Brain abscess: Difference between revisions
No edit summary |
|||
| Line 5: | Line 5: | ||
==[[Brain abscess overview|Overview]]== | ==[[Brain abscess overview|Overview]]== | ||
== History == | == History == | ||
Revision as of 19:58, 23 January 2012
For patient information, click here
|
Brain abscess Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Brain abscess On the Web |
|
American Roentgen Ray Society Images of Brain abscess |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
History
Prior to the 1800s, brain abscesses were almost uniformly fatal, and were rarely diagnosed prior to autopsy. Macewan was one of the 1st neurosurgeons who showed that these patients could actually be cured via surgical drainage. In the post WWII / antibiotic era, the mortality from brain abscesses really started to drop, and with the advent of the CT in 1974, earlier diagnosis and Rx was finally possible.
Epidemiology and Demographics
There has been a remarkable shift in the epidemiology of brain abscesses over the past several years. Traditionally, and still the case in underdeveloped countries, most brain abscesses are due to un / under-treated otitis and sinusitis. More recently, especially in the U.S., more cases are being seen in immunocompromised patients. Recent stats:
- Accounts for ~ 1 in 10,000 hospital admissions
- Seen in 0.18 – 1.3 % of autopsies.
- M:F 1.5 – 2:1.
- Bimodal age distribution: 25% of cases are seen in children < 15yo (mean 4 – 7yo) with another peak at 30 – 50 yo.
Pathophysiology
Brain abscesses are usually polymicrobial in nature.
The most common organism recovered from cultures is the bacterium Streptococcus. However, a wide variety of other bacteria (Proteus, Pseudomonas, Pneumococcus, Meningococcus, Haemophilus), fungi and parasites may also cause the disease. Fungi and parasites are especially associated with immunocompromised patients. Organisms that are most frequently-associated with brain abscess in patients with AIDS are Mycobacterium tuberculosis, Toxoplasma gondii and Cryptococcus neoformans, though in infection with the latter organism, symptoms of meningitis generally predominate.
Bacterial abscesses rarely (if ever) arise de novo within the brain. There is almost always a primary lesion elsewhere in the body that must be sought assiduously, because failure to treat the primary lesion will result in relapse. In cases of trauma, for example in compound skull fractures where fragments of bone are pushed into the substance of the brain, the cause of the abscess is obvious. Similarly, bullets and other foreign bodies may become sources of infection if left in place. The location of the primary lesion may be suggested by the location of the abscess: infections of the middle ear result in lesions in the middle and posterior cranial fossae;[1] congenital heart disease with right-to-left shunts often result in abscesses in the distribution of the middle cerebral artery[2][3]; and infection of the frontal and ethmoid sinuses usually results in collection in the subdural sinuses.
Brain abscesses usually start as a focal area of cerebritis that eventually develops into a collection of puss, surrounded by a well-vascularized capsule.
- In general, the brain is relatively resistant to infection due to the presence of the abundant blood supply, and the relatively impermeable blood-brain barrier.
- Although underlying pathology (tumor, blood etc.) can sometimes be a nidus for infection, the majority of cases occur in a previously ‘healthy’ brain.
- Experimental models have identified four stages for abscess formation:
- Early cerebritis (days 1 – 3): focal inflammation and edema.
- Late cerebritis (d 4 – 9): development of a necrotic center.
- Early capsular (d 10 – 14): formation of a well-vascularized, ring-enhancing capsule with peripheral gliosis and / or fibrosis.
- Late capsular: (after 2w): formation of a well-formed fibrous capsule.
- Approximately 47% of cases arise from a contiguous infection, most commonly in the middle ear, the paranasal sinuses and teeth.
- ~ 25% result from hematogenous seeding from an extracranial infection.
- Penetrating trauma accounts for ~ 10% of cases.
- 20 – 30% of cases are idiopathic, and no obvious focus can be identified.
- The location of the abscess obviously depends on the source of infection, as does the specific microbial flora.
Clinical Presentation
The symptoms of brain abscess are caused by a combination of increased intracranial pressure due to a space-occupying lesion (headache, vomiting, confusion, coma), infection (fever, fatigue etc.) and focal neurologic brain tissue damage (hemiparesis, aphasia etc.).
The most frequent presenting symptoms are headache, drowsiness, confusion, seizures, hemiparesis or speech difficulties together with fever with a rapidly progressive course.
The symptoms and findings depend largely on the specific location of the abscess in the brain. An abscess in the cerebellum, for instance, may cause additional complaints as a result of brain stem compression and hydrocephalus.
Neurological examination may reveal a stiff neck in occasional cases (erroneously suggesting meningitis). The famous triad of fever, headache and focal neurologic findings are highly suggestive of brain abscess but are observed only in a minority of the patients.
As a summary the presenting signs and symptoms relate to the size and location of the abscess, the virulence of the bug and any underlying comorbidities.
- Headache is the most common complaint, seen > 75% of patients.
- There are no specific descriptors of an abscess headache accounting for one of the factors that often delays the diagnosis.
- The BA is usually not severe, unless the abscess ruptures into a ventricle, at which time meningismus and death often develop as well.
- The classic triad of BA, fever and a focal neurologic deficit are seen in < 50% of cases.
- Signs of increased ICP (N/V, lethargy etc.) can be seen in up to 50% of patients, and is usually an indication for immediate intervention.
- Papilledema, however, is seen in < 25% of cases.
- Fever is present in 40 – 50% of cases, and hence its absence should not be used to exclude the Dx.
- Approximately 30 - 50% of patients will have focal neuro deficits (most commonly hemiparesis).
- 25% of patients present with new-onset seizures.
Diagnosis
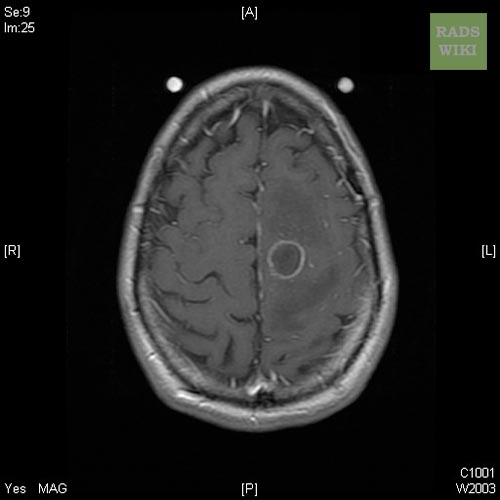
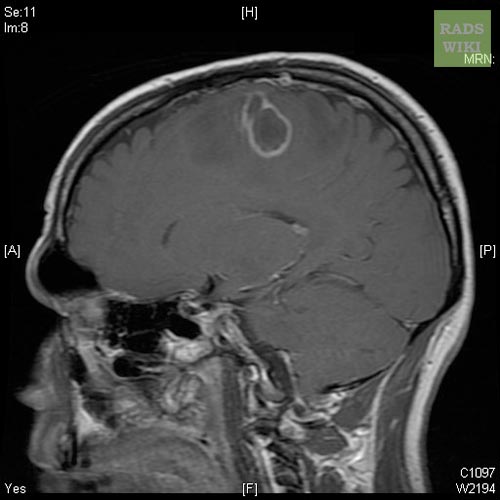
The diagnosis is established by a computed tomography (CT) (with contrast) examination. At the initial phase of the inflammation (which is referred to as cerebritis), the immature lesion does not have a capsule and it may be difficult to distinguish it from other space-occupying lesions or infarcts of the brain. Within 4-5 days the inflammation and the concomitant dead brain tissue are surrounded with a capsule, which gives the lesion the famous ring-enhancing appearance on CT examination with contrast (since intravenously applied contrast material can not pass through the capsule, it is collected around the lesion and looks as a ring surrounding the relatively dark lesion). Lumbar puncture procedure, which is performed in many infectious disorders of the central nervous system is contraindicated in this condition (as it is in all space-occupying lesions of the brain) because removing a certain portion of the cerebrospinal fluid may alter the concrete intracranial pressure balances and cause a part of the brain tissue to move out of the skull (brain herniation).
Ring enhancement may also be observed in cerebral hemorrhages (bleeding) and some brain tumors. However, in the presence of the rapidly progressive course with fever, focal neurologic findings (hemiparesis, aphasia etc) and signs of increased intracranial pressure, the most likely diagnosis should be the brain abscess.
- There are basically no confirmatory blood studies.
- Patients usually have a moderate leukocytosis (< 20k), yet up to 40% can have a normal WBC count.
- The ESR is usually elevated in the 40 – 50 range, but again, can also be normal.
- Blood cultures are usually negative, but should be obtained just in case they are positive.
- The LP is usually not helpful, and the risks are thought to outweigh the benefits.
- If done, the protein and cell counts are usually elevated and CSF Cx are usually negative.
- Obtaining tissue is obviously the gold standard and will demonstrate the pathogen in close to 100% of cases.
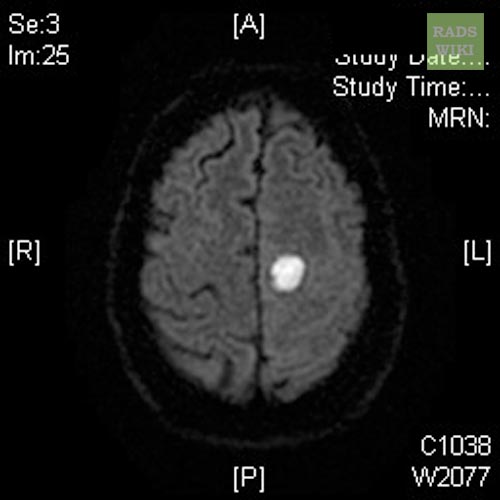
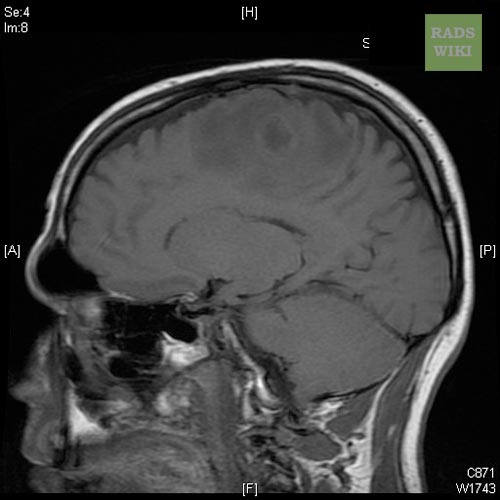
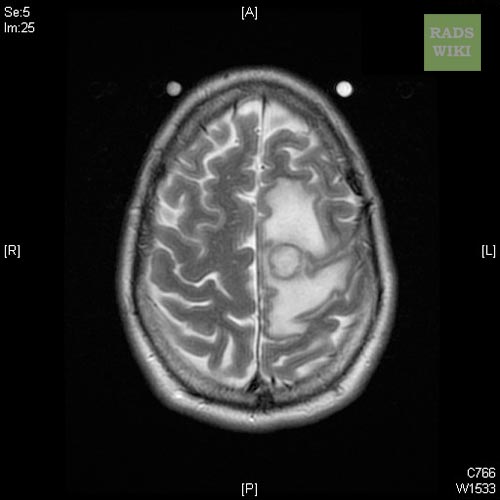
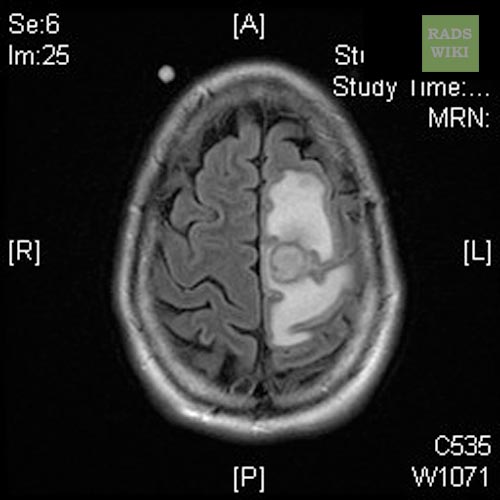
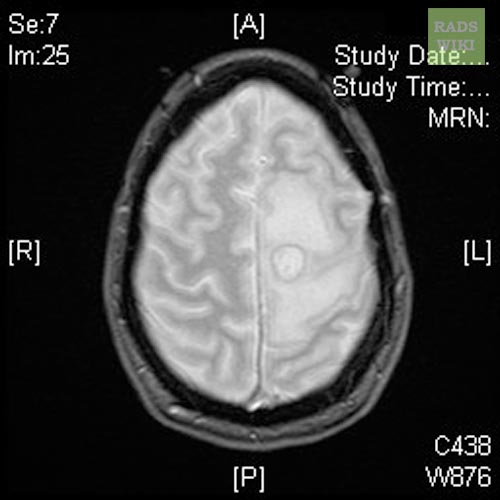
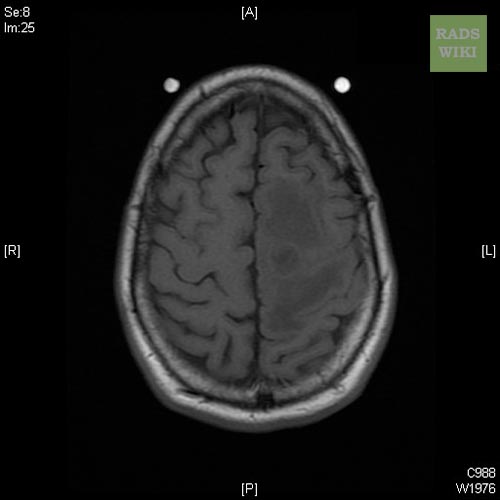
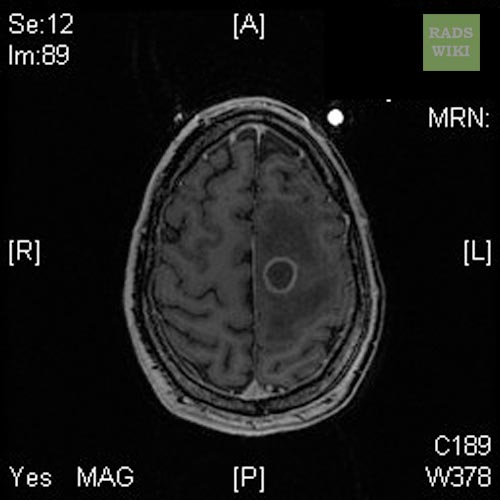
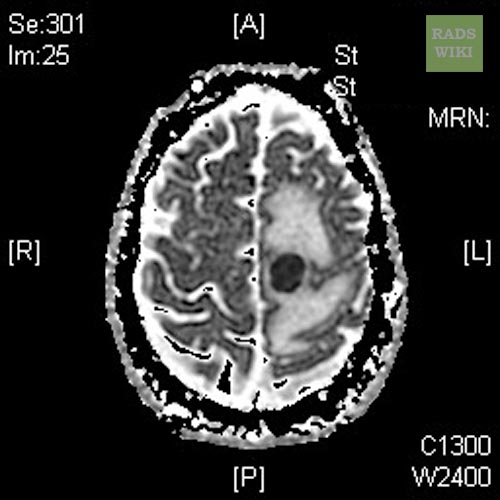
MRI
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
-
Brain abscess
Differential Diagnosis
- Some studies suggest that indium scans can help differentiate abscess from CA, and thallium SPECT scans can distinguish CNS toxo from lymphoma.
- A CT scan with contrast will show a ring-enhancing mass that surrounds an area of hypodensity (necrosis or edema).
- The big differential is metastatic tumor: abscesses are often located in watershed regions, and tumors often enhance diffusely with contrast.
- Despite these differences, the true Dx is sometimes not made until biopsy.
- MRI is generally thought to be the imaging modality of choice and can more accurately stage the abscess and gauge the response to therapy.
Treatment
Treatment is generally a team approach and most reliably depends on obtaining tissue via a stereotactic needle Bx. Although randomized, controlled trials have not been done, the consensus is that abscesses > 3cm should be drained (if accessible).
The treatment includes lowering the increased intracranial pressure and starting intravenous antibiotics (and meanwhile identifying the causative organism mainly by blood culture studies).
Surgical drainage of the abscess remains part of the standard management of bacterial brain abscesses. The location and treatment of the primary lesion also crucial, as is the removal of any foreign material (bone, dirt, bullets, and so forth).
There are a few exceptions to this rule: Haemophilus influenzae meningitis is often associated with subdural effusions that are mistaken for subdural empyemas. These effusions resolve with antibiotics and require no surgical treatment. Tuberculosis can produce brain abscesses that look identical to bacterial abscesses on CT imaging and surgical drainage or aspiration is often necessary to make the diagnosis, but once the diagnosis is made no further surgical intervention is necessary.
- Antibiotics: Brain abscesses are usually polymicrobial, with the most common bugs being microaerophilic streptococci (viridans) and anaerobic bacteria (bacteroides, anaerobic strep and fusobacterium).
- S. aureus, and enterobacteriacae are also seen.
- Bugs associated with trauma include S. aureus and clostridium sp.
- Empiric Rx usually starts with high-dose PCN (10 – 20 million units / d), metronidazole, +/- a 3rd gen cephalosporin.
- Even if the abscess is associated with a dental procedure and other organisms are considered (actinomyces sp.) they generally respond to the above Rx.
- If extending from an otitis, empiric Rx should also cover pseudomonas and enterobacteriacaea.
- If hematogenously spread, coverage depends on the original bug.
- The penetration of abx into an abscess does not necessarily equate with their penetration into the CSF (the blood-brain barrier is not the same as the blood-CSF barrier).
- Drugs like vancomycin, which have poor CSF levels (<10% of serum) have been shown to have good abscess levels (90% of serum).
- Most patients are treated parenterally for at least 8w.
- Some authors also recommend an additional 2 – 3 month course of oral abx to clear up any ‘residual’ infection and to prevent relapses.
- One study actually suggests that, when combined with surgical excision, 3w may be adequate.
- Other studies have reported good outcomes with abx alone in patients with small lesions (<2cm), in well vascularized areas (cortex), who were poor surgical candidates.
- There have not been any studies reporting benefit from intra-thecal or intra-abscess abx.
- There seems to be consensus on obtaining q 2 – 4w f/u CT/MRI scans to document resolution.
Surgery
Surgery has evolved dramatically over the last few decades.
- Once requiring open craniotomy and drainage / excision, most procedures are currently minimally invasive, closed, and performed under local anesthesia with conscious sedation and CT guidance.
- CT guidance is accurate to within 4 – 5mm.
- Stereotactic drainage can also be used if necessary, and is accurate to within 1 – 2mm.
- Open craniotomy with complete excision is usually reserved for patients with multiloculated abscesses or in cases due to more resistant pathogens (e.g. fungi and nocardia).
Adjuvants
- Although steroids have not been studies in well-designed trials, many authors use them in patients with elevated ICP.
- Some animal studies suggest interference with granulation tissue formation and bacterial clearance.
- Anticonvulsants are recommended prophylactically for the 1st 3m, though the data supporting this is lacking.
Prognosis
Once an almost always fatal disease before the CT era. If the abscess is treated before the person goes into a coma then the death rate has been estimated from 5% to 20%.
Early treatment and the patients overall health has an effect on prognosis. Other factors include: antibiotic resistance or the abscess location. An abscess deep within the brain is more difficult to treat than others.
In general
- Mortality is currently quoted to range from 0 – 24%.
- Poor prognostic indicators include:
- Intraventricular rupture:
- 80% mortality rate, often treated with open drainage and debridement f/b ventriculostomy catheter for drainage and intrathecal abx
- Mental status and neurologic function at time of Dx:
- The most common sequellae is seizures, which develop in 35 – 70% of patients.
References
- ↑ Macewan W (1893). Pyogenic Infective Diseases of the Brain and Spinal Cord. Glasgow: James Maclehose and Sons.
- ↑ Ingraham FD, Matson DD (1954). Neurosurgery of Infancy andChildhood. Springfield, Ill: Charles C Thomas. Unknown parameter
|paes=ignored (help) - ↑ Raimondi AJ, Matsumoto S, Miller RA (1965). "Brain abscess in children with congenital heart disease". J Neurosurg. 23: 588&ndash, 95.
Additional Resources
Mathisen, G.E., Johnson, J.P., Brain abscess, Clin Infectious Disease 1997; 25: 763-781.