Esophageal web: Difference between revisions
Ahmed Younes (talk | contribs) |
Ahmed Younes (talk | contribs) |
||
| Line 87: | Line 87: | ||
Esophageal webs must be differentiated from other causes of dysphagia such as achalasia and esophageal carcinoma. | Esophageal webs must be differentiated from other causes of dysphagia such as achalasia and esophageal carcinoma. | ||
<small> | |||
{| class="wikitable" | {| class="wikitable" | ||
! rowspan="3" |Disease | ! rowspan="3" align="center" style="background:#4479BA; color: #FFFFFF;" |Disease | ||
! colspan="8" |Signs and Symptoms | ! colspan="8" align="center" style="background:#4479BA; color: #FFFFFF;" |Signs and Symptoms | ||
! rowspan="3" |Barium esophagogram | ! rowspan="3" align="center" style="background:#4479BA; color: #FFFFFF;" |Barium esophagogram | ||
! rowspan="3" |Endoscopy | ! rowspan="3" align="center" style="background:#4479BA; color: #FFFFFF;" |Endoscopy | ||
! rowspan="3" |Other imaging findings | ! rowspan="3" align="center" style="background:#4479BA; color: #FFFFFF;" |Other imaging and laboratory findings | ||
! rowspan="3" |Gold Standard | ! rowspan="3" align="center" style="background:#4479BA; color: #FFFFFF;" |Gold Standard | ||
|- | |- | ||
| rowspan="2" |Onset | | rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" |Onset | ||
| colspan="3" |Dysphagia | | colspan="3" align="center" style="background:#4479BA; color: #FFFFFF;" |Dysphagia | ||
| rowspan="2" |Weight loss | | rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" |Weight loss | ||
| rowspan="2" |Heartburn | | rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" |Heartburn | ||
| rowspan="2" |Other findings | | rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" |Other findings | ||
| rowspan="2" |Mental status | | rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" |Mental status | ||
|- | |- | ||
|Solids | | align="center" style="background:#4479BA; color: #FFFFFF;" |Solids | ||
|Liquids | | align="center" style="background:#4479BA; color: #FFFFFF;" |Liquids | ||
|Type | | align="center" style="background:#4479BA; color: #FFFFFF;" |Type | ||
|- | |- | ||
|Plummer-Vinson syndrome | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |Plummer-Vinson syndrome | ||
|Gradual | | | ||
* Gradual | |||
| + | | + | ||
| - | | - | ||
| Line 114: | Line 116: | ||
| - | | - | ||
| | | | ||
* Glossitis | * [[Glossitis]] | ||
* Koilonychia | * [[Koilonychia]] | ||
|Normal | |Normal | ||
| | | | ||
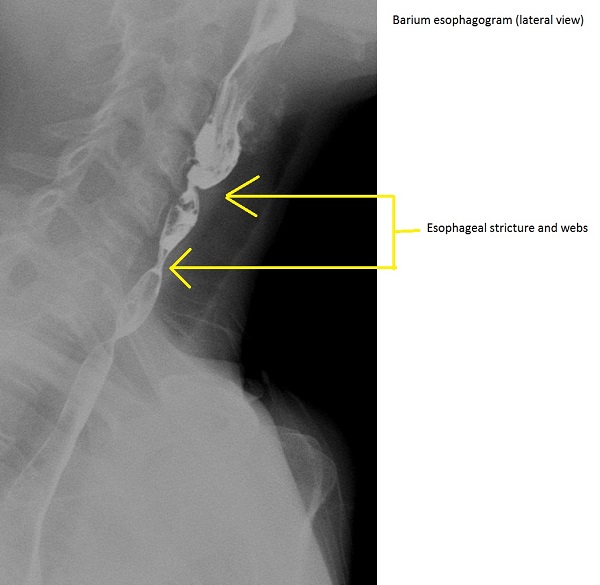
* Thin projections on the | * Thin projections on the anterior [[esophageal]] wall | ||
* Multiple upper | * Multiple upper [[Esophageal stricture|esophageal constrictions]] | ||
[[Image:Plummer-vinson-syndrome.jpg|center|200px|thumb|Barium esophagogram (Source: Case courtesy of Dr Hani Salam, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/14029">rID: 14029</a>)]] | |||
| | |||
* Direct visualization of [[esophageal webs]] | |||
* Superior to [[esophagogram]] | |||
<div style="width:350px">{{#ev:youtube|HFfsTgsB6Pg}}</div> | |||
| | | | ||
* | * Videofluoroscopy shows [[mucosal]] and [[submucosal]] foldings | ||
| | | | ||
Triad of | Triad of | ||
* Iron deficiency anemia | * [[Iron deficiency anemia]] | ||
* Esophageal webs | * [[Esophageal webs]] | ||
* Glossitis | * [[Glossitis]] | ||
|- | |- | ||
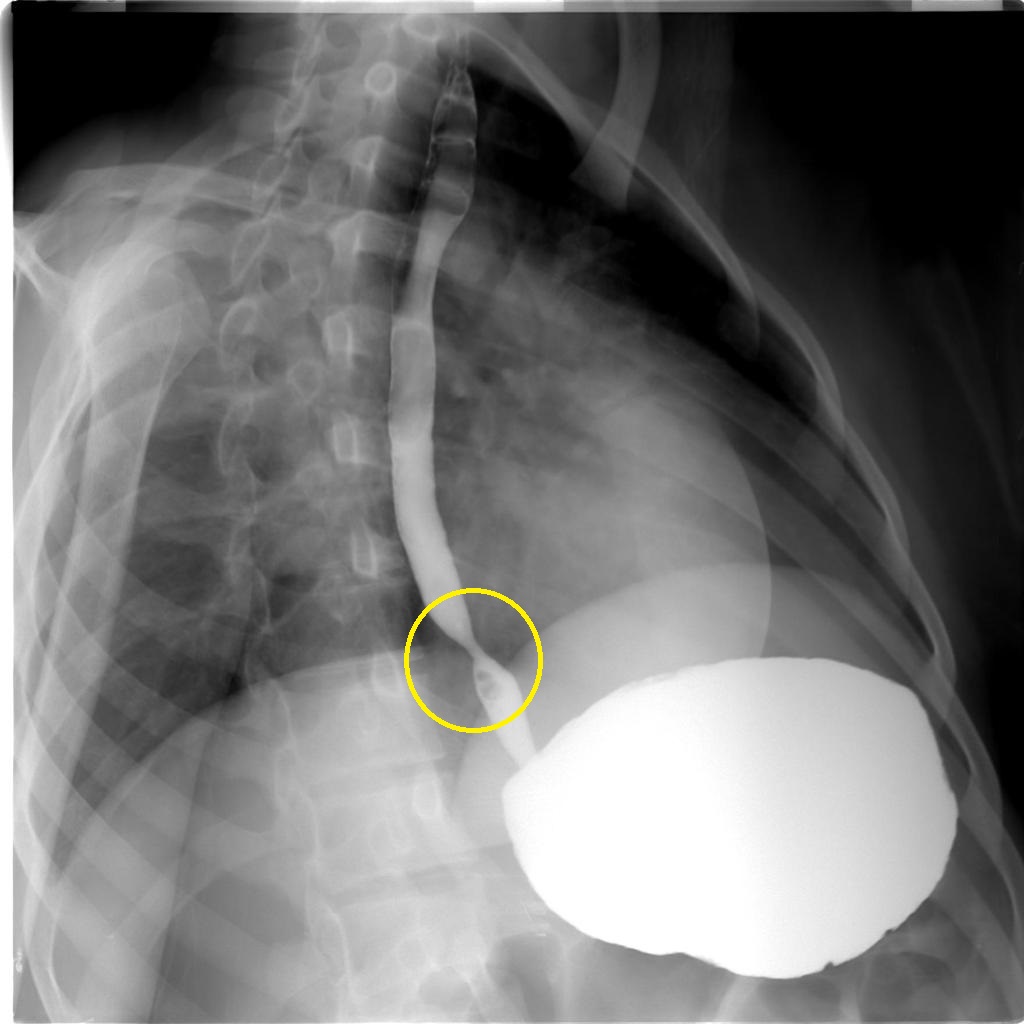
|Esophageal stricture | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Esophageal stricture]] | ||
| | | | ||
* Gradual | * Gradual | ||
| Line 152: | Line 157: | ||
*Sacculations | *Sacculations | ||
*Fixed transverse folds | *Fixed transverse folds | ||
* | *[[Esophageal]] intramural pseudodiverticula | ||
[[Image:Benign-oesophageal-stricture.jpg|center|200px|thumb|Case courtesy of Dr Ahmed Abd Rabou, Radiopaedia.org, rID: 23008]] | |||
| | |||
* [[Mucosal]] edema | |||
* Circumferential thickening in [[Gastroesophageal reflux disease|GERD]] | |||
* Pale [[mucosa]] with white [[exudate]] in lymphocytic esophagitis | |||
* [[Swelling]] and [[hemorrhagic]] [[congestion]] in [[caustic]]<nowiki/> ingestion | |||
<div style="width:350px">{{#ev:youtube|vax5E-jMnQ}}</div> | |||
| | | | ||
* | * [[Manometry]] may show dysmotility | ||
* [[CT scan]] for staging [[malignant]] [[strictures]] | |||
* [[ | |||
| | | | ||
* | * [[Esophagogram|Barium esophagogram]] | ||
|Barium esophagogram | |||
|- | |- | ||
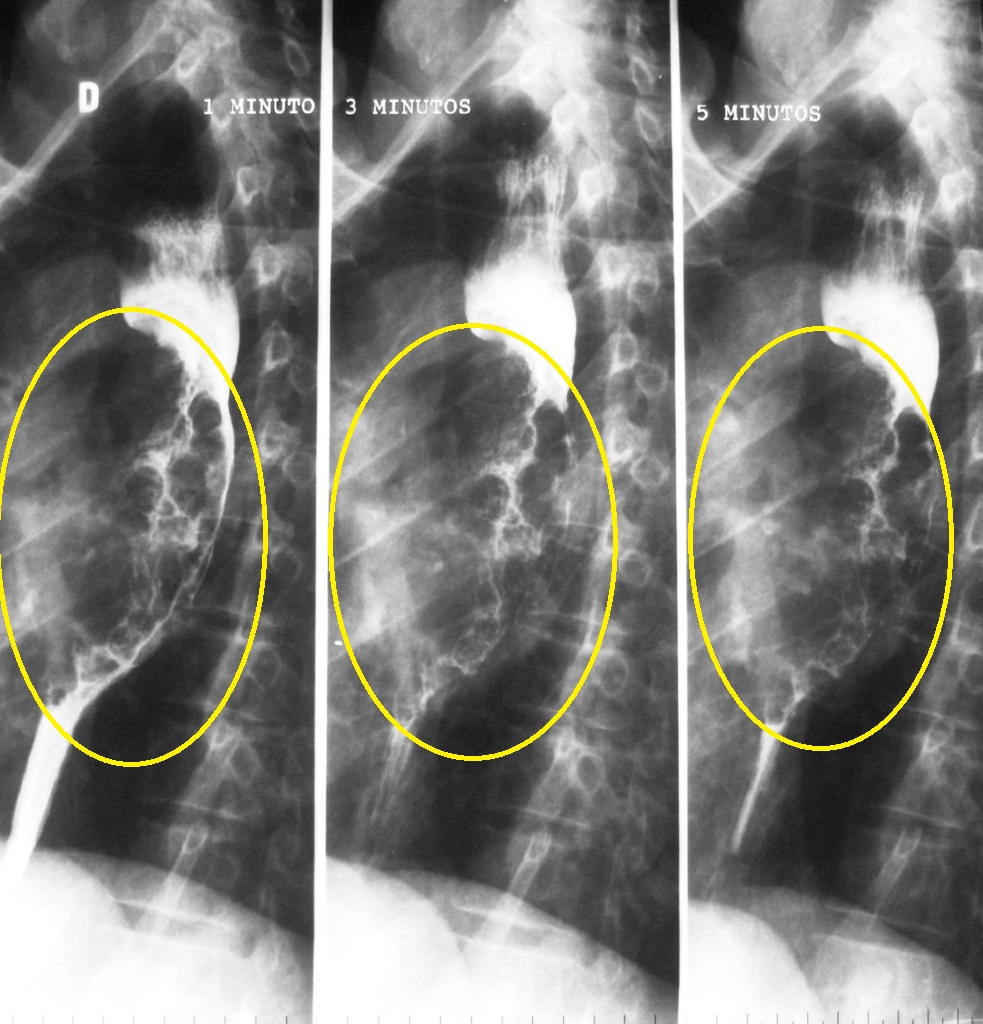
|Diffuse esophageal spasm | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Diffuse esophageal spasm]] | ||
| | | | ||
* Sudden | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| Line 180: | Line 186: | ||
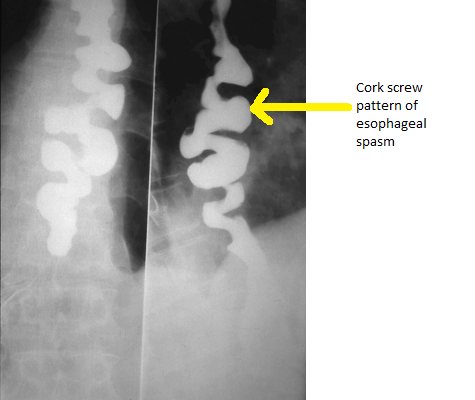
* Nonperistaltic and nonpropulsive contractions | * Nonperistaltic and nonpropulsive contractions | ||
* Corkscrew or rosary bead esophagus | * Corkscrew or rosary bead esophagus | ||
|Inconclusive | [[Image:DES radio.png|center|200px|thumb|Barium swallow appearance of DES<br>Source:By Nevit Dilmen [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)]] | ||
| | |||
* Inconclusive | |||
<div style="width:350px">{{#ev:youtube|2ipA34iMA3c}}</div> | |||
| | |||
*[[Manometry]] shows high-amplitude [[esophageal]] contractions | |||
*[[CT scan]] may show [[hypertrophy]] of esophageal muscles | |||
| | | | ||
*Manometry | * [[Manometry]] | ||
|- | |- | ||
|Achalasia | |style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Achalasia]] | ||
|Gradual | | | ||
* Gradual | |||
| + | | + | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| Line 194: | Line 205: | ||
| - | | - | ||
| | | | ||
* Regurgitation of undigested food | * [[Regurgitation]] of undigested food | ||
* Chest pain | * [[Chest pain]] | ||
|Normal | |Normal | ||
| | | | ||
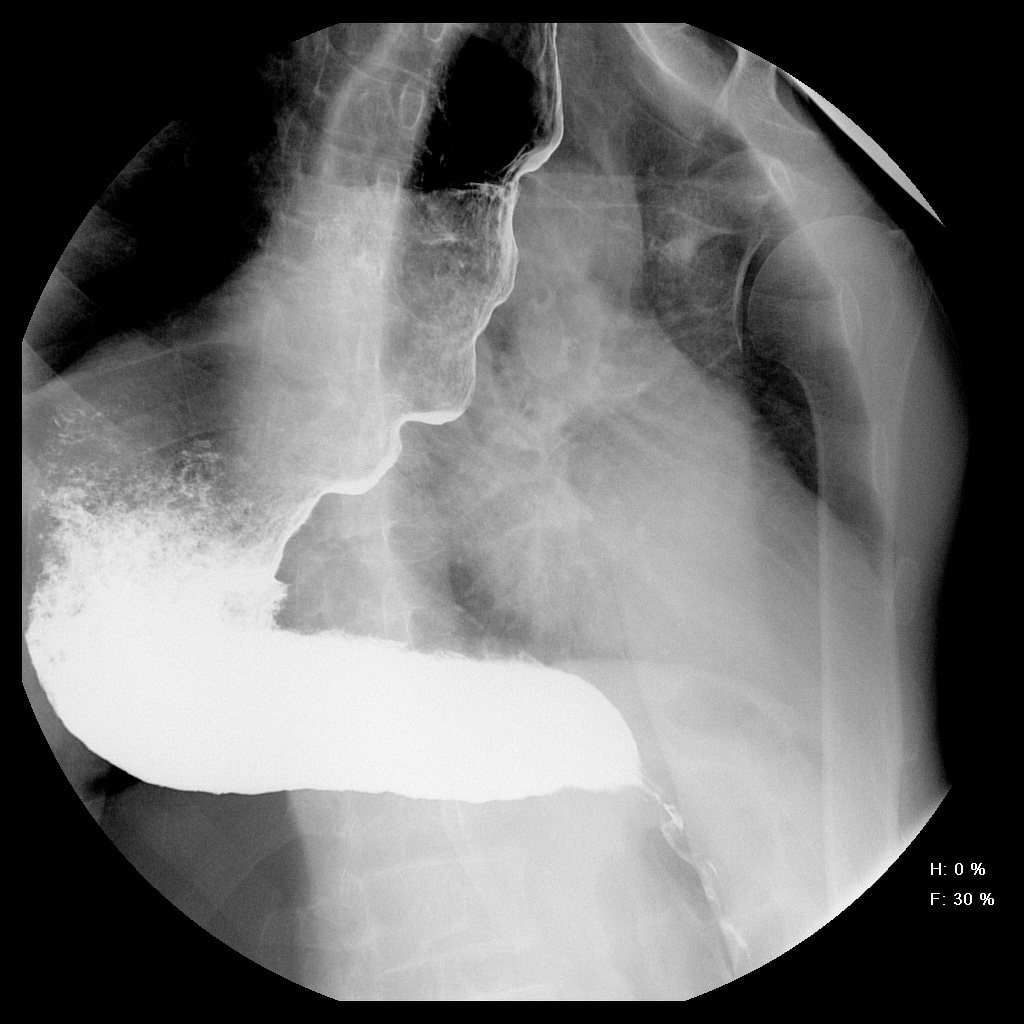
* "Bird's beak | * "Bird's beak" or "rat tail" appearance | ||
* Dilated esophageal body | * Dilated esophageal body | ||
* Air fluid level | * Air fluid level (absent [[peristalsis]]) | ||
* Absence of an intragastric air bubble | * Absence of an intragastric air bubble | ||
[[Image:Achalasia-2.jpg|center|200px|thumb|Case courtesy of Dr Mario Umana, Radiopaedia.org, rID: 38071]] | |||
| | | | ||
* Dilated esophagus | * Dilated [[esophagus]] | ||
* Residual food fragments | * Residual food fragments | ||
* Normal | * Normal [[mucosa]] | ||
<div style="width:350px">{{#ev:youtube|ydLcskQzEjM}}</div> | |||
| | | | ||
* Residual pressure of LES > 10 mmHg | * Residual pressure of [[Lower esophageal sphincter|LES]] > 10 mmHg | ||
* Incomplete relaxation of the [[Lower esophageal sphincter|LES]] | * Incomplete relaxation of the [[Lower esophageal sphincter|LES]] | ||
* Increased resting tone of [[Lower esophageal sphincter|LES]] | * Increased resting tone of [[Lower esophageal sphincter|LES]] | ||
* Aperistalsis | * Aperistalsis | ||
| | | | ||
* History of dysphagia | * History of [[dysphagia]] with positive [[endoscopy]] and [[manometry]] | ||
|- | |- | ||
|Systemic sclerosis | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Systemic sclerosis]] | ||
|Gradual | | | ||
* Gradual | |||
| + | | + | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| Line 226: | Line 236: | ||
| + | | + | ||
| | | | ||
* Muscle and joint pain | * [[Muscle pain|Muscle]] and [[Arthralgia|joint pain]] | ||
* Raynaud's phenomenon | * [[Raynaud's phenomenon]] | ||
* Skin changes | * [[Skin changes]] | ||
|Normal | |Normal | ||
| | | | ||
* Dysmotility | * Dysmotility | ||
* Patulous esophagus | * Patulous [[esophagus]] | ||
| | | | ||
* Mucosal damage | * [[Mucosal]] damage | ||
* Peptic stricture (advanced cases) | * [[Peptic]] stricture (advanced cases) | ||
|Positive serology for | |Positive serology for | ||
* Antinuclear antibodies | * [[Antinuclear antibodies]] | ||
* Rheumatoid factor | * [[Rheumatoid factor]] | ||
* Creatine kinase | * [[Creatine kinase]] | ||
* ESR | * [[ESR]] | ||
|Skin | | | ||
* [[Skin biopsy]] | |||
|- | |- | ||
|Zenker's diverticulum | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Zenker's diverticulum]] | ||
|Gradual | | | ||
* Gradual | |||
| + | | + | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| | | | ||
| +/- | | +/- | ||
| - | | - | ||
| | | | ||
* Food [[regurgitation]] | * Food [[regurgitation]] | ||
| Line 264: | Line 274: | ||
* [[Halitosis]] | * [[Halitosis]] | ||
* [[Coughing]] | * [[Coughing|Cough]] | ||
* [[Hoarseness]] | * [[Hoarseness]] | ||
|Normal | |||
| | |||
* Thin projections on [[esophageal]] wall over [[Killian's dehiscence|Killian's triangle]] | |||
[[Image:Zenker-4.jpg|center|200px|thumb|Zenker's diverticulum-Frontal view <br> Source:Radiopaedia<ref name="urlZenker diverticulum, Case courtesy of Dr Bruno Di Muzio, | Radiology Case | Radiopaedia.org">{{cite web |url=https://radiopaedia.org/cases/zenker-diverticulum |title=Zenker diverticulum | Radiology Case | Radiopaedia.org |format= |work= |accessdate=}}</ref>]] | |||
| | |||
* Outpouching of posterior [[pharyngeal]] wall | |||
* [[ | * Exclude the presence of [[Squamous cell carcinoma|SCC]] | ||
| | <div style="width:350px">{{#ev:youtube|FdEruFsNdVA}}</div> | ||
| | | | ||
* [[CT]] & [[MRI]] shows out-pouching over the posterior esophagus in the Killian's triangle | |||
| | | | ||
* Barium [[Esophagogram|esophagography]] | |||
|- | |- | ||
|Esophageal carcinoma | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Esophageal carcinoma]] | ||
| | | | ||
* Gradual | |||
|<nowiki>+</nowiki> | |||
|<nowiki>+</nowiki> | |||
|Progressive | |Progressive | ||
| + | | + | ||
|<nowiki>+/-</nowiki> | |||
| | | | ||
* [[Lymphadenopathy]] | |||
* [[Cachexia]] | |||
|Normal | |||
| | | | ||
* Irregular [[Strictures|stricture]] | |||
* Pre-stricture [[dilatation]] | |||
[[Image:Oesophageal-squamous-cell-carcinoma-2.jpg|center|200px|thumb|Case courtesy of Dr Bruno Di Muzio, Radiopaedia.org, rID: 4232f]] | |||
| | | | ||
* [[Esophageal]] obstruction | |||
* Staging of disease | |||
<div style="width:350px">{{#ev:youtube|5ucSlgqGAno}}</div> | |||
| | | | ||
* [[CT]] and [[PET scan]] is an optional test for staging of the disease | |||
| | | | ||
* [[Biopsy]] | |||
|- | |- | ||
|Stroke | |style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Stroke]] | ||
([[Cerebral hemorrhage]]) | |||
| | | | ||
* Sudden | |||
|<nowiki>+</nowiki> | |||
|<nowiki>+</nowiki> | |||
|Progressive | |||
|<nowiki>+</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| | | | ||
* [[Dysarthria]] | |||
* Limb [[weakness]] | |||
* [[Fatigue]] | |||
|Impaired | |Impaired | ||
| | | | ||
* Pooling of [[Contrast medium|contrast]] in the [[pharynx]] | |||
* [[Aspiration]] of [[barium]] [[Contrast medium|contrast]] into the [[airway]] | |||
| | | | ||
* Reduced opening of [[upper esophageal sphincter]] | |||
* Reduced [[larynx]] elevation | |||
| | | | ||
* [[CT]] without [[contrast]] shows acute [[hemorrhage]] as a hyperattenuating [[clot]] | |||
| | | | ||
* [[CT]] without [[Contrast medium|contrast]] | |||
|- | |- | ||
|Motor disorders | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |Motor disorders | ||
(Myasthenia gravis) | ([[Myasthenia gravis]]) | ||
| | | | ||
* Gradual | |||
| + | | + | ||
| + | | + | ||
| Line 310: | Line 354: | ||
| | | | ||
| | | | ||
* [[Ptosis]] | |||
* [[Diplopia]] | |||
* [[Fatigue]] | |||
|Normal | |Normal | ||
| | | | ||
* Stasis in [[pharynx]] and pooling in pharyngeal recesses | |||
| | |||
* [[Velopharyngeal insufficiency]] | |||
* Delayed [[swallowing]] function | |||
| | | | ||
* CT may show anterior [[mediastinal]] mass ([[thymoma]]) | |||
* Positive tensilon test | |||
| | | | ||
* Anti–acetylcholine receptor antibody test | |||
|- | |- | ||
|GERD | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[GERD]] | ||
| | | | ||
* Gradual | |||
* Sudden onset | |||
| + | | + | ||
| - | | - | ||
|Progressive | |Progressive | ||
| +/- | | +/- | ||
| + | |||
| | | | ||
* [[Cough]] | |||
* [[Hoarseness]] | |||
|Normal | |||
| | | | ||
* Free acid reflux | |||
* [[Esophagitis]] with scarring | |||
* [[Strictures]] | |||
* [[Barrett's oesophagus]] | |||
| | | | ||
* [[Erythema]], erosions and [[ulceration]] | |||
* [[Barrett's esophagus]] | |||
| | | | ||
* Esophageal [[manometry]] may show decreased tone of [[Lower esophageal sphincter|LES]] | |||
| | | | ||
* 24 hour [[esophageal]] pH monitoring | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Esophageal web]] | |||
| | | | ||
* Gradual | |||
| + | | + | ||
| +/- | | +/- | ||
| Line 339: | Line 405: | ||
| - | | - | ||
| +/- | | +/- | ||
|Findings of the underlying cause such as iron deficiency anemia or bullous pemphigoid | | | ||
* Findings of the underlying cause such as [[iron deficiency anemia]] or [[bullous pemphigoid]] | |||
|Normal | |Normal | ||
| | | | ||
* | * Symmetrical narrowing of the [[esophagus]] | ||
| | | | ||
* Smooth membrane not encircling the whole [[Lumen (anatomy)|lumen]] | |||
| | |||
* Videofluoroscopy shows [[mucosal]] and [[submucosal]] foldings | |||
| | | | ||
* Barium esophagogram | * Barium [[esophagogram]] | ||
|} | |} | ||
<small> | |||
==Epidemiology== | ==Epidemiology== | ||
Revision as of 21:27, 20 November 2017
|
Esophageal web Main page |
|
Diagnosis |
|---|
|
Treatment |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Synonyms and keywords: Oesophageal web
Overview
| {| class="infobox bordered" style="width: 15em; text-align: left; font-size: 90%; background:AliceBlue" | |
|
Esophageal web Main page | |
|
Diagnosis | |
|---|---|
|
Treatment | |
|-
|- style="line-height: 1;"
|-
|-
|- ! DiseasesDB | 31503 |-
|-
|-
|-
|} Esophageal webs are mucosal folds that partially obstructs the esophageal lumen. The exact pathogenesis of esophageal webs is not known but it is thought to be due to either esophageal inflammation, congenital anomaly, or iron deficiency. They can be classified into type A, B, and C according to their site and extent, type B being the most common. The most common causes are Plummer-Vinson syndrome, celiac sprue and Zenker’s diverticulum. Esophageal webs most commonly present with dysphagia that has a slow onset and is rarely complicated with weight loss. Esophageal webs must be differentiated from other causes of dysphagia such esophageal strictures and achalasia. In barium esophagram, esophageal webs appear as a uniform narrowing of the esophagus and on endoscopy, esophageal webs appear as a smooth narrowing of the esophagus that is not present in the whole circumference of the lumen. Esophageal dilation is the cornerstone of treatment and it is effective in relieving the symptoms but with high recurrence rate.
Historical perspective
- In 1944, esophageal webs were first described by Templeton and it was thought to be a congenital disease because most of the patients were children.[1]
- In 1953, a series of case reports of patients having dysphagia and radiological signs denoting esophageal narrowing made the diagnosis of esophageal rings not confined to the pediatric population.
- In 1968, histological examination of specimens from the esophageal rings proved that none of them had muscle involvement.[2]
Classification
Esophageal webs can be classified according to their site and extent in three categories[3] [4][5]
Type A
- Type A esophageal rings describe webs that involve the muscle layer of the esophageal wall and lies in close proximity to the squamocolumnar junction.
- It is less common than type B esophageal webs.
Type B
- Type B esophageal rings describe the webs that involve only the mucosa and submucosa of the esophagus.
- It is often named “Schatzki ring”.
- It is located exactly at the squamocolumnar junction.
Type C
- Type C esophageal rings refer to wall invaginations due to pressure from the diaphragm.
- It is rare with no clinical significance.
Pathophysiology
Pathogenesis
There are multiple theories explaining the origin of esophageal webs
Inflammation
- Esophageal webs are thought to be due to the chronic damage to the esophageal mucosa.
- This is supported by the presence of inflammatory cells in the wall of the web.[1]
- In allergic esophagitis, eosinophils were found while in cases of chronic inflammation as GERD, lymphocytes prevailed.
Congenital theory
- Esophageal webs are thought to be due to failure of the esophagus to recanalize.
- Specimens showed that the esophageal webs contained respiratory epithelium supporting this theory.[6]
- The webs mostly remain asymptomatic for long times and that is why it is not correlated with being congenital.
Iron deficiency
- The esophageal webs of Plummer-Vinson syndrome have been associated with iron deficiency anemia in many studies.
- The exact mechanism by which iron deficiency causes esophageal webs is not known, but it was hypothesized that iron deficiency starts a sequence of events in the esophageal epithelium that ends in its damage and formation of a web.[7]
- Moreover, treatment of iron deficiency in Plummer-Vinson syndrome patients leads to resolution of dysphagia even before the laboratory results become normal.
Gross picture
- Esophageal webs appear as an eccentric narrowing of the esophageal lumen (while rings cause circumferential narrowing).
Microscopic picture
- Esophageal webs are covered normally by mucosa and submucosa.
- It is characterized by the presence of basal cell hyperplasia.
- The tissue is often heavily infiltrated with chronic inflammatory cells.
- Eosinophilic esophagitis is characterized by the presence of eosinophils infiltration.
Causes
More common causes
- Iron deficiency anemia
- Plummer-Vinson syndrome
- Celiac sprue
- Zenker’s diverticulum
Less common causes
Differentiating esophageal webs from other diseases
Esophageal webs must be differentiated from other causes of dysphagia such as achalasia and esophageal carcinoma.
| Disease | Signs and Symptoms | Barium esophagogram | Endoscopy | Other imaging and laboratory findings | Gold Standard | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Onset | Dysphagia | Weight loss | Heartburn | Other findings | Mental status | |||||||
| Solids | Liquids | Type | ||||||||||
| Plummer-Vinson syndrome |
|
+ | - | Non progressive | +/- | - | Normal |
 |
{{#ev:youtube|HFfsTgsB6Pg}}
|
|
Triad of | |
| Esophageal stricture |
|
+ | - | Progressive | +/- | +/- | Normal |
 |
{{#ev:youtube|vax5E-jMnQ}}
|
|
||
| Diffuse esophageal spasm |
|
+ | + | Non progressive | + | + | Normal |
 Source:By Nevit Dilmen [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) |
{{#ev:youtube|2ipA34iMA3c}}
|
|
||
| Achalasia |
|
+ | + | Non progressive | +/- | - |
|
Normal |
 |
{{#ev:youtube|ydLcskQzEjM}}
|
||
| Systemic sclerosis |
|
+ | + | Progressive | +/- | + |
|
Normal |
|
|
Positive serology for | |
| Zenker's diverticulum |
|
+ | - | +/- | - |
|
Normal |
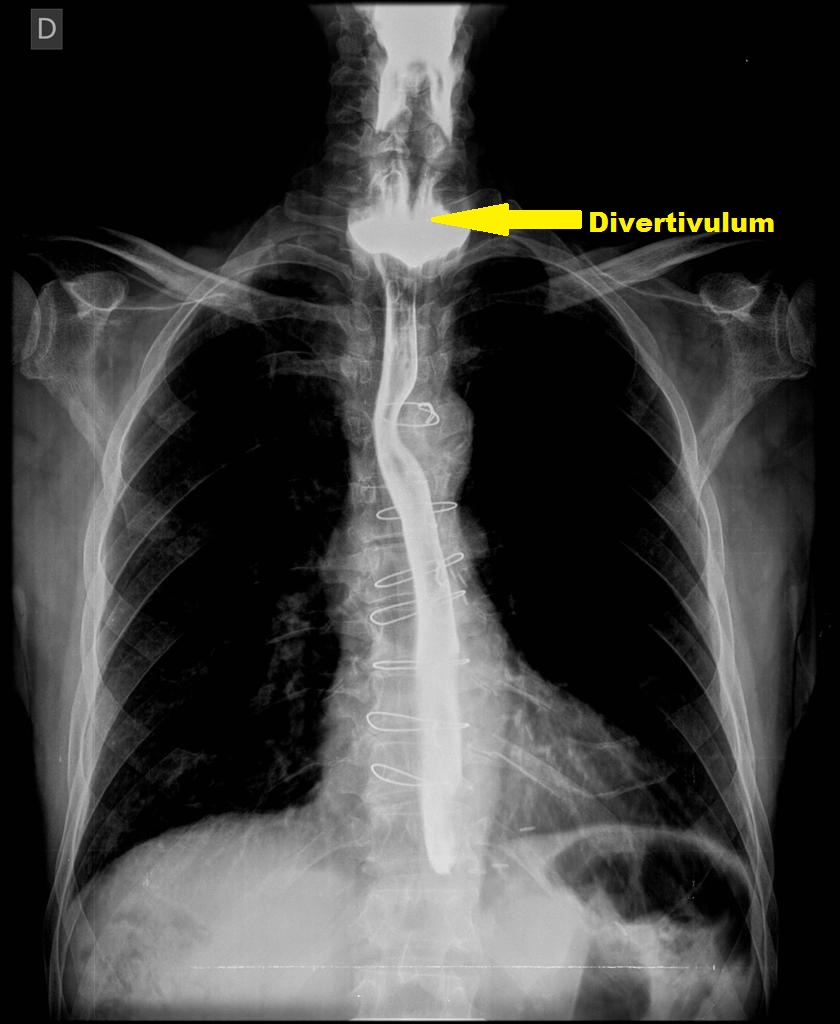 Source:Radiopaedia[8] |
{{#ev:youtube|FdEruFsNdVA}}
|
| ||
| Esophageal carcinoma |
|
+ | + | Progressive | + | +/- | Normal |
 |
{{#ev:youtube|5ucSlgqGAno}}
|
|||
| Stroke |
|
+ | + | Progressive | + | +/- |
|
Impaired |
|
|
||
| Motor disorders |
|
+ | + | Progressive | +/- | Normal |
|
|
|
| ||
| GERD |
|
+ | - | Progressive | +/- | + | Normal |
|
|
| ||
| Esophageal web |
|
+ | +/- | Progressive | - | +/- |
|
Normal |
|
|
|
|
Epidemiology
Prevalence
- Webs are diagnosed in 5-15% of patients doing barium esophagogram for diagnosing the cause of dysphagia.
- Congenital esophageal webs are estimated to be 1 in 25,000 to 1 in 50,000 live births.
Race
- Esophageal webs affects the whites more than other population
Sex
- Esophageal webs tend to be more common in females.
- This may be due to the increased prevalence of iron deficiency anemia.
Age
- Esophageal has no predilection for an age group, however, it is usually not symptomatic until after the age of 40.
Screening
According to USPSTF, there are no screening measures recommended for esophageal webs.
Natural history, complications and prognosis
Natural history
- The disease can start at any age but symptoms usually start in the fifth decade of life.
- The dysphagia is usually to solids at the beginning then it progresses to both solids and liquids.
- If left untreated, the webs may progress causing esophageal strictures and esophageal carcinoma.
Complications
- Progression to esophageal carcinoma.
- Choking spells
- Esophagitis from chronic injury of the mucosa
- Progression to esophageal stricture
Prognosis
- The prognosis of esophageal webs is generally good especially with treatment of the underlying cause.
- One of out of ten patients with Plummer-Vinson syndrome will develop esophageal carcinoma.
History and symptoms
History
- Patients are usually older than 40 years because it can be asymptomatic for a long time.
- The patient may give a history of the cause such as iron deficiency anemia, GERD, or autoimmune disease.
- There may be a history of excessive food chewing to facilitate swallowing.
Symptoms
- Most of the esophageal webs are asymptomatic.
- The major symptom of esophageal webs is dysphagia.
- Dysphagia is usually more for solid food.
- Esophageal webs do not usually result in malnutrition nor to weight loss.
Physical examination
Esophageal webs do not have significant physical exam findings, however, it might show the signs of the cause such as
- Koilonychia and glossitis in the cases of Plummer-Vinson syndrome.
- It might also show the findings in in the cases of skin disorders such as epidermolysis bullosa, bullous pemphigoid, and pemphigus vulgaris.
Lab findings
- A Laboratory workup is not necessary for the diagnosis of esophageal webs because the diagnosis is dependent on the symptoms and radiological tests.
- CBC might show microcytic hypochromic anemia in cases of Plummer-Vinson syndrome as it is the primary cause of the esophageal web.
- Antibody panel might be done to screen for the primary cause.
Radiological tests
Barium esophagogram
- It is more sensitive in detecting esophageal webs than endoscopy.
- Webs appear as a uniform narrowing of the esophageal lumen.
Other diagnostic tests
Endoscopy
- Endoscopy is less sensitive in detecting webs than barium esophagram.
- Esophageal webs appear as a smooth membrane that is not encircling the whole lumen.
- It allows obtaining a biopsy from the lesion in addition to excluding other causes of dysphagia.
- Esophageal webs can go unnoticed during the esophagram as it is only a mucous membrane fold with no muscle support.
Treatment
Medical treatment
- Patients should be educated to change their diet and food habits, especially in the cases when esophageal webs are secondary to GERD.
- H2 blockers or proton pump inhibitors can be used for managing the symptoms of GERD and the prevention of progression to webs.
- Proper management of acid reflux after esophageal dilation is associated with decreased recurrence of symptoms.
Surgical treatment
- Esophageal dilation is the cornerstone of treating esophageal webs especially in cases refractory to medical treatment.
- In cases of eosinophilic esophagitis, dilation should be gradual as sudden forced dilation is associated with muscle tears.
- In cases of non-eosinophilic esophagitis, dilation using a single dilator is more effective than graded dilation.
- Esophageal dilation is associated with improved symptoms of dysphagia.
- Esophageal dilation is associated with symptom recurrence in about 89% at five years and often requires redoing of the procedure.
References
- ↑ 1.0 1.1 Okamura H, Tsutsumi S, Inaki S, Mori T (1988). "Esophageal web in Plummer-Vinson syndrome". Laryngoscope. 98 (9): 994–8. doi:10.1288/00005537-198809000-00014. PMID 3412097.
- ↑ HARDY JD, CONN JH (1962). "Diseases of the esophagus: an analysis of 308 consecutive cases". Ann. Surg. 155: 971–90. PMC 1466157. PMID 13904659.
- ↑ Smith MS (2010). "Diagnosis and management of esophageal rings and webs". Gastroenterol Hepatol (N Y). 6 (11): 701–4. PMC 3033540. PMID 21437018.
- ↑ Mann NS, Leung JW (2005). "Pathogenesis of esophageal rings in eosinophilic esophagitis". Med. Hypotheses. 64 (3): 520–3. doi:10.1016/j.mehy.2004.08.021. PMID 15617859.
- ↑ Pleet JL, Taboada S, Rishi A, Milman PJ, Trindade AJ (2017). "Rings in the esophagus are not always eosinophilic esophagitis: Case series of ring forming lymphocytic esophagitis and review of the literature". Endosc Int Open. 5 (6): E484–E488. doi:10.1055/s-0043-106579. PMC 5451283. PMID 28573181.
- ↑ Sinha SK, Nain CK, Udawat HP, Prasad KK, Das R, Nagi B, Singh K (2008). "Cervical esophageal web and celiac disease". J. Gastroenterol. Hepatol. 23 (7 Pt 1): 1149–52. doi:10.1111/j.1440-1746.2008.05452.x. PMID 18554241.
- ↑ DeVault KR (1996). "Lower esophageal (Schatzki's) ring: pathogenesis, diagnosis and therapy". Dig Dis. 14 (5): 323–9. PMID 8902418.
- ↑ "Zenker diverticulum | Radiology Case | Radiopaedia.org".