Astrocytoma MRI: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
|||
| Line 74: | Line 74: | ||
:* T2: usually hyperintense | :* T2: usually hyperintense | ||
:* T1 C+ (Gd): common and is usually in the solid component, but can be also peripheric | :* T1 C+ (Gd): common and is usually in the solid component, but can be also peripheric | ||
===Subependymal Giant Cell Astrocytoma<ref name=Radiopaedia052015>{{cite web | title = Subependymal giant cell astrocytoma [Dr Bruno Di Muzio and Dr Jeremy Jones]| url | |||
===Subependymal Giant Cell Astrocytoma<ref name=Radiopaedia052015>{{cite web | title = Subependymal giant cell astrocytoma [Dr Bruno Di Muzio and Dr Jeremy Jones]| url http://radiopaedia.org/articles/subependymal-giant-cell-astrocytoma }}</ref>=== | |||
* T1: heterogenous and hypo- to isointense to grey matter | * T1: heterogenous and hypo- to isointense to grey matter | ||
* T2: heterogenous and hyperintense to grey matter; calcified components can be hypointense | * T2: heterogenous and hyperintense to grey matter; calcified components can be hypointense | ||
* T1 C+ (Gd): can show marked enhancement | * T1 C+ (Gd): can show marked enhancement | ||
{| | |||
| valign=top | | |||
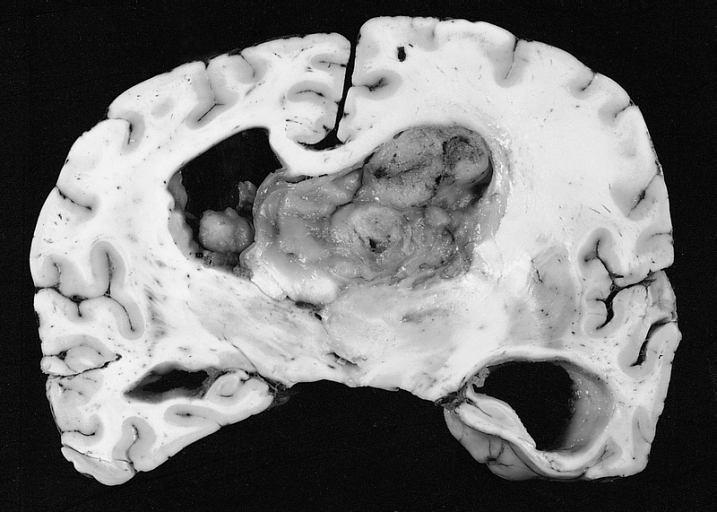
[[File:Astrocytoma 01.jpg|thumb|center|200 px|https://en.wikipedia.org/wiki/Subependymal_giant_cell_astrocytoma]] | |||
|style="width: 300px"| | |||
| [[File:Astrocytoma 02.jpg|thumb|center|200 px|https://en.wikipedia.org/wiki/Subependymal_giant_cell_astrocytoma]] | |||
|} | |||
===Pleomorphic xanthoastrocytomas (PXA)<ref name=Radiopaedia062015>{{cite web | title = Pleomorphic xanthoastrocytomas [Dr Bruno Di Muzio and Dr Frank Gaillard]| url = http://radiopaedia.org/articles/pleomorphic-xanthoastrocytoma }}</ref> === | ===Pleomorphic xanthoastrocytomas (PXA)<ref name=Radiopaedia062015>{{cite web | title = Pleomorphic xanthoastrocytomas [Dr Bruno Di Muzio and Dr Frank Gaillard]| url = http://radiopaedia.org/articles/pleomorphic-xanthoastrocytoma }}</ref> === | ||
* T1 | * T1 | ||
Revision as of 00:39, 24 August 2015
|
Astrocytoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Study |
|
Astrocytoma MRI On the Web |
|
American Roentgen Ray Society Images of Astrocytoma MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Overview
MRI
Low grade infiltrative astrocytoma[1]
- MRI is the modality of choice for characterising these lesions, and in the case of smaller tumours, they may be subtle and difficult to see on CT, especially as they tend not to enhance.
- Reported signal characteristics include:
- T1
- Isointense to hypointense compared to white matter
- Usually confined to the white matters and causes expansion of the adjacent cortex
- T2/FLAIR
- Mass-like hyperintense signals
- Always follow the white matter distribution and cause expansion of the surrounding cortex
- Cortex can also, be involved in late cases in comparison to the oligodendroglioma which is a cortical based tumour from the start
- The "micro-cystic changes" along the lines of spread of the infiltrative astrocytoma is a very unique behavior for the infilterative astrocytoma, however, it is only appreciated in a few number of cases
- High T2 signal is NOT related to cellularity or cellular atypia, but rather oedema, demyelination and other degenerative change 10
- DWI
- No restricted diffusion
- Increased diffusibility is the key to differentiate the diffuse astrocytoma from the acute ischemia
- T1 C+ (Gd)
- No enhancement is often the rule but small ill defined area of enhancement is not rare (as in path proven case 1); however, when enhancement is seen it should be considered as a warning sign for a progression to a higher grade
- MR spectroscopy
- Typical tumour will show elevated choline peak, low NAA peak, elevatedcholine:creatine ratio
- There is lack of the lactate peak seen at 1:33
- The lactate peak represents the necrosis seen in aggressive mostly WHO grade IV tumours
- MR perfusion: no elevation of rCBV
Fibrillary Astrocytoma[2]
- T1: isointense to hypointense compared to white matter
- T2: hyperintense
- T1 C+ (Gd): usually little or no enhancement
- MR spectroscopy: elevated choline:creatine ratio
- MR perfusion: no elevation of rCBV
Protoplasmic Astrocytoma[3]
- These tumours have fairly characteristic appearances[4]:
- T1: hypointense compared to white matter
- T2: strikingly hyperintense
- FLAIR: large areas of T2 hyperintensity suppress on FLAIR (these are not macrocystic but rather represent the areas with abundant microcystic change)
- T1 C+ (Gd): usually little or no enhancement
- MR spectroscopy: elevated choline:creatine ratio
- MR perfusion: there is reduced rCBV
- The key features which should prompt a protoplasmic astrocytoma being raised as the favoured diagnosis are: A) prominent involvement of cortex B) large portions of the tumour demonstrating high T2 signal which suppresses on FLAIR.
Anaplastic astrocytomas
- Anaplastic astrocytomas appear similar to low grade astrocytomas but are more variable in appearance and a single tumour demonstrates more heterogeneity.
- The key to distinguishing anaplastic astrocytomas from low grade tumours is the presence of enhancement which should be absent in the latter (although one should note that variants, especially gemistocytic astrocytomas, can demonstrate enhancement). The pattern of enhancement is very variable 1.
- Unlike glioblastomas, anaplastic astrocytomas lack frank necrosis, and as such central non-enhancing fluid intensity regions should be absent 1.
- T1: hypointense compared to white matter
- T2: generally hyperintense but can be heterogeneous if calcification of blood present
- T1 C+ (Gd)
- Very variable but usually at least some enhancement present
- Presence of ring enhancement suggests central necrosis and thus glioblastoma rather than anaplastic astrocytoma
- MR spectroscopy
- Increased choline: creatine ratio
- NAA preserved or mildly depressed
- No significant lactate
- Intermediate levels of Myo-inositol (lower than low grade, higher than GBM) 2
- MR perfusion: elevated cerebral blood volume
Pilocytic astrocytoma
- General
- Pilocytic astrocytomas range in appearance.
- Large cystic component with a brightly enhancing mural nodule: 67%
- Non enhancing cyst wall: 21%
- Enhancing cyst wall: 46%
- Heterogeneous, mixed solid and multiple cysts and central necrosis: 16%
- Completely solid: 17%
- Enhancement is almost invariably present (~95%). Up to 20% may demonstrate some calcification. Haemorrhage (case 1) is a rare complication.
- Signal characteristics include
- T1: iso to hypointense solid component compared to adjacent brain
- T2: hyperintense solid component compared to adjacent brain
Pilomyxoid Astrocytomas
- Reported signal characteristics include
- T1: isointense
- T2: usually hyperintense
- T1 C+ (Gd): common and is usually in the solid component, but can be also peripheric
Subependymal Giant Cell Astrocytoma[5]
- T1: heterogenous and hypo- to isointense to grey matter
- T2: heterogenous and hyperintense to grey matter; calcified components can be hypointense
- T1 C+ (Gd): can show marked enhancement
 |
 |
Pleomorphic xanthoastrocytomas (PXA)[6]
- T1
- Solid component iso to hypointense c.f. grey matter
- Cystic component low signal
- Leptomeningeal involvement seen in over 70% of cases 2
- T1 C+ (Gd)
- Solid component usually enhances vividly
- T2
- Solid component iso to hyperintense c.f. grey matter
- Cystic component high signal
- Little surrounding vasogenic oedema
Oligoastrocytomas[7]
- T1: usually hypointense
- T2: usually hyperintense
- T1 C+ (Gd): usually non-enhancing lesions
===Spinal astrocytoma[8]
- As astrocytomas arise from cord parenchyma (c.f. ependymomas that arise in the central canal), they typically have an eccentric location within the spinal cord. They may be exophytic, and even appear largely extramedullary. They usually have poorly defined margins. Peritumoral edema is present in 37% 8. Intratumoural cysts are present in approximately 21% and peritumoral cysts are present in aproximately 16% 8.
- Unlike ependymomas, haemorrhage is uncommon.
- Reported signal characteristics include:
- T1: isointense to hypointense
- T2: hyperintense
- T1 C+ (Gd)
References
- ↑ "Low grade infiltrative astrocytoma [Dr Bruno Di Muzio and Dr Frank Gaillard]".
- ↑ "Fibrillary Astrocytoma [Dr Frank Gaillard]".
- ↑ "Protoplasmic astrocytoma [Dr Yuranga Weerakkody and Dr Frank Gaillard]".
- ↑ Tay KL, Tsui A, Phal PM, Drummond KJ, Tress BM (2011). "MR imaging characteristics of protoplasmic astrocytomas". Neuroradiology. 53 (6): 405–11. doi:10.1007/s00234-010-0741-2. PMID 20644924.
- ↑ "Subependymal giant cell astrocytoma [Dr Bruno Di Muzio and Dr Jeremy Jones]". Text " url http://radiopaedia.org/articles/subependymal-giant-cell-astrocytoma " ignored (help); Missing or empty
|url=(help) - ↑ "Pleomorphic xanthoastrocytomas [Dr Bruno Di Muzio and Dr Frank Gaillard]".
- ↑ "Oligoastrocytomas [Dr Bruno Di Muzio and Dr Frank Gaillard]".
- ↑ "Spinalastrocytomas [Dr Bruno Di Muzio and Dr Frank Gaillard]".