Astrocytoma CT: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
{{CMG}} | {{CMG}} | ||
==Overview== | ==Overview== | ||
On cranial CT astrocytoma is characterized by isodense or hypodense regions of positive mass effect, often without any enhancement. Calcification and cystic or fluid attenuation components are also encountered in CT findings depending on the type and grade of tumor. | |||
==CT findings== | ==CT findings== | ||
*A [[Computed Tomography]] (CT) or [[Magnetic Resonance Imaging]] (MRI) scan is necessary to characterize the anatomy of this tumor (size, location, consistency). | *A [[Computed Tomography]] (CT) or [[Magnetic Resonance Imaging]] (MRI) scan is necessary to characterize the anatomy of this tumor (size, location, consistency). | ||
*CT will usually show distortion of third and lateral ventricles with displacement of anterior and middle cerebral arteries. | *CT will usually show distortion of third and lateral ventricles with displacement of anterior and middle cerebral arteries. | ||
* In the first stage of diagnosis the doctor will take a history of symptoms and perform a basic neurological exam, including an eye exam and tests of vision, balance, coordination and mental status. The doctor will then require a computerized tomography (CT) scan and magnetic resonance imaging (MRI) of the patient's brain. | * In the first stage of diagnosis the doctor will take a history of symptoms and perform a basic neurological exam, including an eye exam and tests of vision, balance, coordination and mental status. The doctor will then require a computerized tomography (CT) scan and magnetic resonance imaging (MRI) of the patient's brain. | ||
* During a CT scan, x rays of the patient's brain are taken from many different directions. These are then combined by a computer, producing a cross-sectional image of the brain. | * During a CT scan, x rays of the patient's brain are taken from many different directions. These are then combined by a computer, producing a cross-sectional image of the brain. | ||
Revision as of 10:32, 24 August 2015
|
Astrocytoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Study |
|
Astrocytoma CT On the Web |
|
American Roentgen Ray Society Images of Astrocytoma CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Overview
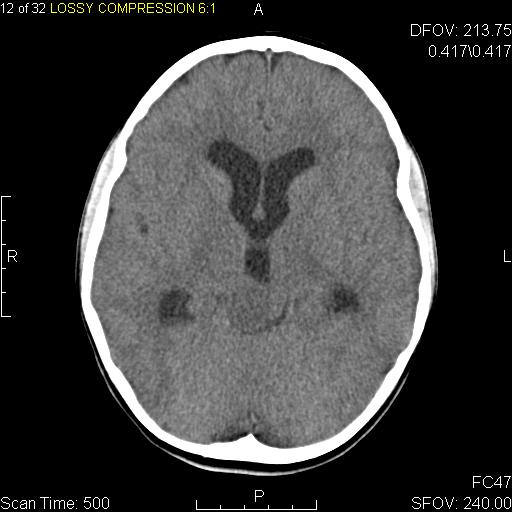
On cranial CT astrocytoma is characterized by isodense or hypodense regions of positive mass effect, often without any enhancement. Calcification and cystic or fluid attenuation components are also encountered in CT findings depending on the type and grade of tumor.
CT findings
- A Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) scan is necessary to characterize the anatomy of this tumor (size, location, consistency).
- CT will usually show distortion of third and lateral ventricles with displacement of anterior and middle cerebral arteries.
- In the first stage of diagnosis the doctor will take a history of symptoms and perform a basic neurological exam, including an eye exam and tests of vision, balance, coordination and mental status. The doctor will then require a computerized tomography (CT) scan and magnetic resonance imaging (MRI) of the patient's brain.
- During a CT scan, x rays of the patient's brain are taken from many different directions. These are then combined by a computer, producing a cross-sectional image of the brain.
- For an MRI, the patient relaxes in a tunnel-like instrument while the brain is subjected to changes of magnetic field. An image is produced based on the behavior of the brain's water molecules in response to the magnetic fields. A special dye may be injected into a vein before these scans to provide contrast and make tumors easier to identify.
 |
Low grade infiltrative astrocytoma[2]
- Typically low grade infiltrating astrocytomas appear as isodense or hypodense regions of positive mass effect, often without any enhancement (in fact presence of enhancement would suggest high tumours), although particularly gemistocytic astrocytomas can demonstrates wispy enhancement.
- Calcification is not seldom (10-20% of cases)1 and may be related to oligodendroglial components (i.e oligoastrocytoma).
- Cystic or fluid attenuation components are also encountered, particularly in gemistocytic and protoplasmic varieties.
Fibrillary Astrocytoma[3]
- Typically fibrillary low grade infiltrating astrocytomas appear as isodense or hypodense regions of positive mass effect, usually without any enhancement (in fact presence of enhancement would suggest high grade, e.g. WHO III or IV tumours.
- Calcification is not infrequently seen (10-20% of cases)1 but is more common in mixed tumours relating to an oligodendroglial components (i.e. oligoastrocytoma).
- Cystic or fluid attenuation components are also encountered although this is far more common in gemistocytic and protoplasmic variants.
Protoplasmic Astrocytoma[4]
- Typically protoplasmic low grade infiltrating astrocytomas appear as hypodense regions of positive mass effect, usually without any enhancement (in fact presence of enhancement would suggest high grade tumours). Areas of the tumour appear of fluid attenuation, due to the aforementioned prominent mucinous microcystic component.
Anaplastic astrocytomas
- CT appearances are intermediate, appearing as regions of low attenuation with positive mass effect. Enhancement is variable.
Subependymal Giant Cell Astrocytoma[5]
- The foramen of Monro is the classic location, and the tumour arises when a subependymal nodule transforms into SGCA over a period of time.
- Typically appears as an intraventricular mass near the foramen of Monro
- They are usually larger than 1 cm
- Lesions are iso- or slightly hypoattenuating to grey matter
- Calcification is common and haemorrhage is possible
- Accompanying hydrocephalus may be present
- Often shows marked contrast enhancement (subependymal nodules also enhance)
Pleomorphic xanthoastrocytomas (PXA)[6]
- PXAs are typically hypo or isodense and may be well or poorly demarcated, usually with little surrounding oedema. Calcification is rare. Due to its superfical location it may cause scalloping of the overlying bone .[7]
- Often there is a cystic component (50-60%) with an enhancing mural nodule. Additionally they are one of the tumours that may exhibit a dural tail, which is reactive rather than due to direct dural invasion, which is rare .
References
- ↑ "Wikipedia".
- ↑ "Low grade infiltrative astrocytoma [Dr Bruno Di Muzio and Dr Frank Gaillard]".
- ↑ "Fibrillary Astrocytoma [Dr Frank Gaillard]".
- ↑ "Protoplasmic astrocytoma [Dr Yuranga Weerakkody and Dr Frank Gaillard]".
- ↑ "Subependymal giant cell astrocytoma [Dr Bruno Di Muzio and Dr Jeremy Jones]".
- ↑ "Pleomorphic xanthoastrocytomas [Dr Bruno Di Muzio and Dr Frank Gaillard]".
- ↑ Koeller KK, Rushing EJ (2004). "From the archives of the AFIP: pilocytic astrocytoma: radiologic-pathologic correlation". Radiographics. 24 (6): 1693–708. doi:10.1148/rg.246045146. PMID 15537977.