Arrhythmogenic right ventricular dysplasia
| Arrhythmogenic right ventricular dysplasia | |
 | |
|---|---|
| ICD-10 | I42.8 |
| OMIM | 107970 |
| DiseasesDB | 29750 |
| MeSH | D019571 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and Keywords: ARVD, arrhythmogenic right ventricular cardiomyopathy or ARVC
Overview
Arrhythmogenic right ventricular dysplasia is a type of nonischemic cardiomyopathy that involves primarily the right ventricle. It is characterized by hypokinetic areas involving the free wall of the right ventricle, with fibrofatty replacement of the right ventricular myocardium, with associated arrhythmias originating in the right ventricle.
Epidemiology and Demographics
ARVD is an important cause of ventricular arrhythmias in children and young adults. It is seen predominantly in males, and 30-50% of cases have a familial distribution.
The incidence of ARVD is about 1/10,000 in the general population in the United States, although some studies have suggested that it may be as common as 1/1,000. It accounts for up to 17% of all sudden cardiac deaths in the young. In Italy, the incidence is 40/10,000, making it the most common cause of sudden cardiac death in the young population.
Pathogenesis
The pathogenesis of ARVD is largely unknown. Apoptosis (programmed cell death) appears to play a large role. It is unclear why only the right ventricle is involved. The disease process starts in the subepicardial region and works its way towards the endocardial surface, leading to transmural involvement (possibly accounting for the aneurysmal dilatation of the RV). Residual myocardium is confined to the subendocardial region and the trabeculae of the RV. These trabeculae may become hypertrophied.
Aneurysmal dilatation is seen in 50% of cases at autopsy. It usually occurs in the diaphragmatic, apical, and infundibular regions (known as the triangle of dysplasia). The left ventricle is involved in 50-67% of individuals. If the left ventricle is involved, it is usually late in the course of disease, and confers a poor prognosis.
There are two pathological patterns seen in ARVD, Fatty infiltration and fibro-fatty infiltration.
Fatty infiltration
The first, fatty infiltration, is confined to the right ventricle. This involves a partial or near-complete substitution of myocardium with fatty tissue without wall thinning. It involves predominantly the apical and infundibular regions of the RV. The left ventricle and ventricular septum are usually spared. No inflammatory infiltrates are seen in fatty infiltration. There is evidence of myocyte (myocardial cell) degeneration and death seen in 50% of cases of fatty infiltration.
Fibro-fatty infiltration
The second, fibro-fatty infiltration, involves replacement of myocytes with fibrofatty tissue. A patchy myocarditis is involved in up to 2/3 of cases, with inflammatory infiltrates (mostly T cells) seen on microscopy. Myocardial atrophy is due to injury and apoptosis. This leads to thinning of the RV free wall (to < 3 mm thickness) Myocytes are replaced with fibrofatty tissue. The regions preferentially involved include the RV inflow tract, the RV outflow tract, and the RV apex. However, the LV free wall may be involved in some cases. Involvement of the ventricular septum is rare. The areas involved are prone to aneurysm formation.
Genetics
It is usually inherited in an autosomal dominant pattern, with variable expression. The penetrance is 20-35% in general, but significantly higher in Italy. Seven gene loci have been implicated in ARVD. However, about 50% of families that express ARVD that undergo genetic screening do not show linkage with any of the known chromosomal loci. It is unclear whether the pathogenesis varies with the different loci involved. A standard genetic screening test is not available.
Differential Diagnosis
The differential diagnosis for the ventricular tachycardia due to ARVD include:
- Congenital heart disease
- Repaired tetralogy of Fallot
- Ebstein's anomaly
- Uhl anomaly
- Atrial septal defect
- Partial anomalous venous return
- Acquired heart disease
- Tricuspid valve disease
- Pulmonary hypertension
- Right ventricular infarction
- Bundle-branch re-entrant tachycardia
- Miscellaneous
- Pre-excited AV re-entry tachycardia
- Idiopathic RVOT tachycardia
Diagnosis
Symptoms
Up to 80% of individuals with ARVD present with syncope or sudden cardiac death. The remainder frequently present with palpitations or other symptoms due to right ventricular outflow tract (RVOT) tachycardia (a type of monomorphic ventricular tachycardia).
Symptoms are usually exercise-related. In populations where hypertrophic cardiomyopathy is screened out prior to involvement in competitive athletics, it is a common cause of sudden cardiac death.
The first clinical signs of ARVD are usually during adolescence. However, signs of ARVD have been demonstrated in infants.
Ventricular arrhythmias
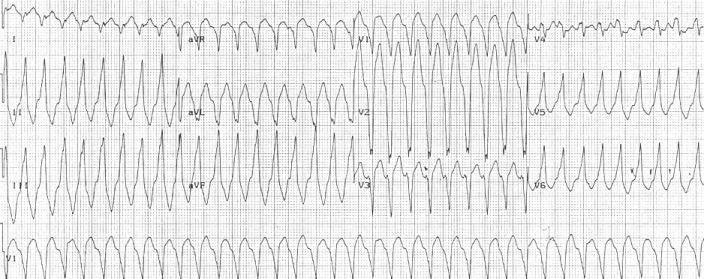 Right ventricular outflow tract tachycardia |
| Monomorphic ventricular tachycardia originating from the right ventricular outflow tract. |
Ventricular arrhythmias due to ARVD typically arise from the diseased right ventricle. The type of arrhythmia ranges from frequent premature ventricular complexes (PVCs) to ventricular tachycardia (VT) to ventricular fibrillation (VF).
While the initiating factor of the ventricular arrhythmias is unclear, it may be due to triggered activity or reentry.
Ventricular arrhythmias are usually exercise-related, suggesting that they are sensitive to catecholamines. The ventricular beats typically have a right axis deviation. Multiple morphologies of ventricular tachycardia may be present in the same individual, suggesting multiple arrhythmogenic foci or pathways.
Right ventricular outflow tract (RVOT) tachycardia is the most common VT seen in individuals with ARVD. In this case, the EKG shows a left bundle branch block (LBBB) morphology with an inferior axis.
Clinical testing
In order to make the diagnosis of ARVD, a number of clinical tests are employed, including the electrocardiogram (EKG), echocardiography, right ventricular angiography, and cardiac MRI.
Researchers at Beth Israel Deaconess Medical Center in Boston have demonstrated an immunohistochemical test that reliably diagnoses ARVD. Doctors were able to correctly diagnose 10 of 11 subjects with definite ARVD and correctly ruled it out in another 10 of 11 subjects, according to results published in the New England Journal of Medicine[1]. The authors conclude more research is needed but the results hold promise for identifying the condition when it can still be treated. "This is a disease in many cases where the first and only symptom is sudden death. And then it's discovered in autopsy," senior author Dr. Jeffrey Saffitz told WikiDoc. "The next step will be testing whether a skin test could detect (ARVC)," Saffitz says, which would eliminate the need for the heart biopsy Saffitz' team used in conducting their ARVC test.
Electrocardiogram
90% of individuals with ARVD have some EKG abnormality. The most common EKG abnormality seen in ARVD is T wave inversion in leads V1 to V3. However, this is a non-specific finding, and may be considered a normal variant in right bundle branch block (RBBB), women, and children under 12 years old.
RBBB itself is seen frequently in individuals with ARVD. This may be due to delayed activation of the right ventricle, rather than any intrinsic abnormality in the right bundle branch.
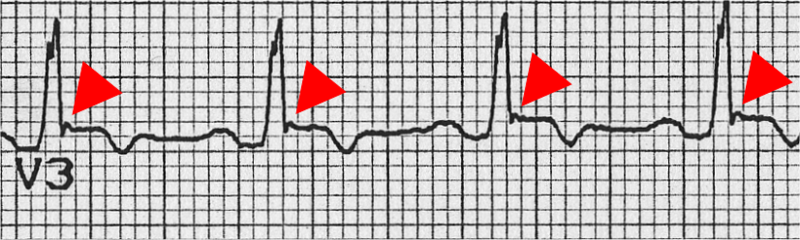 The epsilon wave | |
| The epsilon wave (red triangle), seen in ARVD. |
The epsilon wave is found in about 50% of those with ARVD. This is described as a terminal notch in the QRS complex. It is due to slowed intraventricular conduction. The epsilon wave may be seen on a surface EKG; however, it is more commonly seen on signal averaged EKGs.
Ventricular ectopy seen on a surface EKG in the setting of ARVD is typically of left bundle branch block (LBBB) morphology, with a QRS axis of -90 to +110 degrees. The origin of the ectopic beats is usually from one of the three regions of fatty degeneration (the "triangle of dysplasia"): the RV outflow tract, the RV inflow tract, and the RV apex.

Summary of EKG Characteristics
- Incomplete or complete RBBB
- Inverted T waves in the anterior precordial leads
- Localized prolongation of the QRS complex in leads V1 and V2
- Epsilon waves visible as sharp discrete deflections at the terminal portion of the QRS complex in the anterior precordial leads
- Use QRS width in Lead I which is always <120ms
- Lead III R>S
- S wave upstroke in V1 - V3 >55ms was found in 95 percent of ARVD
Signal averaged ECG
Signal averaged ECG (SAECG) is used to detect late potentials and epsilon waves in individuals with ARVD.
Echocardiography
Echocardiography may reveal an enlarged, hypokinetic right ventricle with a paper-thin RV free wall. The dilatation of the RV will cause dilatation of the tricuspid valve annulus, with subsequent tricuspid regurgitation.Paradoxical septal motion may also be present.
- Right Ventricular Dysplasia 1
<googlevideo>-8417307416816520415&hl=en</googlevideo>
- Right Ventricular Dysplasia 2
<googlevideo>-8312017427182612822&hl=en</googlevideo>
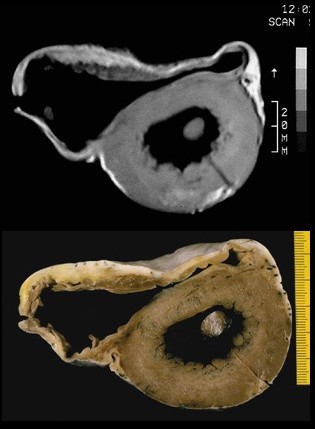
Cardiac MRI
Fatty infiltration of the RV free wall can be visible on cardiac MRI. Fat has increased intensity in T1-weighted images. However, it may be difficult to differentiate intramyocardial fat and the epicardial fat that is commonly seen adjacent to the normal heart. Also, the sub-tricuspid region may be difficult to distinguish from the atrioventricular sulcus, which is rich in fat.
Cardiac MRI can visualize the extreme thinning and akinesis of the RV free wall. However, the normal RV free wall may be about 3 mm thick, making the test less sensitive.
- The typical criteria that can be demonstrated with MR imaging are
- Fatty infiltration of the right ventricular myocardium with high signal intensity on T1-weighted images(major criterion)
- Fibrofatty replacement, which leads to diffuse thinning of the right ventricular myocardium (major criterion)
- Aneurysms of the right ventricle and right ventricular outflow tract (major criterion)
- Dilatation of the right ventricle and right ventricular outflow tract (when severe, major criterion; when mild, minor criterion)
- Regional contraction abnormalities (minor criterion)
- Global systolic dysfunction (major criterion) and global diastolic dysfunction (minor criterion).

Right ventricular angiography
Right ventricular angiography is considered the gold standard for the diagnosis of ARVD. Findings consistent with ARVD are an akinetic or dyskinetic bulging localized to the infundibular, apical, and subtricuspid regions of the RV. The specificity is 90%; however, the test is observer dependent.
Right ventricular biopsy
Transvenous biopsy of the right ventricle can be highly specific for ARVD, but it has low sensitivity. False positives include other conditions with fatty infiltration of the ventricle, such as chronic alcohol abuse and Duchenne/Becker muscular dystrophy.
False negatives are common, however, because the disease progresses typically from the epicardium to the endocardium (with the biopsy sample coming from the endocardium), and the segmental nature of the disease. Also, due to the paper-thin right ventricular free wall that is common in this disease process, most biopsy samples are taken from the ventricular septum, which is commonly not involved in the disease process.
A biopsy sample that is consistent with ARVD would have > 3% fat, >40% fibrous tissue, and <45% myocytes.
Histopathological Findings
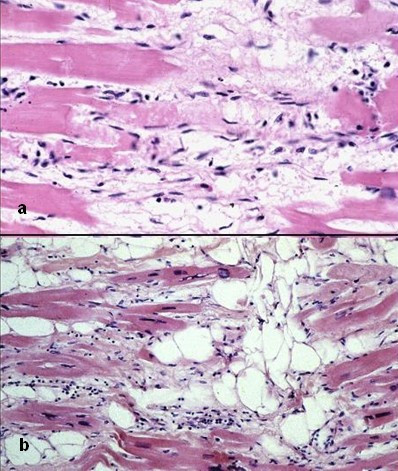
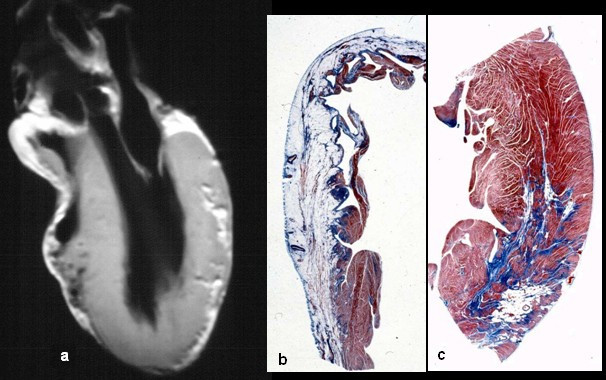
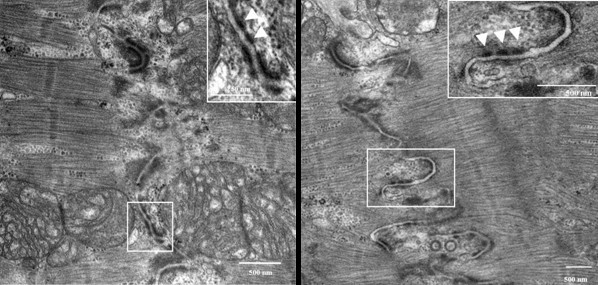
Autopsy
A post mortem histological demonstration of full thickness substitution of the RV myocardium by fatty or fibro-fatty tissue is consistent with ARVD.
Diagnostic Criteria
There is no pathognomonic feature of ARVD. The diagnosis of ARVD is based on a combination of major and minor criteria. To make a diagnosis of ARVD requires either 2 major criteria or 1 major and 2 minor criteria or 4 minor criteria.
Major Criteria
- Right ventricular dysfunction
- Severe dilatation and reduction of RV ejection fraction with little or no LV impairment
- Localized RV aneurysms
- Severe segmental dilatation of the RV
- Tissue characterization
- Fibrofatty replacement of myocardium on endomyocardial biopsy
- Conduction abnormalities
- Epsilon waves in V1 - V3.
- Localized prolongation (>110 ms) of QRS in V1 - V3
- Family history
- Familial disease confirmed on autopsy or surgery
Minor Criteria
- Right ventricular dysfunction
- Mild global RV dilatation and/or reduced ejection fraction with normal LV.
- Mild segmental dilatation of the RV
- Regional RV hypokinesis
- Tissue characterization
- Conduction abnormalities
- Inverted T waves in V2 and V3 in an individual over 12 years old, in the absence of a right bundle branch block (RBBB)
- Late potentials on signal averaged EKG.
- Ventricular tachycardia with a left bundle branch block (LBBB) morphology
- Frequent PVCs (> 1000 PVCs / 24 hours)
- Family history
- Family history of sudden cardiac death before age 35
- Family history of ARVD
Treatment
The goal of management of ARVD is to decrease the incidence of sudden cardiac death. This raises a clinical dilemma: How to prophylactically treat the asymptomatic patient who was diagnosed during family screening.
A certain subgroup of individuals with ARVD are considered at high risk for sudden cardiac death. Characteristics associated with high risk of sudden cardiac death include:
- Young age
- Competitive sports activity
- Malignant familial history
- Extensive RV disease with decreased right ventricular ejection fraction.
- Left ventricular involvement
- Syncope
- Episode of ventricular arrhythmia
Management options include pharmacological, surgical, catheter ablation, and placement of an implantable cardioverter-defibrillator.
Prior to the decision of the treatment option, programmed electrical stimulation in the electrophysiology laboratory may be performed for additional prognostic information. Goals of programmed stimulation include:
- Assessment of the disease's arrhythmogenic potential
- Evaluate the hemodynamic consequences of sustained VT
- Determine whether the VT can be interrupted via antitachycardia pacing.
Regardless of the management option chosen, the individual is typically suggested to undergo lifestyle modification, including avoidance of strenuous exercise, cardiac stimulants (ie: caffeine, nicotine, pseudoephedrine) and alcohol. If the individual wishes to begin an exercise regimen, an exercise stress test may have added benefit.
Pharmacologic management
Pharmacologic management of ARVD involves arrhythmia suppression and prevention of thrombus formation.
Sotalol, a beta blocker and a class III antiarrhythmic agent, is the most effective antiarrhythmic agent in ARVD. Other antiarrhythmic agents used include amiodarone and conventional beta blockers (ie: metoprolol). If antiarrhythmic agents are used, their efficacy should be guided by series ambulatory holter monitoring, to show a reduction in arrhythmic events.
While angiotensin converting enzyme inhibitors (ACE Inhibitors) are well known for slowing progression in other cardiomyopathies, they have not been proven to be helpful in ARVD.
Individuals will decreased RV ejection fraction with dyskinetic portions of the right ventricle may benefit from long term anticoagulation with warfarin to prevent thrombus formation and subsequent pulmonary embolism.
Catheter ablation
Catheter ablation may be used to treat intractable ventricular tachycardia. It has a 60-90% success rate.[2] Unfortunately, due to the progressive nature of the disease, recurrence is common (60% recurrence rate), with the creation of new arrhythmogenic foci. Indications for catheter ablation include drug-refractory VT and frequent recurrence of VT after ICD placement, causing frequent discharges of the ICD.
Implantable cardioverter-defibrillator
An ICD is the most effective prevention against sudden cardiac death. Due to the prohibitive cost of ICDs, they are not routinely placed in all individuals with ARVD.
Indications for ICD placement in the setting of ARVD include:
- Cardiac arrest due to VT or VF
- Symptomatic VT that is not inducible during programmed stimulation
- Failed programmed stimulation-guided drug therapy
- Severe RV involvement with poor tolerance of VT
- Sudden death of immediate family member
Since ICDs are typically placed via a transvenous approach into the right ventricle, there are complications associated with ICD placement and follow-up.
Due to the extreme thinning of the RV free wall, it is possible to perforation the RV during implantation, potentially causing pericardial tamponade. Because of this, every attempt is made at placing the defibrillator lead on the ventricular septum.
After a successful implantation, the progressive nature of the disease may lead to fibro-fatty replacement of the myocardium at the site of lead placement. This may lead to undersensing of the individual's electrical activity (potentially causing inability to sense VT or VF), and inability to pace the ventricle.
Cardiac transplant surgery
Cardiac transplant surgery is rarely performed in ARVD. It may be indicated if the arrhythmias associated with the disease are uncontrollable or if there is severe bi-ventricular heart failure that is not manageable with pharmacological therapy.
Family screening
All first degree family members of the affected individual should be screened for ARVD. This is used to establish the pattern of inheritance. Screening should begin during the teenage years unless otherwise indicated. Screening tests include:
- Echocardiogram
- EKG
- Signal averaged EKG
- Holter monitoring
- Cardiac MRI
- Exercise stress test
Prognosis
There is a long asymptomatic lead-time in individuals with ARVD. While this is a genetically transmitted disease, individuals in their teens may not have any characteristics of ARVD on screening tests.
Many individuals have symptoms associated with ventricular tachycardia, such as palpitations, light-headedness, or syncope. Others may have symptoms and signs related to right ventricular failure, such as lower extremity edema, or liver congestion with elevated hepatic enzymes (hepatopathy). Unfortunately, sudden cardiac death may be the first manifestation of disease.
ARVD is a progressive disease. Over time, the right ventricle becomes more involved, leading to right ventricular failure. The right ventricle will fail before there is left ventricular dysfunction. However, by the time the individual has signs of overt right ventricular failure, there will be histological involvement of the left ventricle. Eventually, the left ventricle will also become involved, leading to bi-ventricular failure. Signs and symptoms of left ventricular failure may become evident, including congestive heart failure, atrial fibrillation, and an increased incidence of thromboembolic events.
References
- ↑ Asimaki A, Tandri H, Huang H; et al. (2009). "A new diagnostic test for arrhythmogenic right ventricular cardiomyopathy". N. Engl. J. Med. 360 (11): 1075–84. doi:10.1056/NEJMoa0808138. PMID 19279339. Unknown parameter
|month=ignored (help) - ↑ Fontaine G, Tonet J, Gallais Y, Lascault G, Hidden-Lucet F, Aouate P, Halimi F, Poulain F, Johnson N, Charfeddine H, Frank R. (2000). "Ventricular tachycardia catheter ablation in arrhythmogenic right ventricular dysplasia: a 16-year experience". Curr Cardiol Rep. 2 (6): 498–506. PMID 11203287.
Additional Resources
- Ahmad F, Li D, Karibe A, et al. Localization of a gene responsible for arrhythmogenic right ventricular dysplasia to chromosome 3p23. Circulation. Dec 22-29 1998;98(25):2791-5.
- Basso C, Thiene G, Corrado D, et al. Arrhythmogenic right ventricular cardiomyopathy. Dysplasia, dystrophy, or myocarditis?. Circulation. Sep 1 1996;94(5):983-91.
- Blake LM, Scheinman MM, Higgins CB. MR features of arrhythmogenic right ventricular dysplasia. AJR Am J Roentgenol. Apr 1994;162(4):809-12.
- Bomma C, Dalal D, Tandri H, Prakasa K, Nasir K, Roguin A. Evolving role of multidetector computed tomography in evaluation of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Am J Cardiol. Jul 1 2007;100(1):99-105.
- Burke AP, Farb A, Tashko G, Virmani R. Arrhythmogenic right ventricular cardiomyopathy and fatty replacement of the right ventricular myocardium: are they different diseases?. Circulation. Apr 28 1998;97(16):1571-80.
- Carlson MD, White RD, Trohman RG, et al. Right ventricular outflow tract ventricular tachycardia: detection of previously unrecognized anatomic abnormalities using cine magnetic resonance imaging. J Am Coll Cardiol. Sep 1994;24(3):720-7.
- Celbis O, Aydin NE, Mizrak B, Ozdemir B. Arrhythmogenic right ventricular dysplasia cases in forensic autopsies. Am J Forensic Med Pathol. Sep 2007;28(3):235-7.
- Corrado D, Basso C, Thiene G, et al. Spectrum of clinicopathologic manifestations of arrhythmogenic right ventricular cardiomyopathy/dysplasia: a multicenter study. J Am Coll Cardiol. Nov 15 1997;30(6):1512-20.
- Daliento L, Rizzoli G, Thiene G, et al. Diagnostic accuracy of right ventriculography in arrhythmogenic right ventricular cardiomyopathy. Am J Cardiol. Sep 15 1990;66(7):741-5.
- El Masry HZ, Yadav AV. Arrhythmogenic right ventricular dysplasia/cardiomyopathy. Expert Rev Cardiovasc Ther. Feb 2008;6(2):249-60.
- Fontaine G, Fontaliran F, Hebert JL, et al. Arrhythmogenic right ventricular dysplasia. Annu Rev Med. 1999;50:17-35.
- Fontaine G, Gallais Y, Fornes P, Hébert JL, Frank R. Arrhythmogenic right ventricular dysplasia/cardiomyopathy. Anesthesiology. Jul 2001;95(1):250-4.
- Fontaine G, Tonet J, Gallais Y, et al. Ventricular tachycardia catheter ablation in arrhythmogenic right ventricular dysplasia: a 16-year experience. Curr Cardiol Rep. Nov 2000;2(6):498-506.
- Kantarci M, Bayraktutan U, Sevimli S, Bayram E, Durur I. Multidetector computed tomography findings of arrhythmogenic right ventricular dysplasia: a case report. Heart Surg Forum. 2007;10(6):E431-3.
- Kinsara AJ, Zaman L, Gorgels A. Arrhythmogenic right ventricular dysplasia. Am J Emerg Med. Jan 2001;19(1):67-70.
- Li D, Ahmad F, Gardner MJ, et al. The locus of a novel gene responsible for arrhythmogenic right- ventricular dysplasia characterized by early onset and high penetrance maps to chromosome 10p12-p14. Am J Hum Genet. Jan 2000;66(1):148-56.
- Midiri M, Finazzo M, Brancato M, et al. Arrhythmogenic right ventricular dysplasia: MR features. Eur Radiol. 1997;7(3):307-12.
- Midiri M, Finazzo M. MR imaging of arrhythmogenic right ventricular dysplasia. Int J Cardiovasc Imaging. Aug 2001;17(4):297-304.
- Moric-Janiszewska E, Markiewicz-Loskot G. Review on the genetics of arrhythmogenic right ventricular dysplasia. Europace. May 2007;9(5):259-66.
- Peters S. Left ventricular impairment in arrhythmogenic right ventricular dysplasia: what we can learn from angiography. Cardiology. 1995;86(6):473-6.
- Rampazzo A, Nava A, Danieli GA, et al. The gene for arrhythmogenic right ventricular cardiomyopathy maps to chromosome 14q23-q24. Hum Mol Genet. Jun 1994;3(6):959-62.
- Rampazzo A, Nava A, Miorin M, et al. ARVD4, a new locus for arrhythmogenic right ventricular cardiomyopathy, maps to chromosome 2 long arm. Genomics. Oct 15 1997;45(2):259-63.
- Ricci C, Longo R, Pagnan L, et al. Magnetic resonance imaging in right ventricular dysplasia. Am J Cardiol. Dec 15 1992;70(20):1589-95.
- Segal HN. Parchment heart. Am Heart J. 1950;40:948.
- Severini GM, Krajinovic M, Pinamonti B, et al. A new locus for arrhythmogenic right ventricular dysplasia on the long arm of chromosome 14. Genomics. Jan 15 1996;31(2):193-200.
- Tandri H, Macedo R, Calkins H, Marcus F, Cannom D, Scheinman M. Role of magnetic resonance imaging in arrhythmogenic right ventricular dysplasia: insights from the North American arrhythmogenic right ventricular dysplasia (ARVD/C) study. Am Heart J. Jan 2008;155(1):147-53.
- Van der Wall EE, Kayser HW, Bootsma MM, et al. Arrhythmogenic right ventricular dysplasia: MRI findings. Herz. 25(4):356-64.
- White RD, Trohman RG, Flamm SD, et al. Right ventricular arrhythmia in the absence of arrhythmogenic dysplasia: MR imaging of myocardial abnormalities. Radiology. Jun 1998;207(3):743-51.
- Wichter T, Hindricks G, Lerch H, et al. Regional myocardial sympathetic dysinnervation in arrhythmogenic right ventricular cardiomyopathy. An analysis using 123I-meta-iodobenzylguanidine scintigraphy. Circulation. Feb 1994;89(2):667-83
- Willerson JT, Cohn JN. Cardiovascular Medicine. 2nd ed. New York, NY: Churchill Livingstone; 2000: 1665-76.