Brain abscess: Difference between revisions
| Line 27: | Line 27: | ||
==Treatment== | ==Treatment== | ||
[[Brain abscess medical therapy|Medical therapy]] | [[Brain abscess surgery|Surgical options]] | [[Brain abscess primary prevention|Primary prevention]] | [[Brain abscess secondary prevention|Secondary prevention]] | [[Brain abscess cost-effectiveness of therapy|Financial costs]] | [[Brain abscess future or investigational therapies|Future therapies]] | [[Brain abscess medical therapy|Medical therapy]] | [[Brain abscess surgery|Surgical options]] | [[Brain abscess primary prevention|Primary prevention]] | [[Brain abscess secondary prevention|Secondary prevention]] | [[Brain abscess cost-effectiveness of therapy|Financial costs]] | [[Brain abscess future or investigational therapies|Future therapies]] | ||
== Diagnosis == | == Diagnosis == | ||
The diagnosis is established by a [[computed tomography]] (CT) (with contrast) examination. At the initial phase of the inflammation (which is referred to as [[cerebrit]]is), the immature lesion does not have a capsule and it may be difficult to distinguish it from other space-occupying lesions or infarcts of the brain. Within 4-5 days the inflammation and the concomitant dead brain tissue are surrounded with a capsule, which gives the lesion the famous ring-enhancing appearance on CT examination with contrast (since intravenously applied contrast material can not pass through the capsule, it is collected around the lesion and looks as a ring surrounding the relatively dark lesion). [[Lumbar puncture]] procedure, which is performed in many infectious disorders of the central nervous system is contraindicated in this condition (as it is in all space-occupying lesions of the brain) because removing a certain portion of the [[Cerebral Spinal Fluid|cerebrospinal fluid]] may alter the concrete intracranial pressure balances and cause a part of the brain tissue to move out of the skull ([[brain herniation]]). | The diagnosis is established by a [[computed tomography]] (CT) (with contrast) examination. At the initial phase of the inflammation (which is referred to as [[cerebrit]]is), the immature lesion does not have a capsule and it may be difficult to distinguish it from other space-occupying lesions or infarcts of the brain. Within 4-5 days the inflammation and the concomitant dead brain tissue are surrounded with a capsule, which gives the lesion the famous ring-enhancing appearance on CT examination with contrast (since intravenously applied contrast material can not pass through the capsule, it is collected around the lesion and looks as a ring surrounding the relatively dark lesion). [[Lumbar puncture]] procedure, which is performed in many infectious disorders of the central nervous system is contraindicated in this condition (as it is in all space-occupying lesions of the brain) because removing a certain portion of the [[Cerebral Spinal Fluid|cerebrospinal fluid]] may alter the concrete intracranial pressure balances and cause a part of the brain tissue to move out of the skull ([[brain herniation]]). | ||
Revision as of 20:07, 23 January 2012
For patient information, click here
|
Brain abscess Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Brain abscess On the Web |
|
American Roentgen Ray Society Images of Brain abscess |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Historical Perspective
Pathophysiology
Epidemiology & Demographics
Risk Factors
Screening
Causes
Differentiating Brain abscess
Complications & Prognosis
Diagnosis
History and Symptoms | Physical Examination | Laboratory tests | Electrocardiogram | X Rays | CT | MRI Echocardiography or Ultrasound | Other images | Alternative diagnostics
Treatment
Medical therapy | Surgical options | Primary prevention | Secondary prevention | Financial costs | Future therapies
Diagnosis
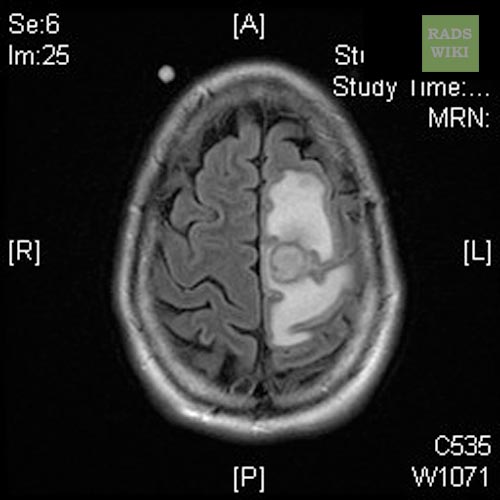
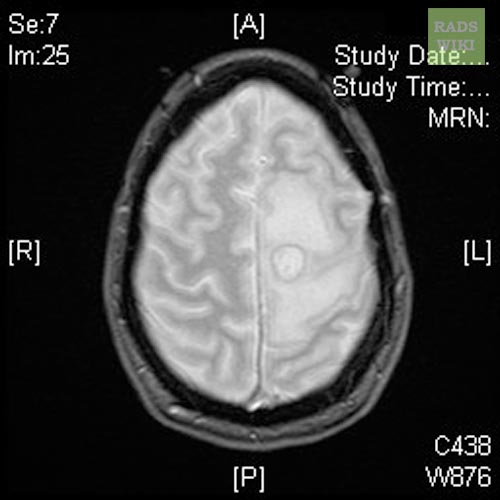
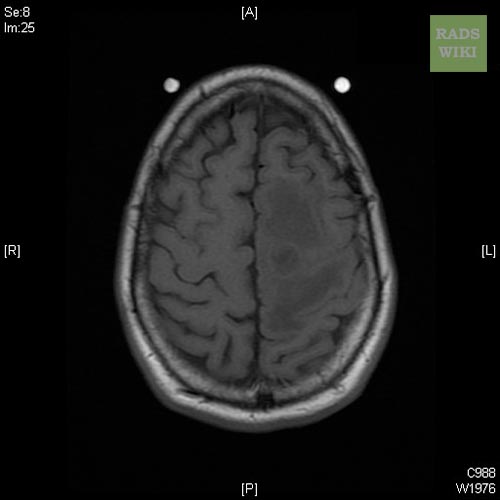
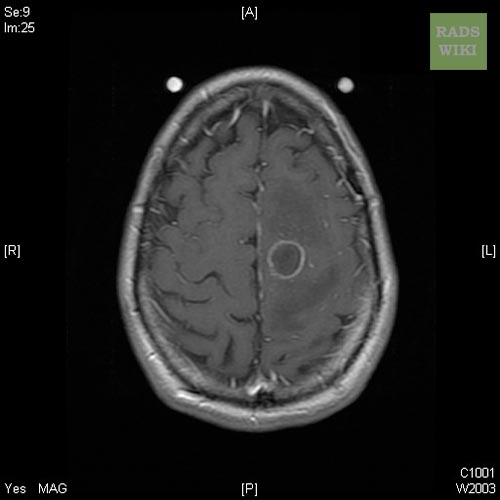
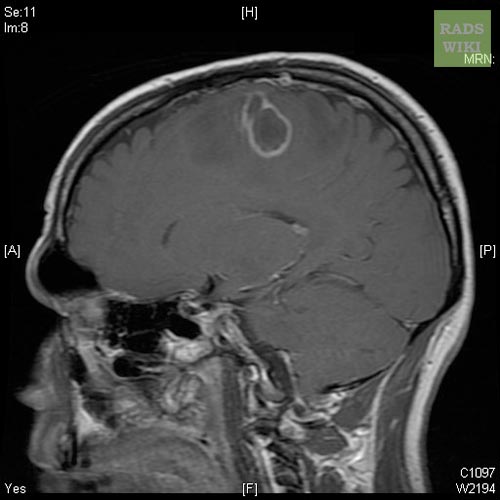
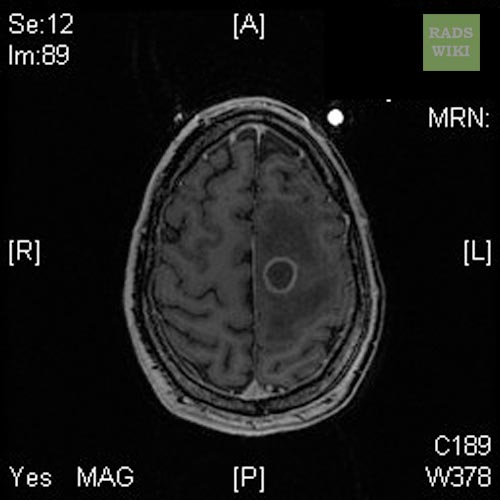
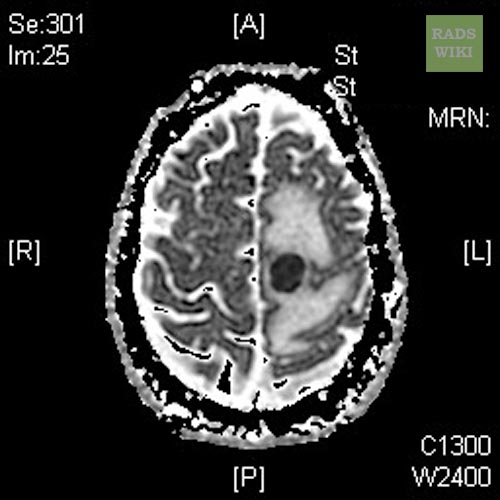
The diagnosis is established by a computed tomography (CT) (with contrast) examination. At the initial phase of the inflammation (which is referred to as cerebritis), the immature lesion does not have a capsule and it may be difficult to distinguish it from other space-occupying lesions or infarcts of the brain. Within 4-5 days the inflammation and the concomitant dead brain tissue are surrounded with a capsule, which gives the lesion the famous ring-enhancing appearance on CT examination with contrast (since intravenously applied contrast material can not pass through the capsule, it is collected around the lesion and looks as a ring surrounding the relatively dark lesion). Lumbar puncture procedure, which is performed in many infectious disorders of the central nervous system is contraindicated in this condition (as it is in all space-occupying lesions of the brain) because removing a certain portion of the cerebrospinal fluid may alter the concrete intracranial pressure balances and cause a part of the brain tissue to move out of the skull (brain herniation).
Ring enhancement may also be observed in cerebral hemorrhages (bleeding) and some brain tumors. However, in the presence of the rapidly progressive course with fever, focal neurologic findings (hemiparesis, aphasia etc) and signs of increased intracranial pressure, the most likely diagnosis should be the brain abscess.
- There are basically no confirmatory blood studies.
- Patients usually have a moderate leukocytosis (< 20k), yet up to 40% can have a normal WBC count.
- The ESR is usually elevated in the 40 – 50 range, but again, can also be normal.
- Blood cultures are usually negative, but should be obtained just in case they are positive.
- The LP is usually not helpful, and the risks are thought to outweigh the benefits.
- If done, the protein and cell counts are usually elevated and CSF Cx are usually negative.
- Obtaining tissue is obviously the gold standard and will demonstrate the pathogen in close to 100% of cases.
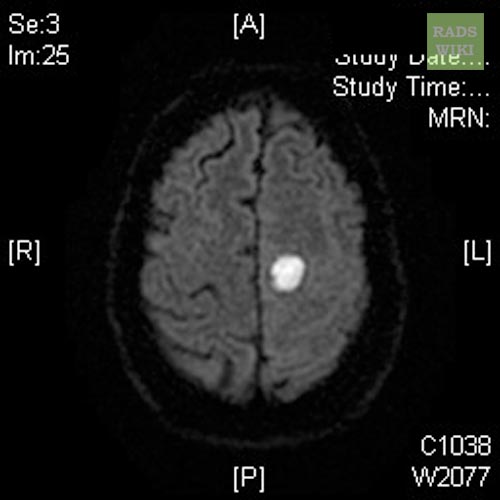
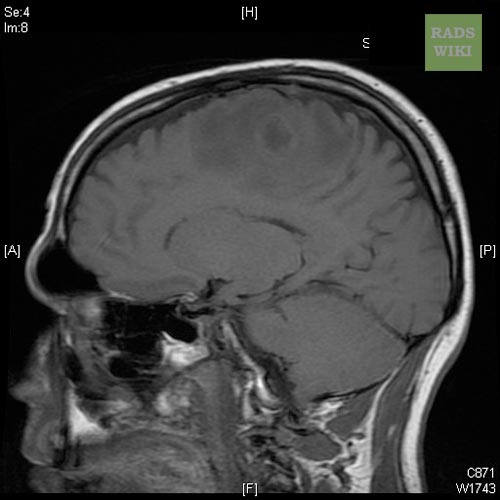
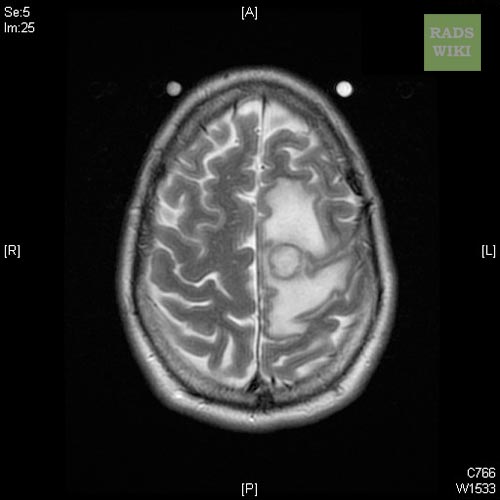
MRI
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
Differential Diagnosis
- Some studies suggest that indium scans can help differentiate abscess from CA, and thallium SPECT scans can distinguish CNS toxo from lymphoma.
- A CT scan with contrast will show a ring-enhancing mass that surrounds an area of hypodensity (necrosis or edema).
- The big differential is metastatic tumor: abscesses are often located in watershed regions, and tumors often enhance diffusely with contrast.
- Despite these differences, the true Dx is sometimes not made until biopsy.
- MRI is generally thought to be the imaging modality of choice and can more accurately stage the abscess and gauge the response to therapy.
Treatment
Treatment is generally a team approach and most reliably depends on obtaining tissue via a stereotactic needle Bx. Although randomized, controlled trials have not been done, the consensus is that abscesses > 3cm should be drained (if accessible).
The treatment includes lowering the increased intracranial pressure and starting intravenous antibiotics (and meanwhile identifying the causative organism mainly by blood culture studies).
Surgical drainage of the abscess remains part of the standard management of bacterial brain abscesses. The location and treatment of the primary lesion also crucial, as is the removal of any foreign material (bone, dirt, bullets, and so forth).
There are a few exceptions to this rule: Haemophilus influenzae meningitis is often associated with subdural effusions that are mistaken for subdural empyemas. These effusions resolve with antibiotics and require no surgical treatment. Tuberculosis can produce brain abscesses that look identical to bacterial abscesses on CT imaging and surgical drainage or aspiration is often necessary to make the diagnosis, but once the diagnosis is made no further surgical intervention is necessary.
- Antibiotics: Brain abscesses are usually polymicrobial, with the most common bugs being microaerophilic streptococci (viridans) and anaerobic bacteria (bacteroides, anaerobic strep and fusobacterium).
- S. aureus, and enterobacteriacae are also seen.
- Bugs associated with trauma include S. aureus and clostridium sp.
- Empiric Rx usually starts with high-dose PCN (10 – 20 million units / d), metronidazole, +/- a 3rd gen cephalosporin.
- Even if the abscess is associated with a dental procedure and other organisms are considered (actinomyces sp.) they generally respond to the above Rx.
- If extending from an otitis, empiric Rx should also cover pseudomonas and enterobacteriacaea.
- If hematogenously spread, coverage depends on the original bug.
- The penetration of abx into an abscess does not necessarily equate with their penetration into the CSF (the blood-brain barrier is not the same as the blood-CSF barrier).
- Drugs like vancomycin, which have poor CSF levels (<10% of serum) have been shown to have good abscess levels (90% of serum).
- Most patients are treated parenterally for at least 8w.
- Some authors also recommend an additional 2 – 3 month course of oral abx to clear up any ‘residual’ infection and to prevent relapses.
- One study actually suggests that, when combined with surgical excision, 3w may be adequate.
- Other studies have reported good outcomes with abx alone in patients with small lesions (<2cm), in well vascularized areas (cortex), who were poor surgical candidates.
- There have not been any studies reporting benefit from intra-thecal or intra-abscess abx.
- There seems to be consensus on obtaining q 2 – 4w f/u CT/MRI scans to document resolution.
Surgery
Surgery has evolved dramatically over the last few decades.
- Once requiring open craniotomy and drainage / excision, most procedures are currently minimally invasive, closed, and performed under local anesthesia with conscious sedation and CT guidance.
- CT guidance is accurate to within 4 – 5mm.
- Stereotactic drainage can also be used if necessary, and is accurate to within 1 – 2mm.
- Open craniotomy with complete excision is usually reserved for patients with multiloculated abscesses or in cases due to more resistant pathogens (e.g. fungi and nocardia).
Adjuvants
- Although steroids have not been studies in well-designed trials, many authors use them in patients with elevated ICP.
- Some animal studies suggest interference with granulation tissue formation and bacterial clearance.
- Anticonvulsants are recommended prophylactically for the 1st 3m, though the data supporting this is lacking.
Prognosis
Once an almost always fatal disease before the CT era. If the abscess is treated before the person goes into a coma then the death rate has been estimated from 5% to 20%.
Early treatment and the patients overall health has an effect on prognosis. Other factors include: antibiotic resistance or the abscess location. An abscess deep within the brain is more difficult to treat than others.
In general
- Mortality is currently quoted to range from 0 – 24%.
- Poor prognostic indicators include:
- Intraventricular rupture:
- 80% mortality rate, often treated with open drainage and debridement f/b ventriculostomy catheter for drainage and intrathecal abx
- Mental status and neurologic function at time of Dx:
- The most common sequellae is seizures, which develop in 35 – 70% of patients.
References
Additional Resources
Mathisen, G.E., Johnson, J.P., Brain abscess, Clin Infectious Disease 1997; 25: 763-781.