389523 | |||
}}</ref> ====== | |||
* Under 50 years old | |||
* No large [[Mediastinum|mediastinal]] [[Lymphadenopathy|adenopathy]] | |||
* [[Erythrocyte sedimentation rate|ESR]] of less than 50 mm/h and no [[B symptoms]] (or an ESR of less than 30 mm/h with B symptoms) | |||
* Disease limited to three or fewer regions of involvement | |||
====== The criteria are used by the German Hodgkin Study Group (GHSG) for definitions of favorable disease include:<ref>{{Cite journal | |||
| author = [[Andreas Engert]], [[Annette Plutschow]], [[Hans Theodor Eich]], [[Andreas Lohri]], [[Bernd Dorken]], [[Peter Borchmann]], [[Bernhard Berger]], [[Richard Greil]], [[Kay C. Willborn]], [[Martin Wilhelm]], [[Jurgen Debus]], [[Michael J. Eble]], [[Martin Sokler]], [[Antony Ho]], [[Andreas Rank]], [[Arnold Ganser]], [[Lorenz Trumper]], [[Carsten Bokemeyer]], [[Hartmut Kirchner]], [[Jorg Schubert]], [[Zdenek Kral]], [[Michael Fuchs]], [[Hans-Konrad Muller-Hermelink]], [[Rolf-Peter Muller]] & [[Volker Diehl]] | |||
| title = Reduced treatment intensity in patients with early-stage Hodgkin's lymphoma | |||
: | | journal = [[The New England journal of medicine]] | ||
| volume = 363 | |||
| issue = 7 | |||
| pages = 640–652 | |||
| year = 2010 | |||
| month = August | |||
| doi = 10.1056/NEJMoa1000067 | |||
| pmid = 20818855 | |||
}}</ref> ====== | |||
* No more than two sites of involvement | |||
* No extranodal extension | |||
* No [[mediastinal mass]] measuring one-third the maximum thoracic diameter or greater | |||
* [[Erythrocyte sedimentation rate|ESR]] less than 50 mm/h (less than 30 mm/h if [[B symptoms]] present) | |||
* | |||
===Prognostic factors in advanced (stage III and IV) Hodgkin's lymphoma=== | |||
The International Prognostic Score (IPS) is the most commonly used risk stratification system for patients with advanced-stage disease (stages III and IV), which uses the following seven potential unfavorable features at diagnosis: <ref>{{Cite journal | |||
| author = [[Alden A. Moccia]], [[Jane Donaldson]], [[Mukesh Chhanabhai]], [[Paul J. Hoskins]], [[Richard J. Klasa]], [[Kerry J. Savage]], [[Tamara N. Shenkier]], [[Graham W. Slack]], [[Brian Skinnider]], [[Randy D. Gascoyne]], [[Joseph M. Connors]] & [[Laurie H. Sehn]] | |||
| title = International Prognostic Score in advanced-stage Hodgkin's lymphoma: altered utility in the modern era | |||
| journal = [[Journal of clinical oncology : official journal of the American Society of Clinical Oncology]] | |||
| volume = 30 | |||
| issue = 27 | |||
| pages = 3383–3388 | |||
| year = 2012 | |||
| month = September | |||
| doi = 10.1200/JCO.2011.41.0910 | |||
| pmid = 22869887 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[D. Hasenclever]] & [[V. Diehl]] | |||
| title = A prognostic score for advanced Hodgkin's disease. International Prognostic Factors Project on Advanced Hodgkin's Disease | |||
| journal = [[The New England journal of medicine]] | |||
| volume = 339 | |||
| issue = 21 | |||
| pages = 1506–1514 | |||
| year = 1998 | |||
| month = November | |||
| doi = 10.1056/NEJM199811193392104 | |||
| pmid = 9819449 | |||
}}</ref> | |||
* [[Serum albumin]] <4 g/dL | |||
* [[Hemoglobin]] <10.5 g/dL | |||
* Male gender | |||
* Age >45 years | |||
* Stage IV disease | |||
* [[White blood cells|White blood cell]] count ≥15,000/microL | |||
* Absolute [[lymphocyte]] count <600/microL and/or <8 percent of the total white blood cell count | |||
Each variable is assigned 1 point and the total score is inversely related to 5-year survival rates as follows: | |||
# No point : 84 percent | |||
# One points : 77 percent | |||
# Two points : 67 percent | |||
# Three points : 60 percent | |||
# Four points : 51 percent | |||
# Five or more points : 42 percent | |||
===5-Year Survival=== | ===5-Year Survival=== | ||
| Line 43: | Line 223: | ||
* When stratified by age, the 5-year relative survival of patients with Hodgkin's lymphoma was 90.5% and 52.8% for patients <65 and ≥ 65 years of age respectively.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | * When stratified by age, the 5-year relative survival of patients with Hodgkin's lymphoma was 90.5% and 52.8% for patients <65 and ≥ 65 years of age respectively.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | ||
* The survival of patients with Hodgkin's lymphoma varies with the stage of the disease. | * The survival of patients with Hodgkin's lymphoma varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of Hodgkin's lymphoma:<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | ||
{| style="cellpadding=0; cellspacing= 0; width: 600px;" | {| style="cellpadding=0; cellspacing= 0; width: 600px;" | ||
|- | |- | ||
|style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align=center |'''Stage'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align=center | '''5-year relative survival (%), (2004-2010)''' | | style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Stage'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" | '''5-year relative survival (%), (2004-2010)''' | ||
|- | |- | ||
| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align=left |'''All stages'''|| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align=left |85.3% | | style="font-size: 100; padding: 0 5px; background: #e4e4e4" align="left" |'''All stages'''|| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align="left" |85.3% | ||
|- | |- | ||
| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align=left |'''Localized'''|| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align=left | | style="font-size: 100; padding: 0 5px; background: #e4e4e4" align="left" |'''Localized'''|| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align="left" |90.8% | ||
|- | |- | ||
| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align=left |'''Regional'''|| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align=left |92.1% | | style="font-size: 100; padding: 0 5px; background: #e4e4e4" align="left" |'''Regional'''|| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align="left" |92.1% | ||
|- | |- | ||
| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align=left | | style="font-size: 100; padding: 0 5px; background: #e4e4e4" align="left" |'''Distant'''|| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align="left" |76.2% | ||
|- | |- | ||
| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align=left | | style="font-size: 100; padding: 0 5px; background: #e4e4e4" align="left" |'''Unstaged'''|| style="font-size: 100; padding: 0 5px; background: #e4e4e4" align="left" |80.7% | ||
|} | |} | ||
* The survival of patients with Hodgkin's lymphoma also varies with the subtype of Hodgkin's lymphoma. | * The survival of patients with Hodgkin's lymphoma also varies with the subtype of Hodgkin's lymphoma. Shown below is the 5-year relative survival by the subtype of Hodgkin's lymphoma:<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | ||
** Classical Hodgkin's lymphoma: 84.8% | ** Classical Hodgkin's lymphoma: 84.8% | ||
***Lymphocyte-rich: 87.1% | ***Lymphocyte-rich: 87.1% | ||
| Line 75: | Line 255: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
[[Category:Disease]] | [[Category:Disease]] | ||
| Line 82: | Line 264: | ||
[[Category:Mature chapter]] | [[Category:Mature chapter]] | ||
[[Category:Needs content]] | [[Category:Needs content]] | ||
Latest revision as of 22:13, 29 July 2020
|
Hodgkin's lymphoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hodgkin's lymphoma natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Hodgkin's lymphoma natural history, complications and prognosis |
|
FDA on Hodgkin's lymphoma natural history, complications and prognosis |
|
CDC on Hodgkin's lymphoma natural history, complications and prognosis |
|
Hodgkin's lymphoma natural history, complications and prognosis in the news |
|
Blogs on Hodgkin's lymphoma natural history, complications and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sowminya Arikapudi, M.B,B.S. [2] Mohsen Basiri M.D.
Overview
Hodgkin's lymphoma has a bimodal age distribution and both children and adult may be affected. The early peak occurs in the middle-to-late 20's and the second peak after the age of 50. Treatment outcomes of Hodgkin’s lymphoma are excellent and five-year survival rates are more than 80%. Owing to modern therapies, the natural history of untreated Hodgkin’s lymphoma is actually difficult to determine. Survivors are at risk for relapse, second primary malignancies, cardiovascular complications and other treatment-related toxicities. Prognosis is based on the stage of the disease and other prognostic factors. The early stage of the Hodgkin's lymphoma is associated with the most favorable prognosis and the 5-year survival rate of patients with Hodgkin's lymphoma varies with the stage of the disease.
Natural History
- Hodgkin's lymphoma has a bimodal age distribution and both children and adult may be affected. The most common symptom of classic Hodgkin's lymphoma includes painless localized peripheral lymphadenopathy.
- Owing to modern therapies, the natural history of untreated Hodgkin’s lymphoma is actually difficult to determine.
- If left untreated, Hodgkin's lymphoma develop complications depend on site and size of mass, including breathing problem, hypoxemia, chest pain, significant weight loss, and a tracheoesophageal fistula and eventually significant decrease in the overall survival.[1]
Complications
- The main complications of Hodgkin lymphoma are due to side effects of chemotherapy and/or radiotherapy, table below provides these general side effects:
| Complications of Chemotherapy[2] | Complications of Radiotherapy[2] |
| Skin reactions | Skin changes |
| Nausea and vomiting | Nausea and vomiting |
| Sore throat and painful swallowing | Sore mouth |
| Taste changes | Loss of appetite |
| Fatigue | Fatigue |
| Diarrhea | Diarrhea |
| Bone marrow suppression | Bone marrow suppression |
| Dental cavities | Constipation |
| Thyroid problems | Hair loss |
| Fertility problems | Cystitis |
| Heart and lung problems | Muscle and joint pain |
| Second cancers | Second cancers |
| Pain at the injection site | |
| Inflammation of the vein | |
| Allergic reactions | |
| Organ damage | |
| Fluid retention |
- Leading complications in Hodgkin lymphoma survivors are second primary malignancies and cardiovascular toxicities. Cardiovascular complications of radiation therapy (RT) include pericarditis, myocardial ischemia or infarction, cardiomyopathy, heart failure, valvular abnormalities, or conduction abnormalities. [3][4]
- Breast, lung, and colon cancer are the majority of second cancers in Hodgkin’s lymphoma survivors. [5]
- Leukemia and non-Hodgkin lymphoma (NHL) are less common. Most leukemias that occur after the treatment are acute myeloid leukemia (AML) related to alkylating agent exposure. [6]
- The relative risk of non-Hodgkin lymphoma increases among Hodgkin lymphoma survivors, and this risk increases with follow-up time. [7] [8]
Prognosis
Prognostic factors for early (Stage I and II) Hodgkin's lymphoma[9]
- Hodgkin lymphoma is considered as curable cancer, with stages I and II considered early stage. In addition, other clinical features, such as age, absence or presence of B symptoms, number of involved sites, and size of lymphadenopathy are used by experts to stratify Hodgkin's lymphoma into favorable and unfavorable subtypes.
The definitions of favorable disease are proposed by the European Organization for the Research and Treatment of Cancer (EORTC) are following:[10]
- Under 50 years old
- No large mediastinal adenopathy
- ESR of less than 50 mm/h and no B symptoms (or an ESR of less than 30 mm/h with B symptoms)
- Disease limited to three or fewer regions of involvement
The criteria are used by the German Hodgkin Study Group (GHSG) for definitions of favorable disease include:[11]
- No more than two sites of involvement
- No extranodal extension
- No mediastinal mass measuring one-third the maximum thoracic diameter or greater
- ESR less than 50 mm/h (less than 30 mm/h if B symptoms present)
Prognostic factors in advanced (stage III and IV) Hodgkin's lymphoma
The International Prognostic Score (IPS) is the most commonly used risk stratification system for patients with advanced-stage disease (stages III and IV), which uses the following seven potential unfavorable features at diagnosis: [12][13]
- Serum albumin <4 g/dL
- Hemoglobin <10.5 g/dL
- Male gender
- Age >45 years
- Stage IV disease
- White blood cell count ≥15,000/microL
- Absolute lymphocyte count <600/microL and/or <8 percent of the total white blood cell count
Each variable is assigned 1 point and the total score is inversely related to 5-year survival rates as follows:
- No point : 84 percent
- One points : 77 percent
- Two points : 67 percent
- Three points : 60 percent
- Four points : 51 percent
- Five or more points : 42 percent
5-Year Survival
- Between 2004 and 2010, the 5-year relative survival of patients with Hodgkin's lymphoma was 87.7%.[14]
- When stratified by age, the 5-year relative survival of patients with Hodgkin's lymphoma was 90.5% and 52.8% for patients <65 and ≥ 65 years of age respectively.[14]
- The survival of patients with Hodgkin's lymphoma varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of Hodgkin's lymphoma:[14]
| Stage | 5-year relative survival (%), (2004-2010) |
| All stages | 85.3% |
| Localized | 90.8% |
| Regional | 92.1% |
| Distant | 76.2% |
| Unstaged | 80.7% |
- The survival of patients with Hodgkin's lymphoma also varies with the subtype of Hodgkin's lymphoma. Shown below is the 5-year relative survival by the subtype of Hodgkin's lymphoma:[14]
- Classical Hodgkin's lymphoma: 84.8%
- Lymphocyte-rich: 87.1%
- Mixed cellularity: 80%
- Lymphocyte-depleted: 56.6%
- Nodular sclerosis: 89.4%
- Classical Hodgkin's lymphoma not otherwise specified: 75.2%
- Nodular lymphocyte predominant Hodgkin's lymphoma: 95.3%
- Classical Hodgkin's lymphoma: 84.8%
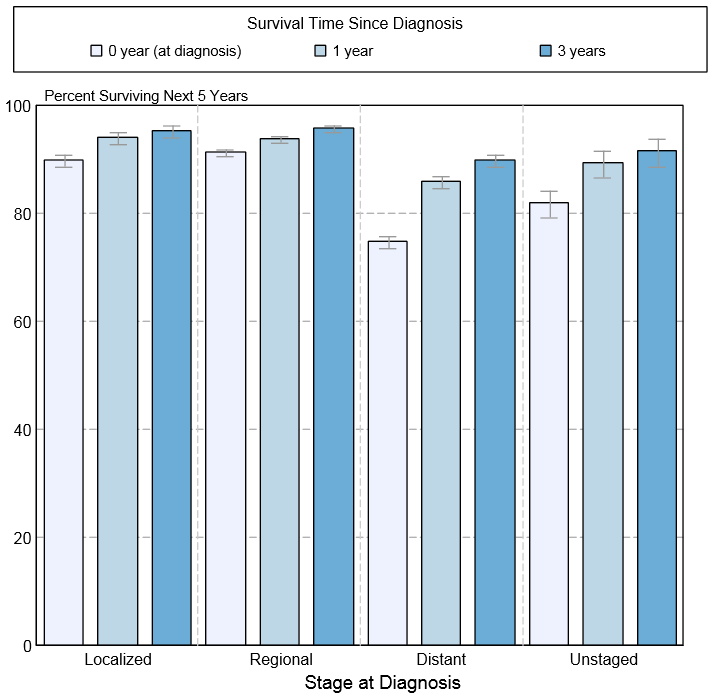
- Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of Hodgkin's lymphoma by stage at diagnosis according to SEER. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[14]
References
- ↑ Greco, Ralph S. (1974). "Hodgkin Disease in Connecticut From 1935 to 1962". Archives of Internal Medicine. 134 (6): 1039. doi:10.1001/archinte.1974.00320240073007. ISSN 0003-9926.
- ↑ 2.0 2.1 Hodgkin-lymphoma. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/hodgkin-lymphoma/treatment/?region=ab Accessed on September 10, 2015
- ↑ Shira L. Galper, James B. Yu, Peter M. Mauch, Jon F. Strasser, Barbara Silver, Ann Lacasce, Karen J. Marcus, Mary Ann Stevenson, Ming Hui Chen & Andrea K. Ng (2011). "Clinically significant cardiac disease in patients with Hodgkin lymphoma treated with mediastinal irradiation". Blood. 117 (2): 412–418. doi:10.1182/blood-2010-06-291328. PMID 20858859. Unknown parameter
|month=ignored (help) - ↑ Andrea K. Ng, Ann LaCasce & Lois B. Travis (2011). "Long-term complications of lymphoma and its treatment". Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 29 (14): 1885–1892. doi:10.1200/JCO.2010.32.8427. PMID 21483015. Unknown parameter
|month=ignored (help) - ↑ Michael Schaapveld, Berthe M. P. Aleman, Anna M. van Eggermond, Cecile P. M. Janus, Augustinus D. G. Krol, Richard W. M. van der Maazen, Judith Roesink, John M. M. Raemaekers, Jan Paul de Boer, Josee M. Zijlstra, Gustaaf W. van Imhoff, Eefke J. Petersen, Philip M. P. Poortmans, Max Beijert, Marnix L. Lybeert, Ina Mulder, Otto Visser, Marieke W. J. Louwman, Inge M. Krul, Pieternella J. Lugtenburg & Flora E. van Leeuwen (2015). "Second Cancer Risk Up to 40 Years after Treatment for Hodgkin's Lymphoma". The New England journal of medicine. 373 (26): 2499–2511. doi:10.1056/NEJMoa1505949. PMID 26699166. Unknown parameter
|month=ignored (help) - ↑ J. M. Kaldor, N. E. Day, E. A. Clarke, F. E. Van Leeuwen, M. Henry-Amar, M. V. Fiorentino, J. Bell, D. Pedersen, P. Band & D. Assouline (1990). "Leukemia following Hodgkin's disease". The New England journal of medicine. 322 (1): 7–13. doi:10.1056/NEJM199001043220102. PMID 2403650. Unknown parameter
|month=ignored (help) - ↑ M. Henry-Amar (1992). "Second cancer after the treatment for Hodgkin's disease: a report from the International Database on Hodgkin's Disease". Annals of oncology : official journal of the European Society for Medical Oncology. 3 Suppl 4: 117–128. PMID 1450072. Unknown parameter
|month=ignored (help) - ↑ F. E. van Leeuwen, W. J. Klokman, M. B. Veer, A. Hagenbeek, A. D. Krol, U. A. Vetter, M. Schaapveld, P. van Heerde, J. M. Burgers, R. Somers & B. M. Aleman (2000). "Long-term risk of second malignancy in survivors of Hodgkin's disease treated during adolescence or young adulthood". Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 18 (3): 487–497. doi:10.1200/JCO.2000.18.3.487. PMID 10653864. Unknown parameter
|month=ignored (help) - ↑ Hodgkin-lymphoma. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/hodgkin-lymphoma/diagnosis/?region=ab Accessed on September 16, 2015
- ↑ J. M. Cosset, M. Henry-Amar, J. H. Meerwaldt, P. Carde, E. M. Noordijk, J. Thomas, J. M. Burgers, R. Somers, M. Hayat & M. Tubiana (1992). "The EORTC trials for limited stage Hodgkin's disease. The EORTC Lymphoma Cooperative Group". European journal of cancer (Oxford, England : 1990). 28A (11): 1847–1850. PMID 1389523.
- ↑ Andreas Engert, Annette Plutschow, Hans Theodor Eich, Andreas Lohri, Bernd Dorken, Peter Borchmann, Bernhard Berger, Richard Greil, Kay C. Willborn, Martin Wilhelm, Jurgen Debus, Michael J. Eble, Martin Sokler, Antony Ho, Andreas Rank, Arnold Ganser, Lorenz Trumper, Carsten Bokemeyer, Hartmut Kirchner, Jorg Schubert, Zdenek Kral, Michael Fuchs, Hans-Konrad Muller-Hermelink, Rolf-Peter Muller & Volker Diehl (2010). "Reduced treatment intensity in patients with early-stage Hodgkin's lymphoma". The New England journal of medicine. 363 (7): 640–652. doi:10.1056/NEJMoa1000067. PMID 20818855. Unknown parameter
|month=ignored (help) - ↑ Alden A. Moccia, Jane Donaldson, Mukesh Chhanabhai, Paul J. Hoskins, Richard J. Klasa, Kerry J. Savage, Tamara N. Shenkier, Graham W. Slack, Brian Skinnider, Randy D. Gascoyne, Joseph M. Connors & Laurie H. Sehn (2012). "International Prognostic Score in advanced-stage Hodgkin's lymphoma: altered utility in the modern era". Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 30 (27): 3383–3388. doi:10.1200/JCO.2011.41.0910. PMID 22869887. Unknown parameter
|month=ignored (help) - ↑ D. Hasenclever & V. Diehl (1998). "A prognostic score for advanced Hodgkin's disease. International Prognostic Factors Project on Advanced Hodgkin's Disease". The New England journal of medicine. 339 (21): 1506–1514. doi:10.1056/NEJM199811193392104. PMID 9819449. Unknown parameter
|month=ignored (help) - ↑ 14.0 14.1 14.2 14.3 14.4 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.