Giardia lamblia: Difference between revisions
| Line 91: | Line 91: | ||
==Treatment== | ==Treatment== | ||
===Antimicrobial Regimen=== | ===Antimicrobial Regimen=== | ||
*Giardia lamblia | *Giardia lamblia<ref>{{cite book | last = Bennett | first = John | title = Mandell, Douglas, and Bennett's principles and practice of infectious diseases | publisher = Elsevier/Saunders | location = Philadelphia, PA | year = 2015 | isbn = 978-1455748013 }}</ref> | ||
:*Preferred regimen(1): | :*Preferred regimen(1): | ||
::*Adult: [[Tinidazole]] 2 g, single dose | ::*Adult: [[Tinidazole]] 2 g, single dose | ||
Revision as of 19:09, 29 June 2015
| Giardia lamblia | ||||||||
|---|---|---|---|---|---|---|---|---|
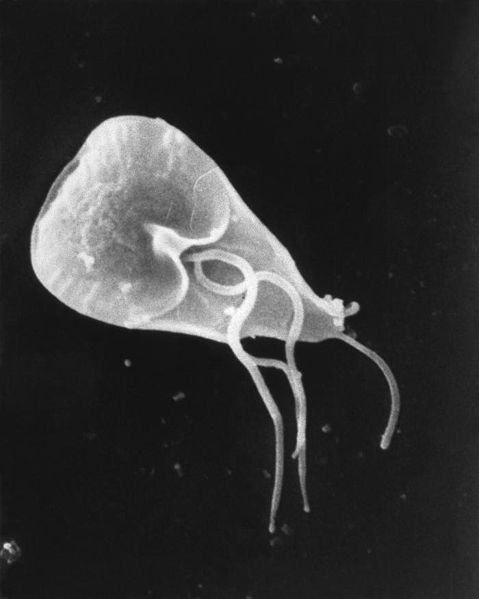 Giardia cell, SEM
| ||||||||
| Scientific classification | ||||||||
| ||||||||
| Binomial name | ||||||||
| Giardia lamblia (Kunstler, 1882) |
|
WikiDoc Resources for Giardia lamblia |
|
Articles |
|---|
|
Most recent articles on Giardia lamblia Most cited articles on Giardia lamblia |
|
Media |
|
Powerpoint slides on Giardia lamblia |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Giardia lamblia at Clinical Trials.gov Trial results on Giardia lamblia Clinical Trials on Giardia lamblia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Giardia lamblia NICE Guidance on Giardia lamblia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Giardia lamblia Discussion groups on Giardia lamblia Patient Handouts on Giardia lamblia Directions to Hospitals Treating Giardia lamblia Risk calculators and risk factors for Giardia lamblia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Giardia lamblia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Overview
Giardia lamblia (synonymous with Lamblia intestinalis and Giardia duodenalis) is a flagellated protozoan parasite that colonises and reproduces in the small intestine, causing giardiasis. The giardia parasite attaches to the epithelium by a ventral adhesive disc, and reproduces via binary fission[1]. Giardiasis does not disseminate haematogenously, nor does it spread to other parts of the gastro-intestinal tract, but remains confined to the lumen of the small intestine[2]. Giardia trophozoites absorb their nutrients from the lumen of the small intestine, and are anaerobes.
Hosts
Giardia affects humans, but Giardia is also one of the most common parasites infecting cats and dogs. Mammalian hosts also include cows, beavers, deer, and sheep.
Life cycle

Giardia belongs among the diplomonads.
Giardia infection can occur through ingestion of dormant cysts in contaminated water, or by the faecal-oral route (through poor hygiene practices). The Giardia cyst can survive for weeks to months in cold water[3], and therefore can be present in contaminated wells and water systems, and even clean-looking mountain streams, as well as city reservoirs, as the Giardia cysts are resistant to conventional water treatment methods, such as chlorination and ozonolysis.[3] Zoonotic transmission is also possible, and therefore Giardia infection is a concern for people camping in the wilderness or swimming in contaminated streams or lakes, especially the artificial lakes formed by beaver dams (hence the popular name for giardiasis, "Beaver Fever").
As well as water-borne sources, faecal-oral transmission can also occur, for example in day care centres, where children may have poorer hygiene practices. Those who work with children are also at risk of being infected, as are family members of infected individuals. Not all Giardia infections are symptomatic, so some people can unknowingly serve as carriers of the parasite.
The life cycle begins with a noninfective cyst being excreted with faeces of an infected individual. Once out in the environment, the cyst becomes infective. A distinguishing characteristic of the cyst is 4 nuclei and a retracted cytoplasm. Once ingested by a host, the trophozoite emerges to an active state of feeding and motility. After the feeding stage, the trophozoite undergoes asexual replication through longitudinal binary fission. The resulting trophozoites and cysts then pass through the digestive system in the faeces. While the trophozoites may be found in the faeces, only the cysts are capable of surviving outside of the host.
Distinguishing features of the trophozoites are large karyosomes and lack of peripheral chromatin, giving the two nuclei a halo appearance. Cysts are distinguished by a retracted cytoplasm. This protozoa lacks mitochondria, although the discovery of the presence of mitochodrial remnant organelles in one recent study "indicate that Giardia is not primitively amitochondrial and that it has retained a functional organelle derived from the original mitochondrial endosymbiont"[4]
Manifestation of Infection
Nomenclature for Giardia species are difficult, as humans and other animals appear to have morphologically identical parasites.
Colonisation of the gut results in inflammation and villous atrophy, reducing the gut's absorptive capability. In humans, infection is symptomatic only about 50% of the time, and protocol for treating asymptomatic individuals is controversial.[3] Symptoms of infection include (in order of frequency) diarrhea, malaise, excessive gas (often flatulence or a foul or sulphuric-tasting belch, which has been known to be so nauseating in taste that it can cause the infected person to vomit), steatorrhoea (pale, foul smelling, greasy stools), epigastric pain, bloating, nausea, diminished interest in food, possible (but rare) vomiting which is often violent, and weight loss.[3] Pus, mucus and blood are not commonly present in the stool. In healthy individuals, the condition is usually self-limiting, although the infection can be prolonged in patients who are immunocompromised, or who have decreased gastric acid secretion.[3] People with recurring Giardia infections, particularly those with a lack of IgA, may develop chronic disease. Lactase deficiency may develop in an infection with Giardia, however this usually does not persist for more than a few weeks, and a full recovery is the norm.
Cats can be cured easily, lambs usually simply lose weight, but in calves the parasites can be fatal and often are not responsive to antibiotics or electrolytes. Carriers among calves can also be asymptomatic. Dogs have a high infection rate, as 30% of the population under one year old are known to be infected in kennels. The infection is more prevalent in puppies than in adult dogs. This parasite is deadly for chinchillas, so extra care must be taken by providing them with safe water. Infected dogs can be isolated and treated, or the entire pack at a kennel can be treated together regardless. Kennels should also be then cleaned with bleach or other cleaning disinfectants. The grass areas used for exercise should be considered contaminated for at least one month after dogs show signs of infection, as cysts can survive in the environment for long periods of time. Prevention can be achieved by quarantine of infected dogs for at least 20 days and careful management and maintenance of a clean water supply.
Prevention and Treatment
Treatment of drinking water for Giardia typically involves high efficiency filtration and/or chemical disinfection such as chlorination or ozonation. However, normal concentrations of chlorine and ozone used in mass water treatment are not adequate to kill the cysts. Scooping water from the top of a stream or river is not an effective way to avoid Giardia. Filtering (<1ųm pore) or boiling is recommended for purification of drinking water in wilderness conditions.
A Giardia lamblia infection in humans is diagnosed with an antigen test or, if that is unavailable, an ova and parasite examination of stool. Multiple stool examinations are recommended, since the cysts and trophozoites are not shed consistently.
Human infection is conventionally treated with metronidazole, tinidazole or nitazoxonide. Although Metronidazole is the current first-line therapy, it is mutagenic in bacteria and carcinogenic in mice, so should be avoided during pregnancy.[3] One of the most common alternative treatments is berberine sulfate (found in Oregon grape root, goldenseal, yellowroot, and various other plants). Berberine has been shown to have an antimicrobial and an antipyretic effect. Berberine compounds cause uterine stimulation, and so should be avoided in pregnancy. High doses of berberine can cause bradycardia and hypotension. [5]
| Drug | Treatment duration | Possible Side Effects |
|---|---|---|
| Metronidazole | 5-7 days | Metallic taste; nausea; vomiting; dizziness; headache; disulfiram-like effect; neutropenia |
| Tinidazole | Single dose | Metallic taste; nausea; vomiting; belching; dizziness; headache; disulfiram-like effect |
| Nitazoxanide | 3 days | Abdominal pain; diarrhoea; vomiting; headache; yellow-green discolouration of urine |
Table adapted from Huang, White..[3]
Microscopy
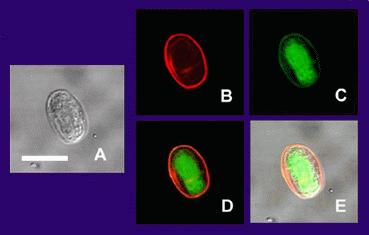
(A) is the cyst imaged by transmission (differential interference contrast), only.
(B) is the cyst wall selectively imaged through use of fluorescent-labelled (TRITC) antibody that is cyst wall specific.
(C) is the cyst imaged through use of carboxy fluorescein diacetate, a viability stain.
(D) is a composite image of (B) and (C).
(E) is a composite image of (A), (B), and (C).
Under a normal compound light microscope, Giardia often looks like a "clown face," with two nuclei outlined by adhesive discs above dark median bodies that form the "mouth." Cysts have four nuclei.
Research
Giardia alternates between two different forms — a hardy, dormant cyst that contaminates water or food and an active, disease-causing form that emerges after the parasite is ingested. National Institute of General Medical Sciences grantee Dr. Frances Gillin of the University of California, San Diego and her colleagues cultivated the entire life cycle of this parasite in the laboratory, and identified biochemical cues in the host's digestive system which trigger Giardia's life cycle transformations.[6][7] They also uncovered several ways in which the parasite evades the defences of the infected organism. One of these is by altering the proteins on its surface, which confounds the ability of the infected animal's immune system to detect and combat the parasite (called antigenic variation). Gillin's work reveals why Giardia infections are extremely persistent and prone to recur. In addition, these insights into Giardias biology and survival techniques may enable scientists to develop better strategies to understand, prevent, and treat giardia infections.
History
The trophozoite form of Giardia was first observed in 1681 by Antoni van Leeuwenhoek in his own diarrheal stools. In 1915, the parasite was named in honour of Professor A. Giard of Paris. His observations were recreated, using a single lensed microscope of the kind used by Leeuwenhoek, by British microbiologist Brian J. Ford who showed how clearly one could view Giardia through a primitive microscope.[8]
In 1998, there was a Giardia outbreak in Sydney, Australia that was found to be due to contamination of the water supply. This was ameliorated with improved water treatment.
A similar outbreak took place in Oslo, Norway in October 2007. The outbreak was also found to be due to contamination of the water supply.
Treatment
Antimicrobial Regimen
- Giardia lamblia[9]
- Preferred regimen(1):
- Adult: Tinidazole 2 g, single dose
- Pediatric: Tinidazole 50 mg/kg, single dose (maximum, 2 g)
- Preferred regimen(2):
- Adult: Metronidazole 250 mg tid for 5-7 days
- Pediatric: Metronidazole 5 mg/kg tid for 7 days
- Preferred regimen(3):
- Adult: Nitazoxanide 500 mg bid for 3 days
- Pediatric: Nitazoxanide Age 12-47 months: 100 mg bid for 3 days and for Age 4-11 years: 200 mg bid for 3 days
- Preferred regimen(4):
- Adult: Albendazole 400 mg qd for 5 days
- Pediatric: Albendazole 15 mg/kg/day for 5-7 days (maximum, 400 mg)
- Preferred regimen(5):
- Adult: Paromomycin 500 mg tid for 5-10 days
- Pediatric: Paromomycin 30 mg/kg/day in 3 doses for 5-10 days
- Preferred regimen(6):
- Adult: Quinacrine 100 mg tid for 5-7 days
- Pediatric: Quinacrine 2 mg/kg tid for 7 days
- Preferred regimen(7):
- Adult: Furazolidone 100 mg qid for 7-10 days
- Pediatric: Furazolidone 2 mg/kg qid for 10 days
References
- ↑ Oxford textbook of Medicine, Fourth Edition, Volume 1. Oxford University Press pp759-760
- ↑ Harrison's Internal Medicine, Harrison's Online Chapter 199 Protozoal intestinal infections and trochomoniasis
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Huang DB, White AC (2006). "An updated review on Cryptosporidium and Giardia". Gastroenterol. Clin. North Am. 35 (2): 291–314, viii. doi:10.1016/j.gtc.2006.03.006. PMID 16880067.
- ↑ Tovar J, León-Avila G, Sánchez LB; et al. (2003). "Mitochondrial remnant organelles of Giardia function in iron-sulphur protein maturation". Nature. 426 (6963): 172–6. doi:10.1038/nature01945. PMID 14614504.
- ↑ UpToDate (Lexi-Comp, Inc.) retrieved 28 August 2007
- ↑ Hetsko ML, McCaffery JM, Svärd SG, Meng TC, Que X, Gillin FD (1998). "Cellular and transcriptional changes during excystation of Giardia lamblia in vitro". Exp. Parasitol. 88 (3): 172–83. doi:10.1006/expr.1998.4246. PMID 9562420.
- ↑ Svärd SG, Meng TC, Hetsko ML, McCaffery JM, Gillin FD (1998). "Differentiation-associated surface antigen variation in the ancient eukaryote Giardia lamblia". Mol. Microbiol. 30 (5): 979–89. PMID 9988475.
- ↑ Ford, BJ The discovery of Giardia The Microscope 2005;53(4):148-153.
- ↑ Bennett, John (2015). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455748013.
External links
- GiardiaDB: The Giardia lamblia genome sequencing project
- Washington State Department of Health fact sheet on Giardia.
- Center for Disease Control fact sheet on Giardia
- Giardia article at MicrobeWiki
- Video of Giardia Life Cycle
- Giardia and the Sierra Nevada