COVID-19-associated acute kidney injury: Difference between revisions
Jump to navigation
Jump to search
Gerald Chi- (talk | contribs) |
Gerald Chi- (talk | contribs) |
||
| Line 16: | Line 16: | ||
==Pathophysiology== | ==Pathophysiology== | ||
* Angiotensin-converting enzyme 2 ([[ACE2]]), which is a primary receptor for [[SARS-CoV-2]] entry into cells, mostly presents in renal tubular epithelial cells as well as lungs and heart.<ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref> | |||
* Despite kidney injury following [[COVID-19]] infection is less frequent than severe lung injury, [[ACE2]]: [[ACE]] ratio is higher in the kidneys compared to the respiratory system. (1:1 in the kidneys VS 1:20 in the respiratory system)<ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref> | |||
* After [[SARS-CoV-2]] enters through the nasal cavity, it may travel to the kidneys and enters the bloodstream leading to severe inflammatory response activation and [[cytokine]] storm. | |||
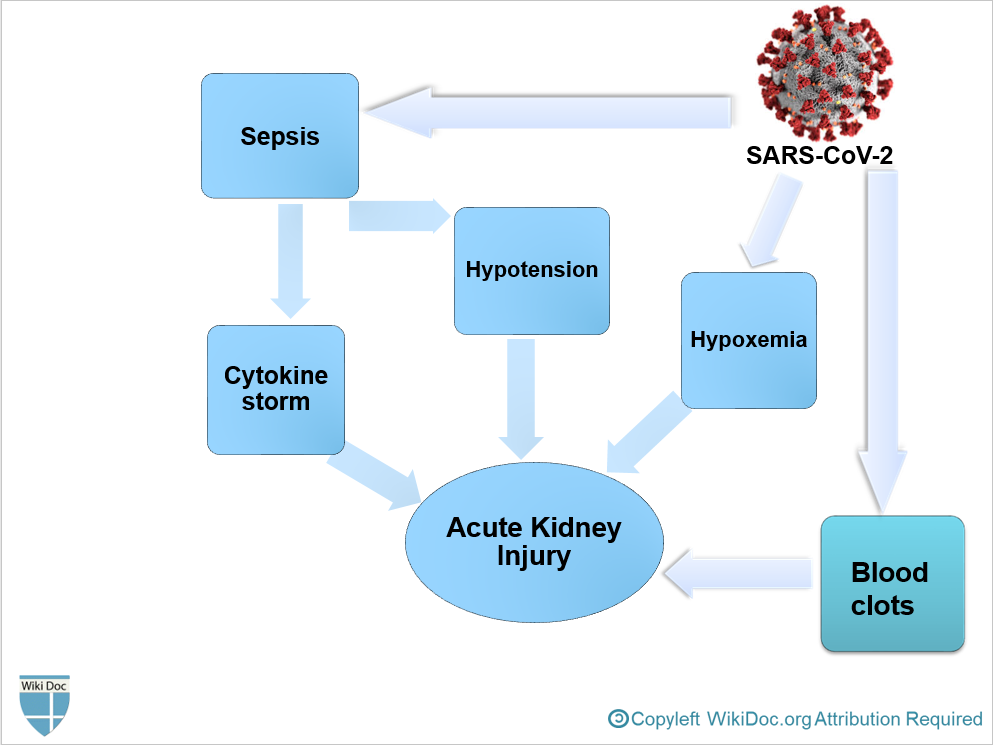
* It is thought that [[AKI]] following COVID-19 is the result of: <ref name="MalhaMueller2020">{{cite journal|last1=Malha|first1=Line|last2=Mueller|first2=Franco B.|last3=Pecker|first3=Mark S.|last4=Mann|first4=Samuel J.|last5=August|first5=Phyllis|last6=Feig|first6=Peter U.|title=COVID-19 and the Renin-Angiotensin System|journal=Kidney International Reports|volume=5|issue=5|year=2020|pages=563–565|issn=24680249|doi=10.1016/j.ekir.2020.03.024}}</ref> | |||
**[[Sepsis]] | |||
**[[Hypovolemia]] and [[Hypotension]] | |||
**[[Hypoxemia]] | |||
**Blood clots formation, leading to impaired blood flow in the renal arterioles. | |||
[[File:AKI physiopathology COVID.PNG|600px|center]] | |||
==Differentiating COVID-19-Associated Acute Kidney Injury From Other Diseases== | ==Differentiating COVID-19-Associated Acute Kidney Injury From Other Diseases== | ||
Revision as of 17:05, 25 June 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sogand Goudarzi, MD [2], Nasrin Nikravangolsefid, MD-MPH [3]
Synonyms and keywords: COVID-19-associated AKI
Overview
COVID-19 can involve many organs leading to organ failure, one of which is kidneys that manifest with mild proteinuria to advanced acute kidney injury (AKI).
Historical Perspective
- Early reports from China revealed that COVID-19 rarely involves the kidneys, as acute renal failure was not seen among COVID-19 hospitalized patients and mild BUN or creatinine rise [10.8%] and mild proteinuria [7.2%] occurred. [1]
- However, recent study found 75.4% of hospitalized patients with COVID-19 pneumonia developed hematuria, proteinuria, and AKI. But, these findings are not significantly different from other critical diseases.[2]
Classification
Pathophysiology
- Angiotensin-converting enzyme 2 (ACE2), which is a primary receptor for SARS-CoV-2 entry into cells, mostly presents in renal tubular epithelial cells as well as lungs and heart.[3]
- Despite kidney injury following COVID-19 infection is less frequent than severe lung injury, ACE2: ACE ratio is higher in the kidneys compared to the respiratory system. (1:1 in the kidneys VS 1:20 in the respiratory system)[3]
- After SARS-CoV-2 enters through the nasal cavity, it may travel to the kidneys and enters the bloodstream leading to severe inflammatory response activation and cytokine storm.
- It is thought that AKI following COVID-19 is the result of: [3]
- Sepsis
- Hypovolemia and Hypotension
- Hypoxemia
- Blood clots formation, leading to impaired blood flow in the renal arterioles.
Differentiating COVID-19-Associated Acute Kidney Injury From Other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications, and Prognosis
Diagnosis
Symptoms
Family History
Physical Examination
Appearance of the Patient
Vital Signs
Skin
Head
Eyes
Ear
Nose
Throat
Heart
Lungs
Abdomen
Extremities
Neurologic
Other
Laboratory Findings
Biomarker Studies
CT
MRI
Ultrasound
Treatment
Pharmacotherapy
Acute Pharmacotherapies
Chronic Pharmacotherapies
Surgery and Device Based Therapy
Indications for Surgery
Pre-Operative Assessment
Post-Operative Management
Primary Prevention
Genetic Counseling
References
- ↑ Wang, Luwen; Li, Xun; Chen, Hui; Yan, Shaonan; Li, Dong; Li, Yan; Gong, Zuojiong (2020). "Coronavirus Disease 19 Infection Does Not Result in Acute Kidney Injury: An Analysis of 116 Hospitalized Patients from Wuhan, China". American Journal of Nephrology. 51 (5): 343–348. doi:10.1159/000507471. ISSN 0250-8095.
- ↑ Pei, Guangchang; Zhang, Zhiguo; Peng, Jing; Liu, Liu; Zhang, Chunxiu; Yu, Chong; Ma, Zufu; Huang, Yi; Liu, Wei; Yao, Ying; Zeng, Rui; Xu, Gang (2020). "Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia". Journal of the American Society of Nephrology. 31 (6): 1157–1165. doi:10.1681/ASN.2020030276. ISSN 1046-6673.
- ↑ 3.0 3.1 3.2 Malha, Line; Mueller, Franco B.; Pecker, Mark S.; Mann, Samuel J.; August, Phyllis; Feig, Peter U. (2020). "COVID-19 and the Renin-Angiotensin System". Kidney International Reports. 5 (5): 563–565. doi:10.1016/j.ekir.2020.03.024. ISSN 2468-0249.