Cryptosporidium parvum: Difference between revisions
No edit summary |
No edit summary |
||
| Line 20: | Line 20: | ||
}} | }} | ||
'''''Cryptosporidium parvum''''' is one of several [[protozoa]]l species that cause [[cryptosporidiosis]], a [[parasitic disease]] of the [[mammal]]ian [[intestine|intestinal tract]]. | |||
''''' | Primary symptoms of ''C. parvum'' infection are acute, watery, and non-bloody [[diarrhea]]. ''C. parvum'' infection is of particular concern in [[immunocompromised]] patients, where diarrhea can reach 10–15L per day. Other symptoms may include [[anorexia (symptom)|anorexia]], [[nausea]]/[[vomiting]] and [[abdomen|abdominal]] pain. Extra-intestinal sites include the lung, liver and gall bladder where it causes respiratory cryptosporidosis, hepatitis and cholecystitis.<ref>”Cryptosporidiosis.” Laboratory Identification of Parasites of Public Health Concern. CDC. 5 Sept 2007. <http://www.dpd.cdc.gov/dpdx/HTML/Cryptosporidiosis.htm></ref>{{Failed verification|date=January 2012}} | ||
Cryptosporidium parvum is | Infection is caused by ingestion of [[sporulate]]d [[oocyst]]s transmitted by the faecal-oral route. In healthy human hosts, the median infective dose is 132 oocysts.<ref>{{cite journal |author=DuPont HL, Chappell CL, Sterling CR, Okhuysen PC, Rose JB, Jakubowski W |title=The infectivity of Cryptosporidium parvum in healthy volunteers |journal=N. Engl. J. Med. |volume=332 |issue=13 |pages=855–9 |date=March 1995 |pmid=7870140 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=7870140&promo=ONFLNS19 |doi=10.1056/NEJM199503303321304}}</ref> The general [[Cryptosporidium#Life cycle|''C. parvum'' life cycle]] is shared by other members of the genus. Invasion of the [[wikt:apical|apical]] tip of [[ileal]] [[enterocyte]]s by [[sporozoite]]s and [[merozoite]]s causes pathology seen in the disease. | ||
In [[ | Infection is generally self-limiting in immunocompetent people. In immunocompromised patients, such as those with [[AIDS]] or those undergoing immunosuppressive therapy, infection may not be self-limiting, leading to dehydration and, in severe cases, death. | ||
==Detection== | |||
''Cryptosporidium parvum'' oocysts are very difficult to detect and therefore diagnose. The oocysts in fecal samples would indicate if the parasite is present in the body but they have a very small size and so detection is made very difficult. Doing a fecal ELISA method to detect the presence of the parasite would eliminate the difficulty due to the small size and many other methods are unable to distinguish between past and present infections; something serological ELISA would not allow to distinguish.<ref name="nejm.org">DuPont et al "The Infectivivty of Cryptosporidium parvum in healthy Volunteers" http://www.nejm.org/doi/pdf/10.1056/NEJM199503303321304</ref> | |||
''C. parvum'' is considered to be the most important waterborne pathogen in developed countries. The protozoa also caused the largest waterborne-disease outbreak ever documented in the United States, making 403,000 people ill in Milwaukee, Wisconsin in 1993.<ref>”Surveillance for Waterborne-Disease Outbreaks -- United States, 1993-1994” CDC. 1996. <http://www.cdc.gov/mmwr/preview/mmwrhtml/00040818.htm></ref> It is resistant to all practical levels of Water chlorination, surviving for 24hrs at 1000 mg/L free chlorine. It is an obligate intracellular pathogen.<ref>{{Cite journal | doi = 10.1016/j.ijpara.2003.10.001 | last1 = Deng | first1 = M. | last2 = Lancto | first2 = C. A. | last3 = Abrahamsen | first3 = M. S. | title = Cryptosporidium parvum regulation of human epithelial cell gene expression | journal = International Journal for Parasitology | volume = 34 | issue = 1 | pages = 73–82 | year = 2004 | pmid = 14711592}}</ref> | |||
==Prevention== | |||
The most effective way to prevent the spread of ''Cryptosporidium parvum'' is to avoid the contact of feces that are contaminated. Avoiding this contact, especially with young children is important, as they are more likely to come into oral contact and have the parasite transferred into the body. These ideas of hygiene are the most effective way to combat this difficult to prevent parasite.<ref name="aem.asm.org">Robertson et al "Survival of Cryposporidium parvum oocysts under various environmental pressures" http://aem.asm.org/content/58/11/3494.full.pdf+html</ref> | |||
==Oocyst Stage== | |||
The ''Cryptosporidium parvum'' oocysts are incredibly durable and this can cause extended problems when attempting to control the spread of the parasite. The oocyst stage can tolerate a vast number of environmental pressures that allows it to be more likely to survive. The oocyst can tolerate temperatures as low as -22C and for long periods of time which means fecal contamination is possible even after going through those environmental extremes. The oocysts can also tolerate shifts in pH that are found in some water treatment process and careful attention to detail must be done to prevent the possibility of infection. The oocysts that are in fecal material are immediately infective and have the potential to find a new host if contamination occurs.<ref name="nejm.org"/><ref name="aem.asm.org"/> | |||
==Genome== | |||
The genome of ''C. parvum'' (sequenced in 2004<ref name="Abrahamsen_2004">{{cite journal | author = Abrahamsen MS, Templeton TJ | title = Complete genome sequence of the apicomplexan, ''Cryptosporidium parvum'' | journal = Science | volume = 304 | issue = 5669 | pages = 441–5 | year = 2004 | pmid = 15044751 | doi = 10.1126/science.1094786 | accessdate = 2008-05-25| url=http://www.sciencemag.org/cgi/content/abstract/304/5669/441|display-authors=etal}}</ref>) have a relatively small size and simple organization of 9.1 Mb, which is composed of eight chromosomes ranging from 1.04 to 1.5 Mb. The genome is very compact, and is one of the few organisms without [[transposable element]]s. Unlike other [[apicomplexa]]ns, ''C. parvum'' has no genes in its [[plastid]]s or [[Mitochondrion|mitochondria]].<ref name="Abrahamsen_2004"/> | |||
==Treatment== | |||
==References== | Supportive therapy such as IV fluids is the primary for ''C. parvum'' infection. [[Paromomycin]] and [[Nitazoxanide]] may alleviate some of the diarrhoeal symptoms, however the latter is contraindicated for AIDS patients. Continuing [[antiretroviral drug]]s to boost the immune system may also control infection. Research into other potential drugs and therapeutics targets, as well as vaccine candidates, is ongoing. | ||
'''''Spiramycin''''' for immunosuppressed patients. | |||
==Important ''C. parvum'' proteins and drug targets== | |||
===Lipid metabolism=== | |||
''C. parvum'' is incapable of de novo lipid synthesis, making its lipid trafficking machinery an important potential therapeutic target. ''C. parvum'' possesses multiple oxysterol-binding proteins (OSBPs), and oxysterol related proteins (OSRPs). Only OSBPs are capable of lipid binding, while both contain [[Pleckstrin homology domain]]s, which function in cell signalling pathways. | |||
===Surface glycoproteins=== | |||
''C. parvum'' possesses numerous surface [[glycoprotein]]s thought to play a role in pathogenesis. An immunodominant >900kDa protein, known as GP900, localizes to the apical end of sporozoites and in [[microneme]]s of merozoites. Its high molecular mass is most likely due to heavy post-translational glycosylation. Indeed, the structure of GP900 is similar to that of a family of glycoproteins known as [[mucin]]s. GP900 is thought to mediate attachment and invasion to host cells. GP900 may also play a role in ''C. parvum’s'' resistance to [[proteolysis]] by the numerous [[proteases]] found in the mammalian gut. | |||
In vitro, hyperimmune sera as well as antibodies directed at specific [[epitope]]s on the GP900 protein inhibit the invasion of ''C. parvum'' sporozoites into MDCK cell monolayers. Additionally, competitive inhibition using native GP900 or purified GP900 fragments reduces cell invasion.<ref>{{cite journal |author=Barnes DA, Bonnin A, Huang JX |title=A novel multi-domain mucin-like glycoprotein of Cryptosporidium parvum mediates invasion |journal=Mol. Biochem. Parasitol. |volume=96 |issue=1–2 |pages=93–110 |date=October 1998 |pmid=9851610 |url=http://linkinghub.elsevier.com/retrieve/pii/S0166-6851(98)00119-4 |doi=10.1016/S0166-6851(98)00119-4|display-authors=etal}}</ref> | |||
Further experiments have confirmed the importance of the mucin-like glycosylations. Lectins directed at GP900 carbohydrate moieties (alpha-N-galactosamine) were able to block adhesion and prevent ''C. parvum'' invasion.<ref>{{cite journal |author=Cevallos AM, Bhat N, Verdon R |title=Mediation of Cryptosporidium parvum Infection In Vitro by Mucin-Like Glycoproteins Defined by a Neutralizing Monoclonal Antibody |journal=Infect. Immun. |volume=68 |issue=9 |pages=5167–75 |date=September 2000 |pmid=10948140 |pmc=101770 |url=http://iai.asm.org/cgi/pmidlookup?view=long&pmid=10948140 |doi=10.1128/IAI.68.9.5167-5175.2000|display-authors=etal}}</ref> | |||
''C. parvum'' glycoproteins have the characteristics of attractive vaccine candidates. Many are immunodominant, and antibodies against select domains block invasion of host cells. | |||
== References == | |||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Apicomplexa]] | [[Category:Apicomplexa]] | ||
Revision as of 18:26, 9 October 2015
|
Cryptosporidiosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cryptosporidium parvum On the Web |
|
American Roentgen Ray Society Images of Cryptosporidium parvum |
|
Risk calculators and risk factors for Cryptosporidium parvum |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];
| Cryptosporidium parvum | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
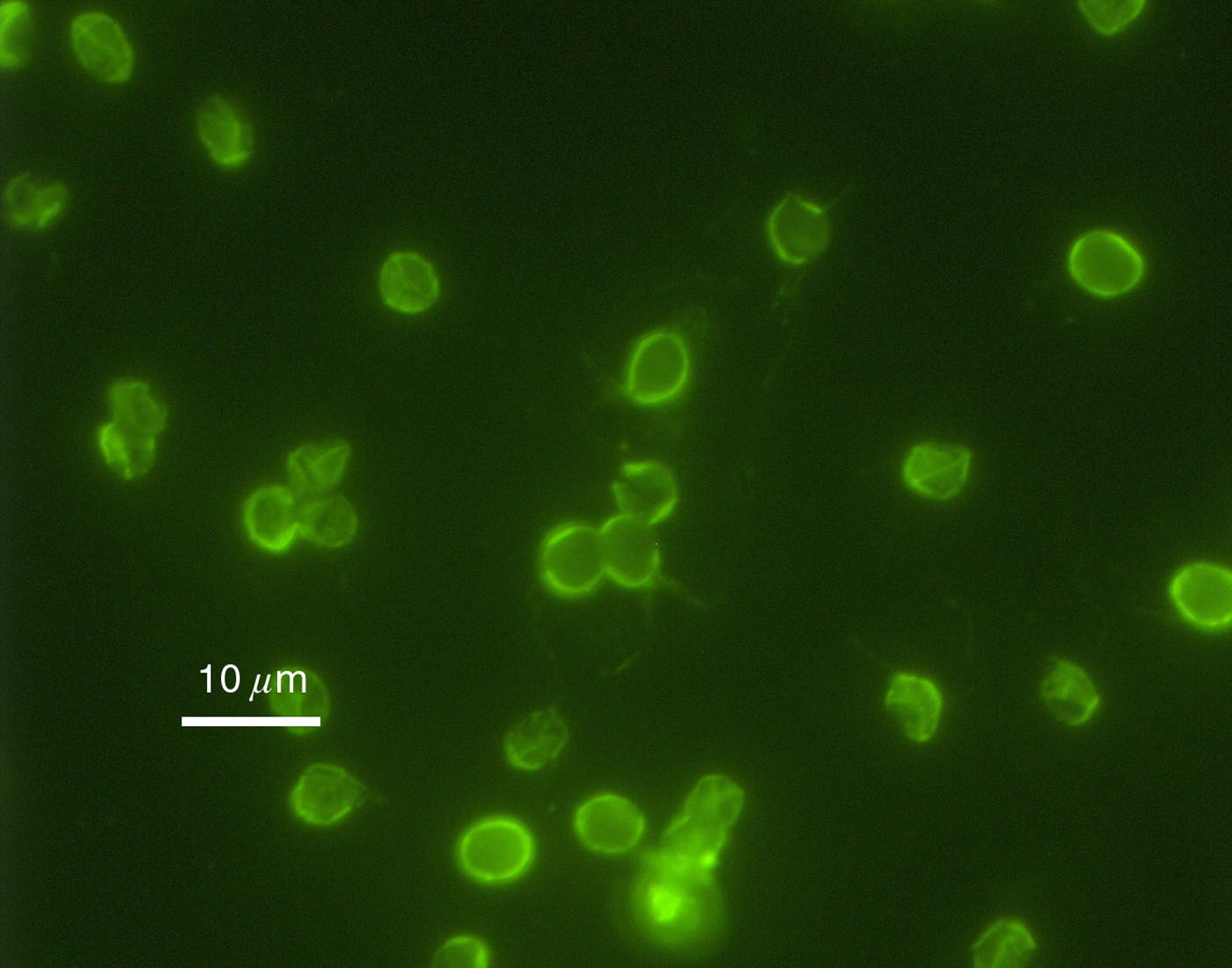 Immunofluorescence image of C. parvum oocysts.
| ||||||||||||||||
| Scientific classification | ||||||||||||||||
| ||||||||||||||||
| Binomial name | ||||||||||||||||
| Cryptosporidium parvum |
Cryptosporidium parvum is one of several protozoal species that cause cryptosporidiosis, a parasitic disease of the mammalian intestinal tract.
Primary symptoms of C. parvum infection are acute, watery, and non-bloody diarrhea. C. parvum infection is of particular concern in immunocompromised patients, where diarrhea can reach 10–15L per day. Other symptoms may include anorexia, nausea/vomiting and abdominal pain. Extra-intestinal sites include the lung, liver and gall bladder where it causes respiratory cryptosporidosis, hepatitis and cholecystitis.[1][not in citation given]
Infection is caused by ingestion of sporulated oocysts transmitted by the faecal-oral route. In healthy human hosts, the median infective dose is 132 oocysts.[2] The general C. parvum life cycle is shared by other members of the genus. Invasion of the apical tip of ileal enterocytes by sporozoites and merozoites causes pathology seen in the disease.
Infection is generally self-limiting in immunocompetent people. In immunocompromised patients, such as those with AIDS or those undergoing immunosuppressive therapy, infection may not be self-limiting, leading to dehydration and, in severe cases, death.
Detection
Cryptosporidium parvum oocysts are very difficult to detect and therefore diagnose. The oocysts in fecal samples would indicate if the parasite is present in the body but they have a very small size and so detection is made very difficult. Doing a fecal ELISA method to detect the presence of the parasite would eliminate the difficulty due to the small size and many other methods are unable to distinguish between past and present infections; something serological ELISA would not allow to distinguish.[3]
C. parvum is considered to be the most important waterborne pathogen in developed countries. The protozoa also caused the largest waterborne-disease outbreak ever documented in the United States, making 403,000 people ill in Milwaukee, Wisconsin in 1993.[4] It is resistant to all practical levels of Water chlorination, surviving for 24hrs at 1000 mg/L free chlorine. It is an obligate intracellular pathogen.[5]
Prevention
The most effective way to prevent the spread of Cryptosporidium parvum is to avoid the contact of feces that are contaminated. Avoiding this contact, especially with young children is important, as they are more likely to come into oral contact and have the parasite transferred into the body. These ideas of hygiene are the most effective way to combat this difficult to prevent parasite.[6]
Oocyst Stage
The Cryptosporidium parvum oocysts are incredibly durable and this can cause extended problems when attempting to control the spread of the parasite. The oocyst stage can tolerate a vast number of environmental pressures that allows it to be more likely to survive. The oocyst can tolerate temperatures as low as -22C and for long periods of time which means fecal contamination is possible even after going through those environmental extremes. The oocysts can also tolerate shifts in pH that are found in some water treatment process and careful attention to detail must be done to prevent the possibility of infection. The oocysts that are in fecal material are immediately infective and have the potential to find a new host if contamination occurs.[3][6]
Genome
The genome of C. parvum (sequenced in 2004[7]) have a relatively small size and simple organization of 9.1 Mb, which is composed of eight chromosomes ranging from 1.04 to 1.5 Mb. The genome is very compact, and is one of the few organisms without transposable elements. Unlike other apicomplexans, C. parvum has no genes in its plastids or mitochondria.[7]
Treatment
Supportive therapy such as IV fluids is the primary for C. parvum infection. Paromomycin and Nitazoxanide may alleviate some of the diarrhoeal symptoms, however the latter is contraindicated for AIDS patients. Continuing antiretroviral drugs to boost the immune system may also control infection. Research into other potential drugs and therapeutics targets, as well as vaccine candidates, is ongoing. Spiramycin for immunosuppressed patients.
Important C. parvum proteins and drug targets
Lipid metabolism
C. parvum is incapable of de novo lipid synthesis, making its lipid trafficking machinery an important potential therapeutic target. C. parvum possesses multiple oxysterol-binding proteins (OSBPs), and oxysterol related proteins (OSRPs). Only OSBPs are capable of lipid binding, while both contain Pleckstrin homology domains, which function in cell signalling pathways.
Surface glycoproteins
C. parvum possesses numerous surface glycoproteins thought to play a role in pathogenesis. An immunodominant >900kDa protein, known as GP900, localizes to the apical end of sporozoites and in micronemes of merozoites. Its high molecular mass is most likely due to heavy post-translational glycosylation. Indeed, the structure of GP900 is similar to that of a family of glycoproteins known as mucins. GP900 is thought to mediate attachment and invasion to host cells. GP900 may also play a role in C. parvum’s resistance to proteolysis by the numerous proteases found in the mammalian gut.
In vitro, hyperimmune sera as well as antibodies directed at specific epitopes on the GP900 protein inhibit the invasion of C. parvum sporozoites into MDCK cell monolayers. Additionally, competitive inhibition using native GP900 or purified GP900 fragments reduces cell invasion.[8]
Further experiments have confirmed the importance of the mucin-like glycosylations. Lectins directed at GP900 carbohydrate moieties (alpha-N-galactosamine) were able to block adhesion and prevent C. parvum invasion.[9]
C. parvum glycoproteins have the characteristics of attractive vaccine candidates. Many are immunodominant, and antibodies against select domains block invasion of host cells.
References
- ↑ ”Cryptosporidiosis.” Laboratory Identification of Parasites of Public Health Concern. CDC. 5 Sept 2007. <http://www.dpd.cdc.gov/dpdx/HTML/Cryptosporidiosis.htm>
- ↑ DuPont HL, Chappell CL, Sterling CR, Okhuysen PC, Rose JB, Jakubowski W (March 1995). "The infectivity of Cryptosporidium parvum in healthy volunteers". N. Engl. J. Med. 332 (13): 855–9. doi:10.1056/NEJM199503303321304. PMID 7870140.
- ↑ 3.0 3.1 DuPont et al "The Infectivivty of Cryptosporidium parvum in healthy Volunteers" http://www.nejm.org/doi/pdf/10.1056/NEJM199503303321304
- ↑ ”Surveillance for Waterborne-Disease Outbreaks -- United States, 1993-1994” CDC. 1996. <http://www.cdc.gov/mmwr/preview/mmwrhtml/00040818.htm>
- ↑ Deng, M.; Lancto, C. A.; Abrahamsen, M. S. (2004). "Cryptosporidium parvum regulation of human epithelial cell gene expression". International Journal for Parasitology. 34 (1): 73–82. doi:10.1016/j.ijpara.2003.10.001. PMID 14711592.
- ↑ 6.0 6.1 Robertson et al "Survival of Cryposporidium parvum oocysts under various environmental pressures" http://aem.asm.org/content/58/11/3494.full.pdf+html
- ↑ 7.0 7.1 Abrahamsen MS, Templeton TJ; et al. (2004). "Complete genome sequence of the apicomplexan, Cryptosporidium parvum". Science. 304 (5669): 441–5. doi:10.1126/science.1094786. PMID 15044751. Retrieved 2008-05-25.
- ↑ Barnes DA, Bonnin A, Huang JX; et al. (October 1998). "A novel multi-domain mucin-like glycoprotein of Cryptosporidium parvum mediates invasion". Mol. Biochem. Parasitol. 96 (1–2): 93–110. doi:10.1016/S0166-6851(98)00119-4. PMID 9851610.
- ↑ Cevallos AM, Bhat N, Verdon R; et al. (September 2000). "Mediation of Cryptosporidium parvum Infection In Vitro by Mucin-Like Glycoproteins Defined by a Neutralizing Monoclonal Antibody". Infect. Immun. 68 (9): 5167–75. doi:10.1128/IAI.68.9.5167-5175.2000. PMC 101770. PMID 10948140.