Candida vulvovaginitis pathophysiology: Difference between revisions
Dima Nimri (talk | contribs) |
Dima Nimri (talk | contribs) |
||
| Line 43: | Line 43: | ||
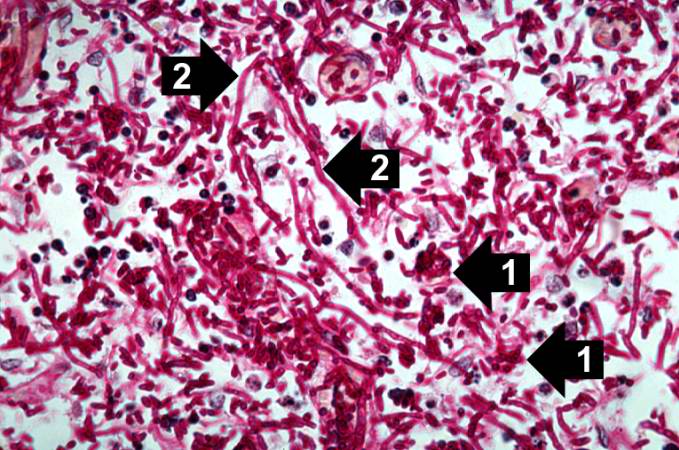
Image:Renal candidiasis 006.jpeg|left|thumb|350px|This high-power photomicrograph shows the yeasts (1) and pseudohyphae (2). | Image:Renal candidiasis 006.jpeg|left|thumb|350px|This high-power photomicrograph shows the yeasts (1) and pseudohyphae (2). | ||
<br clear="left"/> | <br clear="left"/> | ||
</gallery> | </gallery> | ||
Revision as of 18:02, 20 October 2016
|
Candidiasis Main page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Dima Nimri, M.D. [2]
Overview
Several virulence factors of Candida are implicated in vulvovaginitis, but the process of transition from asymptomatic vaginal colonization to symptomatic vulvovaginitis is poorly understood. There may be genetic factors associated with Candida vulvovaginitis, as infection runs in families in many cases and is more common in African-American women.
Pathophysiology
Pathogenesis
- All strains of C. albicans possess a yeast surface mannoprotein. This allows the various strains to adhere to both the exfoliated and buccal epithelial cells of the vagina.[1][2]
- Several virulence factors of Candida are implicated in vulvovaginitis. These include proteolytic enzymes, toxins and phospholipase. Proteolytic enzymes destroy the proteins that normally impair fungal invasion, allowing for Candida to colonize the vagina.[1][2][3]
- The understanding of the transition from asymptomatic vaginal colonization with Candida to symptomatic vulvovaginitis is not clear.[2][3]
Genetics
Genetic factors could be involved in the pathophysiology of Candida vulvovaginitis. Supporting evidence is that many cases were found to be more common in African-American women, run in families, as well as being associated with ABO-Lewis non-secretor phenotype, a rare blood group. In addition, women with Candida vulvovaginitis were found to have decreased concentrations of mannose binding lectin (MBL), hence, the variant (MBL) gene is thought to be a contributing factor in the development of Candida vulvovaginitis.[1][4][5]
Gross Pathology
-
This photograph is a speculum examination of the vagina with Candida infection and the typical thick, curdy vaginal discharge.
-
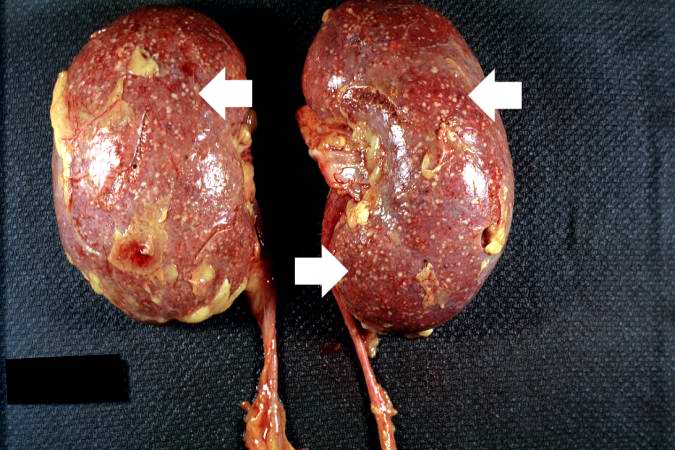
This autopsy photograph of the kidneys demonstrates the multifocal punctate lesions visible on the serosal surface (arrows). Don't confuse these small yellow punctate lesions with the fat that is adherent to the renal capsule.
-
This photograph of the cut surface of these kidneys shows that these multifocal punctate lesions are primarily in the cortex (arrows).
Microscopic Pathology
-
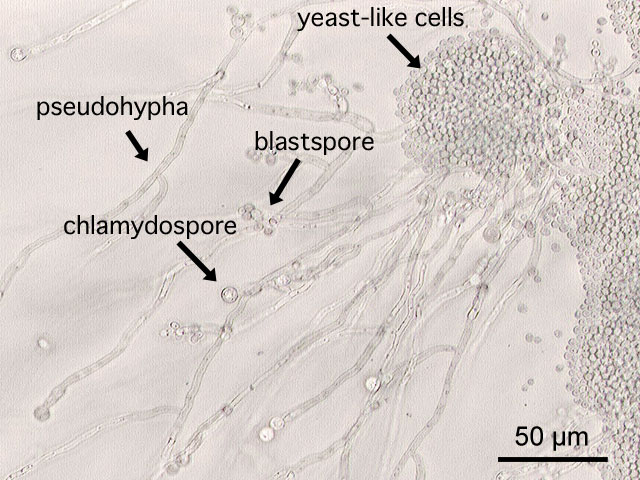
This is a a microscopic image of Candida albicans, grown on cornmeal agar medium.
-
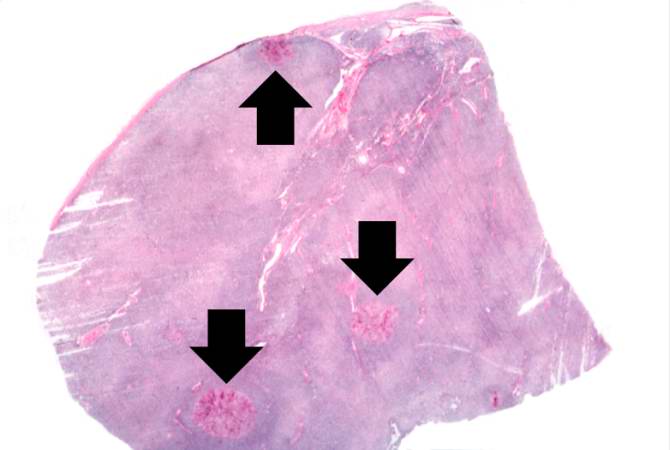
This is a low-power photomicrograph of lymph node with three prominent areas of Candida colonies (arrows). Even at this low magnification, the purple-staining yeast and pseudohyphae can be easily seen. This section was stained with Periodic Acid-Schiff Hematoxylin (PASH), which stains the cell wall of fungi to make them more easily visible.
-
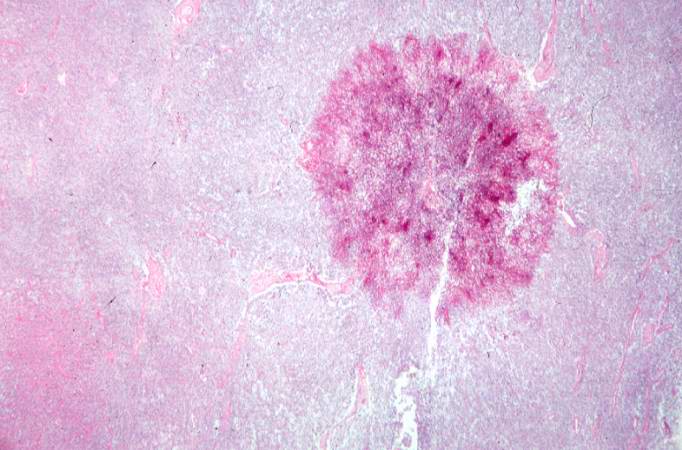
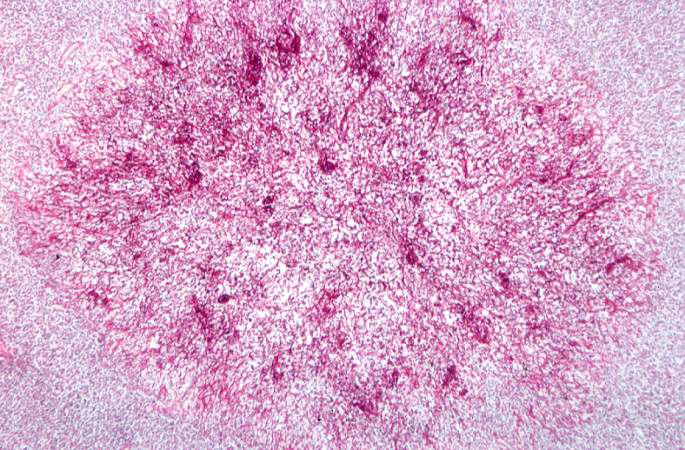
This is a low-power photomicrograph of one of the Candida colonies from this lymph node. The chains of yeast which are termed "pseudohyphae" are apparent at this magnification.
-
This higher-power photomicrograph shows the yeasts and pseudohyphae in this focus of Candida organisms.
-
This high-power photomicrograph shows the yeasts (1) and pseudohyphae (2).
Associated Conditions
- Candida vulvovaginitis may be associated with other pathogens that cause vulvovaginitis. These include Trichomonas vaginalis and Gardnerella vaginalis. The association may be a mixed infection, where 2 or more pathogens are symptomatic, or a co-infection, in which there are 2 or more pathogens but some are not symptomatic.[6][7]
References
- ↑ 1.0 1.1 1.2 Sobel JD (2007). "Vulvovaginal candidosis". Lancet. 369 (9577): 1961–71. doi:10.1016/S0140-6736(07)60917-9. PMID 17560449.
- ↑ 2.0 2.1 2.2 Sobel JD (1985). "Epidemiology and pathogenesis of recurrent vulvovaginal candidiasis". Am. J. Obstet. Gynecol. 152 (7 Pt 2): 924–35. PMID 3895958.
- ↑ 3.0 3.1 Sobel JD (1989). "Pathogenesis of Candida vulvovaginitis". Curr Top Med Mycol. 3: 86–108. PMID 2688924.
- ↑ Liu F, Liao Q, Liu Z (2006). "Mannose-binding lectin and vulvovaginal candidiasis". Int J Gynaecol Obstet. 92 (1): 43–7. doi:10.1016/j.ijgo.2005.08.024. PMID 16256117.
- ↑ Donders GG, Babula O, Bellen G, Linhares IM, Witkin SS (2008). "Mannose-binding lectin gene polymorphism and resistance to therapy in women with recurrent vulvovaginal candidiasis". BJOG. 115 (10): 1225–31. doi:10.1111/j.1471-0528.2008.01830.x. PMID 18715406.
- ↑ Sobel JD, Subramanian C, Foxman B, Fairfax M, Gygax SE (2013). "Mixed vaginitis-more than coinfection and with therapeutic implications". Curr Infect Dis Rep. 15 (2): 104–8. doi:10.1007/s11908-013-0325-5. PMID 23354954.
- ↑ Anderson MR, Klink K, Cohrssen A (2004). "Evaluation of vaginal complaints". JAMA. 291 (11): 1368–79. doi:10.1001/jama.291.11.1368. PMID 15026404.