Chronic stable angina treatment lipid management
|
Chronic stable angina Microchapters | ||
|
Classification | ||
|---|---|---|
| ||
| ||
|
Differentiating Chronic Stable Angina from Acute Coronary Syndromes | ||
|
Diagnosis | ||
|
Alternative Therapies for Refractory Angina | ||
|
Discharge Care | ||
|
Guidelines for Asymptomatic Patients | ||
|
Case Studies | ||
|
Chronic stable angina treatment lipid management On the Web | ||
|
Chronic stable angina treatment lipid management in the news | ||
|
to Hospitals Treating Chronic stable angina treatment lipid management | ||
|
Risk calculators and risk factors for Chronic stable angina treatment lipid management | ||
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor(s)-In-Chief: Lakshmi Gopalakrishnan. M.B.B.S.; Aysha Anwar, M.B.B.S[3]
Overview
In patients with established coronary artery disease, the recommended goal for total cholesterol is 130 mg/dl and LDL-C is 100 mg/dl, while the HDL-C and triglyceride concentrations serve as preferred markers for risk assessment.[1] In patients with CAD, a fasting lipid-profile may be repeated at 5 year intervals to assess the overall risk of cardiovascular mortality and morbidity.[2] Based on the individual’s lipid abnormalities, necessary dietary interventions and/or lipid-lowering agents are suggested to prevent the risk of future coronary events.[3] A Mediterranean diet consisting of fruits, vegetables, lean meat and fish has also been shown to be beneficial. Omega-3 fatty acid supplementation may be indicated in patients with stable angina for secondary prevention, as it has been shown to reduce elevated triglycerides and also reduce the risk of sudden cardiac death.[4][5][6][7] Fish consumption once a week has also been associated with reduced risk of mortality from coronary artery disease and, for this reason, is strongly recommended.[8][9]
Lipid Management
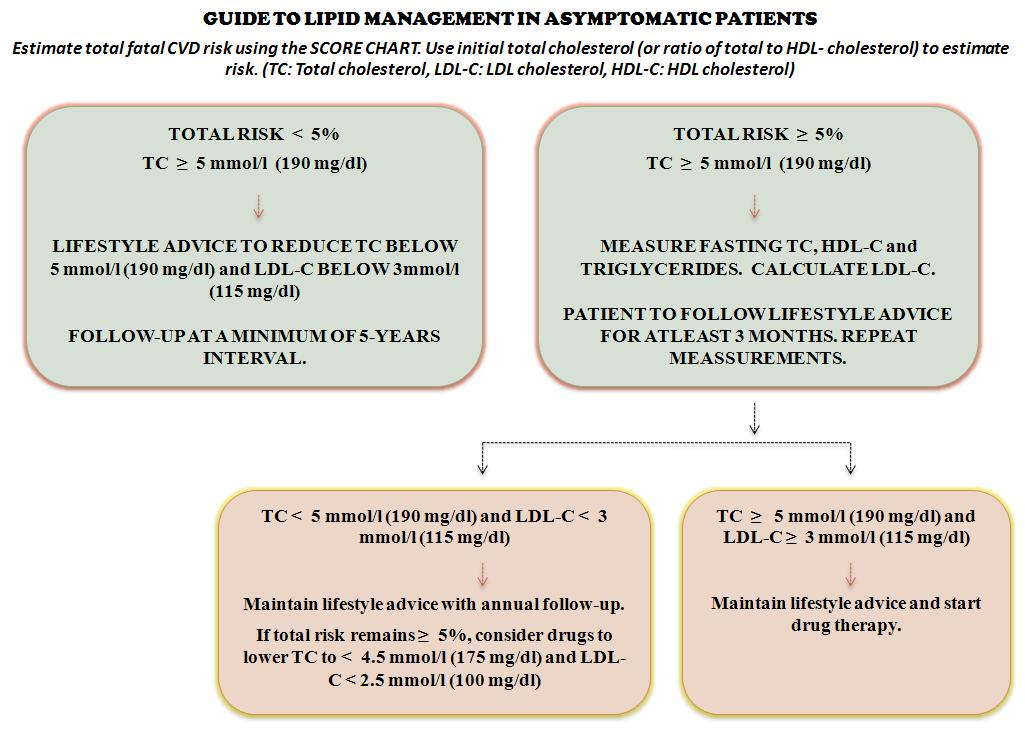
Guide to Lipid Management Adapted from the European Task Force[2]
| “ |
 |
” |
Supportive Trial Data
- The Whitehall Study, a cohort study of 17,718 male civil servants aged 40 through 64 years of age at enrollment with an average follow-up of 18 years of study, evaluated the relationship between plasma cholesterol concentration and mortality from major causes of death. Researchers reported a significant increase in mortality from coronary artery disease associated with increasing cholesterol concentration from the lowest levels (p < 0.01).[3]
- The GISSI-Prevenizone trial, a multi-center interventional trial involving 11,324 participants (both male and female) with a history of recent MI who were randomized to receive either omega-3 PUFA (1 g daily), vitamin E (300 mg daily) or a combination of both, evaluated the effects of omega-3 polyunsaturated fatty acids and vitamin E as supplements in patients who had myocardial infarction. Researchers observed a significant reduction over 3-5 years in the n-3 PUFA treatment group in the rate of death, non-fatal myocardial infarction and stroke. No effect was cene for the vitamin E treatment group. Based on this evidence and the supporting data of similar trials such as DART, the study investigators concluded that dietary supplementation with omega-3 PUFA provided significant benefit in improving the overall clinical outcome of patients with ischemic heart disease.[4]
- The GISSI-Prevenzione sub-study, an investigation within the GISSI-Prevenzione trial data of 11,323 patients (both, male and female) with a history of recent (<3 months) myocardial infarction, assessed the time course of benefit of omega-3 polyunsaturated fatty acids. Researchers attributed the anti-arryhthmic effect of omega-3 PUFA, a finding consistent with previous randomized clinical trials, to a significant early reduction in the total mortality (RR 0.59, 95% CI 0.36, 0.97; P=0.037) and sudden cardiac death (RR 0.47, 95% CI 0.219, 0.995; p=0.048).[5]
- Observational studies have been inconsistent in defining the association between omega-3 polyunsaturated fatty acids and coronary artery disease risk. Therefore, researchers conducted a meta-analysis of randomized controlled trials that compared dietary and non-deitary supplementation of omega-3 polyunsaturated fatty acids on coronary heart disease. The analysis reported a significant reduction in the risk of fatal myocardial infarction (RR 0.7; 95% CI: 0.6, 0.8; p<0.001) and sudden cardiac death (RR 0.7; 95% CI: 0.6, 0.9; p<0.01). Thus, the study concluded omega-3 polyunsaturated fatty acid consumption significantly reduced the overall mortality, mortality due to myocardial infarction and sudden cardiac death; however, these benefits were confined to high-risk patients.[6]
- A 2005 meta-analysis, which reviewed 97 randomized control trials, evaluated the efficacy and safety of different lipid-lowering interventions based on mortality data. Researchers reported a significant reduction in overall cardiovascular mortality associated with omega-3 polyunsaturated fatty acid supplementation. It was further suggested that this therapy could be utilized in patients with stable angina for secondary prevention purposes.[7]
2012 Chronic Angina ACC/AHA Guidelines for the Management of Patients With Chronic Stable Angina (DO NOT EDIT)[10]
Lipid Management (DO NOT EDIT)[10]
| Class I |
| "1. Lifestyle modifications, including daily physical activity and weight management, are strongly recommended for all patients with SIHD. (Level of Evidence: B) " |
| "2. Dietary therapy for all patients should include reduced intake of saturated fats (to <7% of total calories), trans fatty acids (to <1%of total calories), and cholesterol (to <200 mg/d). (Level of Evidence: B) " |
| "3. In addition to therapeutic lifestyle changes, a moderate or high dose of a statin therapy should be prescribed, in the absence of contraindications or documented adverse effects.(Level of Evidence: A) " |
| Class IIa |
| "1. For patients who do not tolerate statins, low-density lipoproteincholesterol–lowering therapy with bile acid sequestrants,* niacin,† or both is reasonable. (Level of Evidence: B) " |
References
- ↑ Fraker TD, Fihn SD, Gibbons RJ, Abrams J, Chatterjee K, Daley J et al. (2007)2007 chronic angina focused update of the ACC/AHA 2002 Guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 Guidelines for the management of patients with chronic stable angina. Circulation 116 (23):2762-72.[1] PMID: 17998462
- ↑ 2.0 2.1 De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J et al. (2003) European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J 24 (17):1601-10. PMID: 12964575
- ↑ 3.0 3.1 Smith GD, Shipley MJ, Marmot MG, Rose G (1992) Plasma cholesterol concentration and mortality. The Whitehall Study. JAMA 267 (1):70-6. PMID: 1727199
- ↑ 4.0 4.1 (1999) Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto miocardico. Lancet 354 (9177):447-55. PMID: 10465168
- ↑ 5.0 5.1 Marchioli R, Barzi F, Bomba E, Chieffo C, Di Gregorio D, Di Mascio R et al. (2002) Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI)-Prevenzione. Circulation 105 (16):1897-903. PMID: 11997274
- ↑ 6.0 6.1 Bucher HC, Hengstler P, Schindler C, Meier G (2002) N-3 polyunsaturated fatty acids in coronary heart disease: a meta-analysis of randomized controlled trials. Am J Med 112 (4):298-304. PMID: 11893369
- ↑ 7.0 7.1 Studer M, Briel M, Leimenstoll B, Glass TR, Bucher HC (2005) Effect of different antilipidemic agents and diets on mortality: a systematic review. Arch Intern Med 165 (7):725-30. DOI:10.1001/archinte.165.7.725 PMID: 15824290
- ↑ Kris-Etherton PM, Harris WS, Appel LJ, Nutrition Committee (2003) Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Arterioscler Thromb Vasc Biol 23 (2):e20-30. PMID: 12588785
- ↑ He K, Song Y, Daviglus ML, Liu K, Van Horn L, Dyer AR et al. (2004) Accumulated evidence on fish consumption and coronary heart disease mortality: a meta-analysis of cohort studies. Circulation 109 (22):2705-11. DOI:10.1161/01.CIR.0000132503.19410.6B PMID: 15184295
- ↑ 10.0 10.1 Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP; et al. (2012). "2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 126 (25): 3097–137. doi:10.1161/CIR.0b013e3182776f83. PMID 23166210.