Coronary artery bypass surgery conduits used for bypass
|
Coronary Artery Bypass Surgery Microchapters | |
|
Pathophysiology | |
|---|---|
|
Diagnosis | |
|
Treatment | |
|
Perioperative Monitoring | |
|
Surgical Procedure | |
|
Special Scenarios | |
|
Coronary artery bypass surgery conduits used for bypass On the Web | |
|
FDA on Coronary artery bypass surgery conduits used for bypass | |
|
CDC on Coronary artery bypass surgery conduits used for bypass | |
|
Coronary artery bypass surgery conduits used for bypass in the news | |
|
Blogs on Coronary artery bypass surgery conduits used for bypass|- |
|
|
Directions to Hospitals Performing Coronary artery bypass surgery conduits used for bypass | |
|
Risk calculators for Coronary artery bypass surgery conduits used for bypass | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editors-in-Chief: Cafer Zorkun, M.D., Ph.D. [2], Mohammed A. Sbeih, M.D.
Conduits used for bypass
The choice of conduits (arteries and/or veins from elsewhere in the body) to bypass the blockages is highly surgeon and institution dependent. Typically, the left internal thoracic artery (LITA) (also referred to as the left internal mammary artery or LIMA) is grafted to the Left Anterior Descending artery and a combination of other arteries and veins is used for other coronary arteries. The right internal thoracic artery (RITA), the great saphenous vein from the leg and the radial artery from the forearm are frequently used. The right gastroepiploic artery from the stomach is infrequently used given the difficult mobilization from the abdomen.
Saphenous vein
- Saphenous vein anatomy
The great saphenous vein (GSV) is frequently used as a conduit for CABG. It originates from where the dorsal vein of the first digit (the large toe) merges with the dorsal venous arch of the foot.
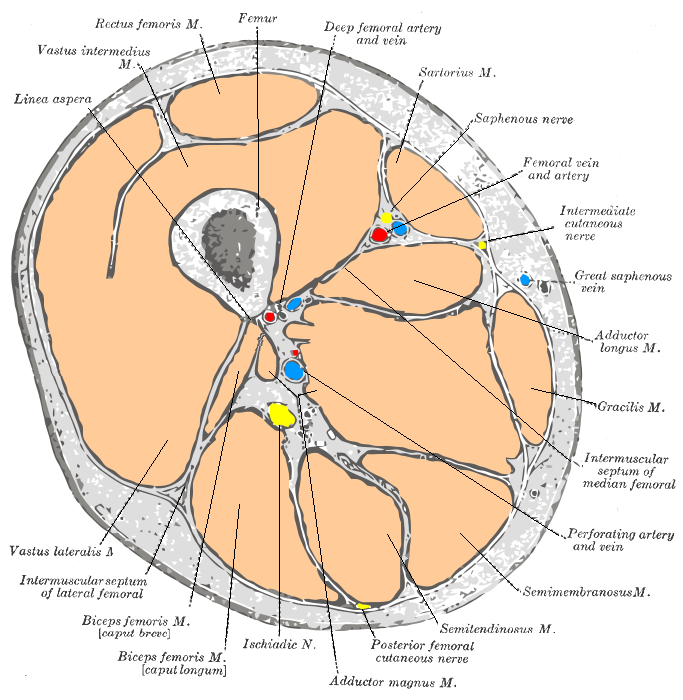
After passing anterior to the medial malleolus (where it often can be visualized and palpated), it runs up the medial side of the leg. At the knee, it runs over the posterior border of the medial epicondyle of the femur bone.
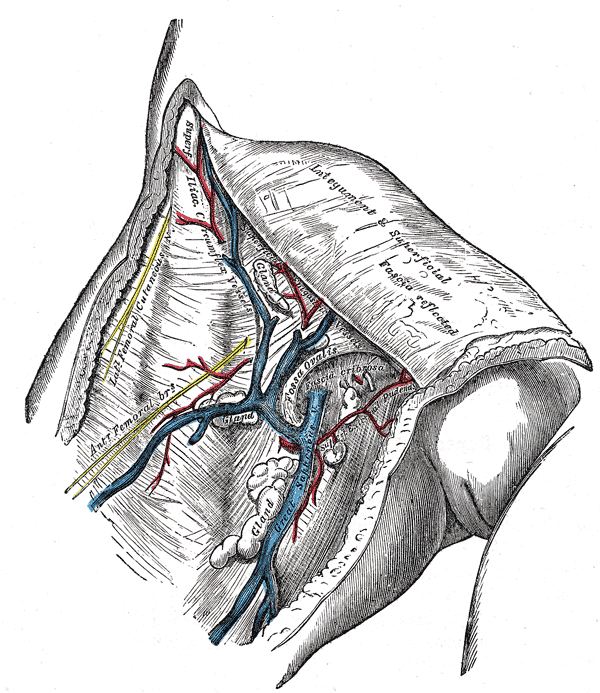
The great saphenous vein then courses laterally to lie on the anterior surface of the thigh before entering an opening in the fascia lata called the saphenous opening. It joins with the femoral vein in the region of the femoral triangle at the saphenofemoral junction.
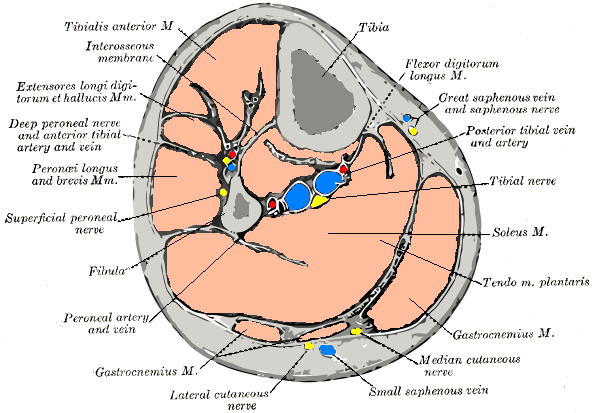
The small saphenous vein (also lesser saphenous vein) originates where the dorsal vein from the fifth digit (smallest toe) merges with the dorsal venous arch of the foot, which attaches to the great saphenous vein. It is considered a superficial vein and is subcutaneous (just under the skin). From its origin, it courses around the lateral aspect of the foot (inferior and posterior to the lateral malleolus) and runs along the posterior aspect of the leg (with the sural nerve), passes between the heads of the gastrocnemius muscle, and drains into the popliteal vein, approximately at or above the level of the knee joint.
-
Cross-section through the middle of the thigh.
-
Cross-section through middle of leg.
-
The great saphenous vein and landmarks along its course
-
The great saphenous vein and its tributaries at the fossa ovalis in the groin.
-
Small saphenous vein and its tributaries.
- Saphenous vein harvesting
The saphenous vein can be harvested by either direct visualization or via an endoscopic approach. Veins that are used either have their valves removed or are turned around so that the valves in them do not occlude blood flow in the graft. The technique of saphenous vein harvesting may influence later SVG patency. The process of harvesting the vein and pressure testing the vein for a leak may damage the endothelium.[1][2]
The endoscopic approach has been associated with lower rates of wound infection, greater patient satisfaction, and earlier mobilization.[3][4][5][6] One small randomized study of 144 patients showed no difference in histologic findings between the traditional and endoscopic techniques.[3]In another small study of 40 patients randomized to the two techniques, no difference was seen in angiographic patency at 3 months.[6]Another small randomized study of 144 patients who returned for angiography demonstrated an occlusion rate of 21.7% for the endoscopic approach vs 17.6% for the open approach.[5] However, non- randomized data from a much larger multicenter study does suggest that endoscopic harvesting may be associated with higher rates of failure and adverse events such as death and MI.[4]
Complications associated with saphenous vein harvesting include the following:
- Saphenous nerve injury
- Infection at incision sites or sepsis.
- Deep vein thrombosis (DVT)
- Keloid scarring
- Chronic pain at incision sites
The right internal thoracic artery (RITA)
In multiple arterial revascularizations during Coronary artery bypass surgery, the right internal thoracic artery (RITA) has been proofed to be a better choice as a conduit than the radial artery. This has been published at the European Society of Cardiology (ESC) 2011 Congress, after a trial on more than 1000 patients who had the operation in a 10 years trial.
The left internal thoracic artery (LITA) (also known as the left internal mammary artery (LIMA)) is the best vessel to use for Coronary artery bypass surgery when only one artery is required.
It was known that the long-term outcomes of the arterial grafts is much better than saphenous vein grafts (SVGs) and has less morbidity and mortality rates. The right internal thoracic artery (RITA) is the best second conduit for the bypass and has better long-term outcomes than the radial artery. The use of the right internal thoracic artery (RITA) results in the following in compare with SVG:
- Less major adverse cardiac and cerebrovascular events.
- Less perioperative myocardial infarction rates.
- Less perioperative stroke rates.
- Less cardiac-related deaths.
There have been good clinical results with single left internal thoracic artery grafting compared with saphenous vein grafting. This prompted surgeons to use both ITAs. Bilateral ITA grafting could improve long term survival. Late complications like myocardial infarction and need to re-operate may be avoided. However, mathematical modelling is required to assist in developing a strategy for use of such grafts.[7]
In a cohort study of 8123 patients who received single internal thoracic artery grafts and 2001 who received bilateral internal thoracic artery grafts for multivessel coronary disease for a duration of 20 years, it was found that the latter produces improved survival compared with single internal thoracic artery grafting during the second postoperative decade, and the magnitude of that benefit increases through 20 postoperative years.[8]
It's easy to harvest the Radial artery, but it has a higher risk for vasospasm and atherosclerosis than the right internal thoracic artery (RITA). Some institution solves this problem (vasospasm) by preparing the radial arteries with phenoxybenzamine.
Although the fact that using both internal thoracic arteries for Coronary artery bypass surgery takes longer time, it has better long-term results and perioperative outcomes. This has to be proofed and confirmed by more randomized and controlled trials.
Conduit Nomenclature
The terms single bypass, double bypass, triple bypass, quadruple bypass and quintuple bypass refer to the number of coronary arteries bypassed in the procedure.
In other words, a double bypass means two coronary arteries are bypassed (e.g. the left anterior descending (LAD) coronary artery and right coronary artery (RCA)); a triple bypass means three vessels are bypassed (e.g. LAD, RCA, left circumflex artery (LCX)); a quadruple bypass means four vessels are bypassed (e.g. LAD, RCA, LCX, first diagonal artery of the LAD) while quintuple means five. Less commonly more than four coronary arteries may be bypassed.
A greater number of bypasses does not imply a person is "sicker," nor does a lesser number imply a person is "healthier."[9] A person with a large amount of coronary artery disease (CAD) may receive fewer bypass grafts owing to the lack of suitable "target" vessels.
A patient with a single stenosis ("narrowing") of the left main coronary artery often requires only two bypasses (to the LAD and the LCX). However, depending upon the anatomy, grafts may also need to be placed to a large diagonal artery, or to additional large obtuse marginal branches.
Assessment of Target Vessels for Bypass Grafting
A coronary artery may be unsuitable for bypass grafting for the following reasons:
- Size: If the native target artery it is small (< 1 mm or < 1.5 mm depending on surgeon preference)
- Location: Some distal locations of the native target artery may not be accessible, or a conduit may not reach the far down the native artery.
- Native artery calcification: Heavily calcified native arteries are sometimes technically not amenable to anastamosis of a conduit.
- Diffuse disease: The native artery may not have a section of vessel that has minimal disease where a conduit can be grafted to.
- The native artery lies in the heart muscle or is intramyocardial: In this scenario the native coronary artery is located within the heart muscle rather than on the surface of the heart and a graft cannot be attached to it.
Although the cardiothoracic surgeon reviews the coronary angiogram prior to surgery and identifies the lesions (or "blockages") in the coronary arteries and will estimate the number of bypass grafts prior to surgery, the final decision is made in the operating room based upon the direct examination of the heart and the suitability of the native target vessel for bypassing.
2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery (DO NOT EDIT)[10]
Bypass Graft Conduit (DO NOT EDIT)[10]
| Class I |
| "1. If possible, the left internal mammary artery (LIMA) should be used to bypass the left anterior descending (LAD) artery when bypass of the LAD artery is indicated.[11][12][13][14] (Level of Evidence: B)" |
| Class III: HARM |
| "1. An arterial graft should not be used to bypass the right coronary artery with less than a critical stenosis (<90%).[14] (Level of Evidence: C)" |
| Class IIa |
| "1. The right internal mammary artery is probably indicated to bypass the LAD artery when the LIMA is unavailable or unsuitable as a bypass conduit. (Level of Evidence: C)" |
| "2. When anatomically and clinically suitable, use of a second internal mammary artery to graft the left circumflex or right coronary artery (when critically stenosed and perfusing LV myocardium) is reasonable to improve the likelihood of survival and to decrease reintervention.[15][8][16][17][18] (Level of Evidence: B)" |
| Class IIb |
| "1. Complete arterial revascularization may be reasonable in patients less than or equal to 60 years of age with few or no comorbidities. (Level of Evidence: C)" |
| "2. Arterial grafting of the right coronary artery may be reasonable when a critical (≥90%) stenosis is present.[14][17][19] (Level of Evidence: B)" |
| "3. Use of a radial artery graft may be reasonable when grafting left-sided coronary arteries with severe stenoses (>70%) and right-sided arteries with critical stenoses (≥90%) that perfuse LV myocardium.[20][21][22][23][24][25] (Level of Evidence: B)" |
References
- ↑ Lawrie GM, Weilbacher DE, Henry PD. Endothelium-dependent relaxation in human saphenous vein grafts. Effects of preparation and clinicopathologic correlations. J Thorac Cardiovasc Surg 1990;100:612—20.
- ↑ Souza DS, Johansson B, Bojo¨ L, Karlsson R, Geijer H, Filbey D, Bodin L, Arbeus M, Dashwood MR. Harvesting the saphenous vein with surrounding tissue for CABG provides long-term graft patency comparable to the left internal thoracic artery: results of a randomized longitudinal trial. J Thorac Cardiovasc Surg 2006;132:373—8.
- ↑ 3.0 3.1 Kiaii B, Moon BC, Massel D, Langlois Y, Austin TW, Willoughby A, Guiraudon C, Howard CR, Guo LR (2002). "A prospective randomized trial of endoscopic versus conventional harvesting of the saphenous vein in coronary artery bypass surgery". J. Thorac. Cardiovasc. Surg. 123 (2): 204–12. PMID 11828277. Retrieved 2010-07-23. Unknown parameter
|month=ignored (help) - ↑ 4.0 4.1 Lopes RD, Hafley GE, Allen KB, Ferguson TB, Peterson ED, Harrington RA, Mehta RH, Gibson CM, Mack MJ, Kouchoukos NT, Califf RM, Alexander JH (2009). "Endoscopic versus open vein-graft harvesting in coronary-artery bypass surgery". The New England Journal of Medicine. 361 (3): 235–44. doi:10.1056/NEJMoa0900708. PMID 19605828. Retrieved 2010-07-12. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 Yun KL, Wu Y, Aharonian V, Mansukhani P, Pfeffer TA, Sintek CF, Kochamba GS, Grunkemeier G, Khonsari S (2005). "Randomized trial of endoscopic versus open vein harvest for coronary artery bypass grafting: six-month patency rates". J. Thorac. Cardiovasc. Surg. 129 (3): 496–503. doi:10.1016/j.jtcvs.2004.08.054. PMID 15746730. Retrieved 2010-07-23. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Perrault LP, Jeanmart H, Bilodeau L, Lespérance J, Tanguay JF, Bouchard D, Pagé P, Carrier M (2004). "Early quantitative coronary angiography of saphenous vein grafts for coronary artery bypass grafting harvested by means of open versus endoscopic saphenectomy: a prospective randomized trial". J. Thorac. Cardiovasc. Surg. 127 (5): 1402–7. doi:10.1016/j.jtcvs.2003.10.040. PMID 15115999. Retrieved 2010-07-23. Unknown parameter
|month=ignored (help) - ↑ Buxton BF, Komeda M, Fuller JA, Gordon I (1998). "Bilateral internal thoracic artery grafting may improve outcome of coronary artery surgery. Risk-adjusted survival". Circulation. 98 (19 Suppl): II1–6. PMID 9852872.
- ↑ 8.0 8.1 Lytle BW, Blackstone EH, Sabik JF, Houghtaling P, Loop FD, Cosgrove DM (2004). "The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years". Ann Thorac Surg. 78 (6): 2005–12, discussion 2012-4. doi:10.1016/j.athoracsur.2004.05.070. PMID 15561021.
- ↑ Ohki S, Kaneko T, Satoh Y; et al. (2002). "[Coronary artery bypass grafting in octogenarian]". Kyobu geka. The Japanese journal of thoracic surgery (in Japanese). 55 (10): 829–33, discussion 833–6. PMID 12233100.
- ↑ 10.0 10.1 Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG; et al. (2011). "2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0b013e31823c074e. PMID 22064599.
- ↑ Boylan MJ, Lytle BW, Loop FD, Taylor PC, Borsh JA, Goormastic M; et al. (1994). "Surgical treatment of isolated left anterior descending coronary stenosis. Comparison of left internal mammary artery and venous autograft at 18 to 20 years of follow-up". J Thorac Cardiovasc Surg. 107 (3): 657–62. PMID 8127094.
- ↑ Cameron A, Davis KB, Green G, Schaff HV (1996). "Coronary bypass surgery with internal-thoracic-artery grafts--effects on survival over a 15-year period". N Engl J Med. 334 (4): 216–9. doi:10.1056/NEJM199601253340402. PMID 8531997.
- ↑ Loop FD, Lytle BW, Cosgrove DM, Stewart RW, Goormastic M, Williams GW; et al. (1986). "Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events". N Engl J Med. 314 (1): 1–6. doi:10.1056/NEJM198601023140101. PMID 3484393.
- ↑ 14.0 14.1 14.2 Sabik JF, Lytle BW, Blackstone EH, Houghtaling PL, Cosgrove DM (2005). "Comparison of saphenous vein and internal thoracic artery graft patency by coronary system". Ann Thorac Surg. 79 (2): 544–51, discussion 544-51. doi:10.1016/j.athoracsur.2004.07.047. PMID 15680832.
- ↑ Lytle BW, Blackstone EH, Loop FD, Houghtaling PL, Arnold JH, Akhrass R; et al. (1999). "Two internal thoracic artery grafts are better than one". J Thorac Cardiovasc Surg. 117 (5): 855–72. PMID 10220677.
- ↑ Sabik JF, Blackstone EH, Gillinov AM, Banbury MK, Smedira NG, Lytle BW (2006). "Influence of patient characteristics and arterial grafts on freedom from coronary reoperation". J Thorac Cardiovasc Surg. 131 (1): 90–8. doi:10.1016/j.jtcvs.2005.05.024. PMID 16399299.
- ↑ 17.0 17.1 Sabik JF, Stockins A, Nowicki ER, Blackstone EH, Houghtaling PL, Lytle BW; et al. (2008). "Does location of the second internal thoracic artery graft influence outcome of coronary artery bypass grafting?". Circulation. 118 (14 Suppl): S210–5. doi:10.1161/CIRCULATIONAHA.107.760827. PMID 18824756.
- ↑ Stevens LM, Carrier M, Perrault LP, Hébert Y, Cartier R, Bouchard D; et al. (2004). "Single versus bilateral internal thoracic artery grafts with concomitant saphenous vein grafts for multivessel coronary artery bypass grafting: effects on mortality and event-free survival". J Thorac Cardiovasc Surg. 127 (5): 1408–15. doi:10.1016/j.jtcvs.2003.10.006. PMID 15116000.
- ↑ Sabik JF, Lytle BW, Blackstone EH, Khan M, Houghtaling PL, Cosgrove DM (2003). "Does competitive flow reduce internal thoracic artery graft patency?". Ann Thorac Surg. 76 (5): 1490–6, discussion 1497. PMID 14602274.
- ↑ Acar C, Ramsheyi A, Pagny JY, Jebara V, Barrier P, Fabiani JN; et al. (1998). "The radial artery for coronary artery bypass grafting: clinical and angiographic results at five years". J Thorac Cardiovasc Surg. 116 (6): 981–9. PMID 9832690.
- ↑ Maniar HS, Sundt TM, Barner HB, Prasad SM, Peterson L, Absi T; et al. (2002). "Effect of target stenosis and location on radial artery graft patency". J Thorac Cardiovasc Surg. 123 (1): 45–52. PMID 11782755.
- ↑ Moran SV, Baeza R, Guarda E, Zalaquett R, Irarrazaval MJ, Marchant E; et al. (2001). "Predictors of radial artery patency for coronary bypass operations". Ann Thorac Surg. 72 (5): 1552–6. PMID 11722042.
- ↑ Possati G, Gaudino M, Alessandrini F, Luciani N, Glieca F, Trani C; et al. (1998). "Midterm clinical and angiographic results of radial artery grafts used for myocardial revascularization". J Thorac Cardiovasc Surg. 116 (6): 1015–21. PMID 9832694.
- ↑ Royse AG, Royse CF, Tatoulis J, Grigg LE, Shah P, Hunt D; et al. (2000). "Postoperative radial artery angiography for coronary artery bypass surgery". Eur J Cardiothorac Surg. 17 (3): 294–304. PMID 10758391.
- ↑ Desai ND, Cohen EA, Naylor CD, Fremes SE, Radial Artery Patency Study Investigators (2004). "A randomized comparison of radial-artery and saphenous-vein coronary bypass grafts". N Engl J Med. 351 (22): 2302–9. doi:10.1056/NEJMoa040982. PMID 15564545.