Bowel obstruction
Template:DiseaseDisorder infobox For patient information click here
|
Bowel obstruction Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Bowel obstruction On the Web |
|
American Roentgen Ray Society Images of Bowel obstruction |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Signs, symptoms and causes
Depending on the level of obstruction, bowel obstruction can present with abdominal pain, abdominal distension, vomiting, fecal vomiting, and constipation.
Obstruction may be due to causes within the bowel lumen, within the wall of the bowel, or external to the bowel (such as compression, entrapment or volvulus).
Bowel obstruction may be complicated by dehydration and electrolyte abnormalities due to vomiting; respiratory compromise from pressure on the diaphragm by a distended abdomen, or aspiration of vomitus; bowel ischaemia or perforation from prolonged distension or pressure from a foreign body.
In small bowel obstruction the pain tends to be colicky (cramping and intermittent) in nature, with spasms lasting a few minutes. The pain tends to be central and mid-abdominal. Vomiting occurs before constipation.
In large bowel obstruction the pain is felt lower in the abdomen and the spasms last longer. Constipation occurs earlier and vomiting may be less prominent. Proximal obstruction of the large bowel may present as small bowel obstruction.
Diagnosis
The main diagnostic tools are blood tests, X-rays of the abdomen, CT scanning and/or ultrasound. If a mass is identified, biopsy may determine the nature of the mass.
-
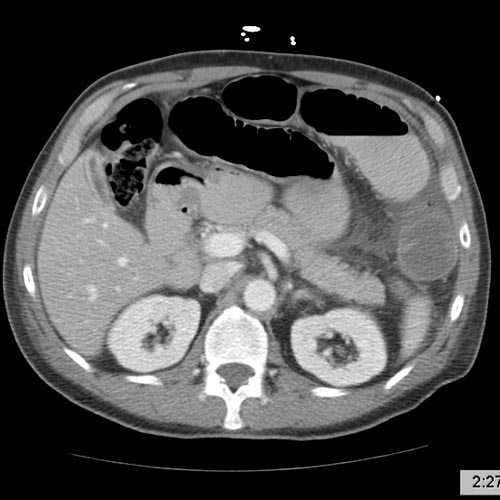
Small bowel obstruction Image courtesy of RadsWiki and copylefted
-
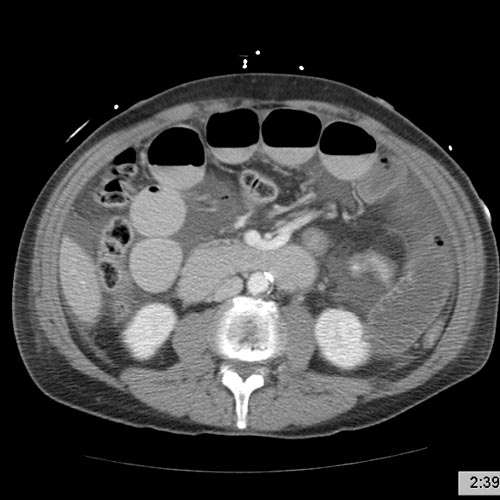
Small bowel obstruction Image courtesy of RadsWiki and copylefted
-
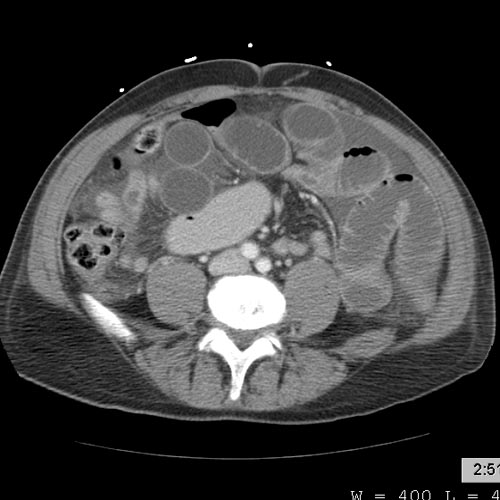
Small bowel obstruction Image courtesy of RadsWiki and copylefted
-
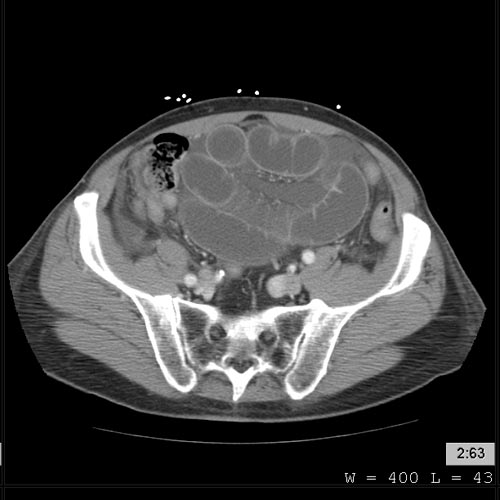
Small bowel obstruction Image courtesy of RadsWiki and copylefted
-
Small bowel obstruction Image courtesy of RadsWiki and copylefted
Radiological signs of bowel obstruction include bowel distension and the presence of multiple (more than six) gas-fluid levels on supine and erect abdominal radiographs.
Contrast enema or small bowel series or CT scan can be used to define the level of obstruction, whether the obstruction is partial or complete, and to help define the cause of the obstruction.
According to a meta-analysis of prospective studies by the Cochrane Collaboration, the appearance of water-soluble contrast in the cecum on an abdominal radiograph within 24 hours of oral administration predicts resolution of an adhesive small bowel obstruction with a pooled sensitivity of 96% and specificity of 96%. PMID 15674958
Colonoscopy, small bowel investigation with ingested camera or push endoscopy, and laparoscopy are other diagnostic options.
Treatment
Some causes of bowel obstruction may resolve spontaneously; many require operative treatment.
In adults, frequently the surgical intervention and the treatment of the causative lesion are required. In malignant large bowel obstruction, endoscopically placed self-expanding metal stents may be used to temporarily relieve the obstruction as a bridge to surgery, or as palliation.
Small bowel obstruction
In the management of small bowel obstructions it is often said that "[n]ever let the sun rise or set on small-bowel obstruction"[1] because they are sometimes fatal if treatment is delayed.
Treatment for a small bowel obstruction is both non-surgical (conservative) and surgical.
Conservative treatment involves insertion of a nasogastric tube, correction of dehydration and electrolyte abnormalities. Opioid pain relievers may be used for patients with severe pain. Antiemetics may be administered if the patient is vomiting. Adhesive obstructions often settle without surgery. If obstruction is complete a surgery is required.
Small bowel obstruction caused by Crohn's disease, peritoneal carcinomatosis, sclerosing peritonitis, radiation enteritis and postpartum bowel obstruction are typically treated conservatively, i.e. without surgery. Conversely, a small bowel obstruction in a "virgin abdomen" (an abdomen that has not seen an operation) is almost never treated conservatively.
Bowel obstruction in children
Fetal and neonatal bowel obstructions are often caused by an intestinal atresia where there is a narrowing or absence of a part of the intestine. These atresias are often discovered before birth via a sonogram and treated with using laparotomy after birth. If the area affected is small then the surgeon may be able to remove the damaged portion and join the intestine back together. In instantances where the narrowing is longer, or the area is damaged and cannot be used for a period of time, a temporary stoma may be placed.
Pathological Findings
-
Intestine: Ileus Newborn Cause Unknown: Gross natural color opened body with protruding grossly dilated loops of bowel there was no evidence of necrotizing enteritis
-
Intestine: Ileus Newborn Cause Unknown: Gross natural color close-up view of distended gut loops