Goitre (patient information)
For the WikiDoc page for this topic, click here
| Goitre (patient information) | |
 | |
|---|---|
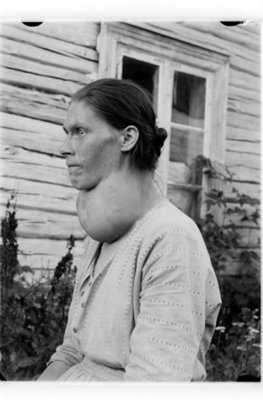
| a woman with a goitre | |
| ICD-10 | E01.0-E01.2 |
| ICD-9 | 240.9 |
| DiseasesDB | 5332 |
| MedlinePlus | 001178 |
| MeSH | Goiter |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Jinhui Wu, MD
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
What is goitre?
How do I know if I have Goitre and what are the symptoms of goitre?
Not all goiters cause signs and symptoms. When symptoms do occur they may include:
- A visible swelling at the base of your neck, the size may range from a single small nodule to large neck lump.
- A tight feeling in your throat
- Cough
- Hoarseness
- Difficulty swallowing
- Shortness of breath
- Fatigue
- Increased appetite
- Nervousness
- Restlessness
- Weight loss
- Muscle cramps
Who is at risk for goitre?
Goiters can affect anyone. Some common risk factors for goiter include:
- A lack of dietary iodine: Epidemical data show that people living in areas lack of iodine and not getting enough iodine in the diet are at high risk of goiter.
- Female gender: Studies demonstrate that women are more likely to thyroid disorders than men.
- Age over 50 years
- Personnal or family history: A personal or family history of autoimmune disease increases your risk.
- Certain medications: Some drugs, such as immunosuppressants, antiretrovirals, amiodarone for arrhythmia and lithium for psychiatric disorders, may increase the risk of developing goitre.
- Radiation: Clinical surveys demonstrate the risk increases when patients have been treated with radiation to the neck or chest area, even when they have been exposed to radiation in a nuclear facility, test or accident.
How to know you have goitre?
- Blood hormone level tests: Blood tests of thyroid hormone can determine the function of thyroid and pituitary glands. Usually, serum thyroid hormone levels (T3, T4) and serum thyroid-stimulating hormone (TSH) are detected. Goiter associated with an overactive thyroid usually involves a high level of thyroid hormone and a lower than normal TSH level in the blood.
- An antibody test: For some causes of goiter such as Hashimoto's thyroiditis and Graves-Basedow disease, a blood test about antibodies may be helpful to the diagnosis.
- Ultrasonography: This is an painless test which uses sound waves to create a picture of the internal organs. During the test, a transducer is put over your neck to form images on a computer screen. The images can tell the size of thyroid gland and whether the gland contains nodules inside.
- Thyroid scans: This is a nuclear medicine test. During the test, a radioactive isotope is injected into the patient's vein. Then, a special camera produces an image of the thyroid on a computer screen. Thyroid scans can provide information about the nature and size of your thyroid.
When to seek urgent medical care?
Call your health care provider if you have symptoms of this disorder. Follow the health care provider's recommendations for follow-up visits.
Treatment options
Goiter treatment depends on the cause, the size of the goiter, patient's signs and symptoms. Usual treatments include medications, surgery and radioactive iodine.
- Observation: An observation approach is recommended for patient whose goiter is small, and doesn't cause problems, and blood hormone tests are normal.
- Medications:
- Iodine deficiency: For those that the goiter is due to iodine deficiency, Lugol's iodine or potassium iodine solution may be recommended.
- Hypothyroidism: If the goiter is due to underactive thyroid, treatment is thyroid hormone supplements. :*Thyroid gland inflammation: For patients with thyroid gland inflammation, aspirin or corticosteroid are needed.
- Hyperthyroidism: For goiters associated with hyperthyroidism, antithyroid drugs such as propylthiouracil and methimazole may need to control hormone levels.
- Surgery: Removing all or part of your thyroid gland (total or partial thyroidectomy) is an option if you have a large goiter that is uncomfortable or causes difficulty breathing or swallowing, or in some cases, if you have nodular goiter causing hyperthyroidism. Surgery is also the treatment for thyroid cancer. You may need to take levothyroxine after surgery, depending on the amount of thyroid removed.
- Radioactive iodine: In some cases, radioactive iodine is used to treat an overactive thyroid gland. The radioactive iodine is taken orally and reaches your thyroid gland through your bloodstream, destroying thyroid cells. The treatment results in diminished size of the goiter but eventually may also cause an underactive thyroid gland. Hormone replacement with the synthetic thyroid hormone levothyroxine then becomes necessary, usually for life.
Diseases with similar symptoms
Where to find medical care for goitre?
Directions to Hospitals Treating goitre
Prevention of goitre
What to expect (Outook/Prognosis)?
Prognosis of goitre depends on the causes of the disease. The outcome of goitre caused by the thyroid cancer is worse than prognosis caused by other diseases, such as Graves' disease, Hashimoto's disease and iodine deficiency.
Copyleft Sources
http://www.mayoclinic.com/print/goiter/DS00217/DSECTION=all&METHOD=print
http://www.nlm.nih.gov/medlineplus/ency/article/001178.htm