COVID-19-associated pulmonary embolism
Pulmonary embolism=
- In May 2020, various autopsies studies revealed pulmonary embolism to be the common cause of death in COVID-19 infected patients.
- These patients in their mid-70s had preexisting medical conditions such as cardiac diseases, hypertension, diabetes, and obesity.[1]
- These studies highlight the role of hypercoagulability as the main contributor to the fatality in these patients.
- Various studies have described Virchow's triad to be the main component of the hypercoagulable state in these patients.
Epidemiology
- Various case reports and case series report relatively high incidence of pulmonary embolism in ICU patients.
- The incidence of thrombotic complications is reported to be 31 % in one study. In this study pulmonary embolism was the most common thrombotic complication.[2]
- Another study reported an overall 24% cumulative incidence of pulmonary embolism in patients with COVID-19 pneumonia, 50% (30–70%) in ICU and 18% (12–27%) in other patients. [3]
- In Non-ICU settings (In-patient), pulmonary embolism is reported to occur in 3% percent of patients in one study.[4]
Risk Factors
Multivariate analysis showed following risk factors that predispose a patient of COVID-19 to pulmonary embolism [5]
| Risk factors predisposing a COVID-19 patient to pulmonary embolism |
|---|
|
Pathogenesis
- As data on COVID-19 has been incomplete and evolving, the pathogenesis of pulmonary embolism has not yet been completely understood. Various contributors to the pathogenesis of pulmonary embolism in these patients are listed in the table below:
| Pathology | Description of the underlying mechanism |
|---|---|
| Endothelial cells dysfunction[6] |
|
| Stasis | Most hospitalized critically ill immobile COVID-19 patients are prone to stasis of blood flow leading to another contributor towards the pathogenesis of pulmonary embolism. |
| Hypercoagulable state[7] |
Various clinical studies have reported different prothrombotic factors in patients who are critically ill and are hospitalized due to COVID-19. These studies report various key lab factors that play an important role in the pathogenesis of pulmonary embolism.
|
Clinical Features
- Pulmonary embolism can present with no symptoms to shock and even sudden cardiac arrest.
- The most common symptoms that were observed in Prospective Investigation of Pulmonary Embolism Diagnosis II (PIOPED II) trial include:[8]
- Dyspnea that is sudden in onset at rest or exertion (73%)
- Pleuritic pain (44%)
- Calf or thigh pain (44%)
- Calf or thigh swelling (41%)
- Cough (34%)
Diagnosis
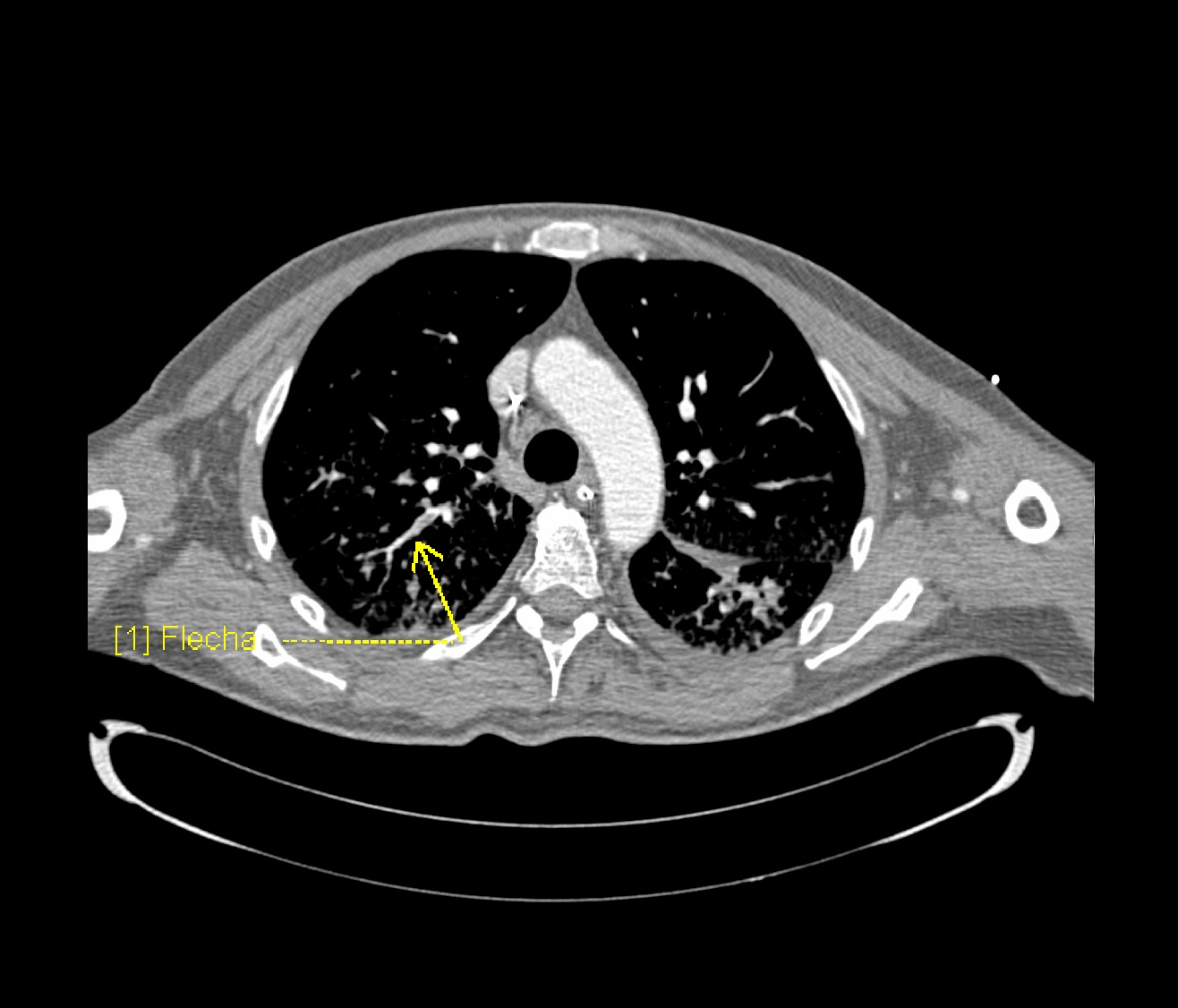
Imaging studies
- Prompt diagnosis of PE in COVID-19 patient is difficult in this regard that various symptoms of COVID-19 overlap with that of pulmonary embolism. American Society of Hematology provides the following guidelines regarding the diagnosis of pulmonary embolism:[9]
- Normal d-dimers level in a patient with low to moderate pretest probability is sufficient to rule out the diagnosis of PE. D-dimers level is usually elevated in COVID-19 patients. This is not applicable to a patient with a high pretest probability.
- Inpatient with suspected PE with symptoms like hypotension, tachycardia, and sudden drop in oxygen saturation with a high pretest probability of PE, computed tomography with pulmonary angiography is used for the diagnosis. Contraindication to the use of CTPA warrants investigation with ventilation/perfusion scan.
Laboratory findings
Lab findings of different case studies of patients having pulmonary embolism due to COVID-19 are given as [10]
- Elevated d-dimers
- Elevated prothrombin time
- Elevated CRP
- Elevated Cardiac biomarkers
- High fibrinogen
- Mild thrombocytopenia or thrombocytosis
- Platelet count can be normal
Treatment
- Different treatment strategies for COVID-19 patients suffering from pulmonary embolism are given in the table below:
| Different treatment options | Details |
|---|---|
| Prophylaxis | All hospitalized patients with COVID 19 should get proper venous thromboembolism prophylaxis in the absence of any contraindication of anticoagulation.
|
| Acute Pulmonary embolism |
|
| Outpatient treatment[9] |
|

- ↑ Wichmann, Dominic; Sperhake, Jan-Peter; Lütgehetmann, Marc; Steurer, Stefan; Edler, Carolin; Heinemann, Axel; Heinrich, Fabian; Mushumba, Herbert; Kniep, Inga; Schröder, Ann Sophie; Burdelski, Christoph; de Heer, Geraldine; Nierhaus, Axel; Frings, Daniel; Pfefferle, Susanne; Becker, Heinrich; Bredereke-Wiedling, Hanns; de Weerth, Andreas; Paschen, Hans-Richard; Sheikhzadeh-Eggers, Sara; Stang, Axel; Schmiedel, Stefan; Bokemeyer, Carsten; Addo, Marylyn M.; Aepfelbacher, Martin; Püschel, Klaus; Kluge, Stefan (2020-05-06). "Autopsy Findings and Venous Thromboembolism in Patients With COVID-19". Annals of Internal Medicine. American College of Physicians. doi:10.7326/m20-2003. ISSN 0003-4819.
- ↑ Klok, F.A.; Kruip, M.J.H.A.; van der Meer, N.J.M.; Arbous, M.S.; Gommers, D.A.M.P.J.; Kant, K.M.; Kaptein, F.H.J.; van Paassen, J.; Stals, M.A.M.; Huisman, M.V.; Endeman, H. (2020). "Incidence of thrombotic complications in critically ill ICU patients with COVID-19". Thrombosis Research. Elsevier BV. 191: 145–147. doi:10.1016/j.thromres.2020.04.013. ISSN 0049-3848.
- ↑ Bompard, Florian; Monnier, Hippolyte; Saab, Ines; Tordjman, Mickael; Abdoul, Hendy; Fournier, Laure; Sanchez, Olivier; Lorut, Christine; Chassagnon, Guillaume; Revel, Marie-pierre (2020-05-12). "Pulmonary embolism in patients with Covid-19 pneumonia". European Respiratory Journal. European Respiratory Society (ERS): 2001365. doi:10.1183/13993003.01365-2020. ISSN 0903-1936.
- ↑ Middeldorp, Saskia; Coppens, Michiel; van Haaps, Thijs F.; Foppen, Merijn; Vlaar, Alexander P.; Müller, Marcella C.A.; Bouman, Catherine C.S.; Beenen, Ludo F.M.; Kootte, Ruud S.; Heijmans, Jarom; Smits, Loek P.; Bonta, Peter I.; van Es, Nick (2020-05-05). "Incidence of venous thromboembolism in hospitalized patients with COVID‐19". Journal of Thrombosis and Haemostasis. Wiley. doi:10.1111/jth.14888. ISSN 1538-7933.
- ↑ Poyiadi, Neo; Cormier, Peter; Patel, Parth Y.; Hadied, Mohamad O.; Bhargava, Pallavi; Khanna, Kanika; Nadig, Jeffrey; Keimig, Thomas; Spizarny, David; Reeser, Nicholas; Klochko, Chad; Peterson, Edward L.; Song, Thomas (2020-05-14). "Acute Pulmonary Embolism and COVID-19". Radiology. Radiological Society of North America (RSNA): 201955. doi:10.1148/radiol.2020201955. ISSN 0033-8419.
- ↑ Teuwen, Laure-Anne; Geldhof, Vincent; Pasut, Alessandra; Carmeliet, Peter (2020-05-21). "COVID-19: the vasculature unleashed". Nature Reviews Immunology. Springer Science and Business Media LLC. doi:10.1038/s41577-020-0343-0. ISSN 1474-1733.
- ↑ Panigada, Mauro; Bottino, Nicola; Tagliabue, Paola; Grasselli, Giacomo; Novembrino, Cristina; Chantarangkul, Veena; Pesenti, Antonio; Peyvandi, Fora; Tripodi, Armando (2020-04-17). "Hypercoagulability of COVID‐19 patients in Intensive Care Unit. A Report of Thromboelastography Findings and other Parameters of Hemostasis". Journal of Thrombosis and Haemostasis. Wiley. doi:10.1111/jth.14850. ISSN 1538-7933.
- ↑ Stein, Paul D.; Beemath, Afzal; Matta, Fadi; Weg, John G.; Yusen, Roger D.; Hales, Charles A.; Hull, Russell D.; Leeper, Kenneth V.; Sostman, H. Dirk; Tapson, Victor F.; Buckley, John D.; Gottschalk, Alexander; Goodman, Lawrence R.; Wakefied, Thomas W.; Woodard, Pamela K. (2007). "Clinical Characteristics of Patients with Acute Pulmonary Embolism: Data from PIOPED II". The American Journal of Medicine. Elsevier BV. 120 (10): 871–879. doi:10.1016/j.amjmed.2007.03.024. ISSN 0002-9343.
- ↑ 9.0 9.1 "COVID-19 and Pulmonary Embolism". Hematology.org. 2020-05-18. Retrieved 2020-06-23.
- ↑ Bikdeli, Behnood; Madhavan, Mahesh V.; Jimenez, David; Chuich, Taylor; Dreyfus, Isaac; Driggin, Elissa; Nigoghossian, Caroline Der; Ageno, Walter; Madjid, Mohammad; Guo, Yutao; Tang, Liang V.; Hu, Yu; Giri, Jay; Cushman, Mary; Quéré, Isabelle; Dimakakos, Evangelos P.; Gibson, C. Michael; Lippi, Giuseppe; Favaloro, Emmanuel J.; Fareed, Jawed; Caprini, Joseph A.; Tafur, Alfonso J.; Burton, John R.; Francese, Dominic P.; Wang, Elizabeth Y.; Falanga, Anna; McLintock, Claire; Hunt, Beverley J.; Spyropoulos, Alex C.; Barnes, Geoffrey D.; Eikelboom, John W.; Weinberg, Ido; Schulman, Sam; Carrier, Marc; Piazza, Gregory; Beckman, Joshua A.; Steg, P. Gabriel; Stone, Gregg W.; Rosenkranz, Stephan; Goldhaber, Samuel Z.; Parikh, Sahil A.; Monreal, Manuel; Krumholz, Harlan M.; Konstantinides, Stavros V.; Weitz, Jeffrey I.; Lip, Gregory Y.H. (2020). "COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up". Journal of the American College of Cardiology. Elsevier BV. 75 (23): 2950–2973. doi:10.1016/j.jacc.2020.04.031. ISSN 0735-1097.