Arachnoid cyst
| Arachnoid cyst | ||
 | ||
|---|---|---|
| Suprasellar Arachnoid Cyst; Extension into posterior fossa and displacing the pons (T1 - MRI) Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | ||
| ICD-10 | Q04.6 | |
| ICD-9 | 348.0 | |
| OMIM | 207790 | |
| DiseasesDB | 33219 | |
| MeSH | D016080 | |
|
Arachnoid cyst Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Arachnoid cyst On the Web |
|
American Roentgen Ray Society Images of Arachnoid cyst |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Causes
The exact cause of arachnoid cysts is not known. Researchers believe that most cases of arachnoid cysts are developmental malformations that arise from the unexplained splitting or tearing of the arachnoid membrane. According to the medical literature, cases of arachnoid cysts have run in families (familial cases) suggesting that a genetic predisposition may play a role in the development of arachnoid cysts in some individuals.
In some cases, arachnoid cysts occurring in the middle fossa are accompanied by underdevelopment (hypoplasia) or compression of the temporal lobe. The exact role that temporal lobe abnormalities play in the development of middle fossa arachnoid cysts is unknown.
In a few rare cases, intracranial arachnoid cysts may be inherited as an autosomal recessive trait. In recessive disorders, the condition does not appear unless a person inherits the same defective gene for the same trait from each parent. If an individual receives one normal gene and one gene for the disease, the person will be a carrier for the disease, but usually will not show symptoms. The risk of transmitting the disease to the children of a couple, both of whom are carriers for a recessive disorder, is 25 percent. Fifty percent of their children risk being carriers of the disease, but generally will not show symptoms of the disorder. Twenty-five percent of their children may receive both normal genes, one from each parent, and will be genetically normal (for that particular trait). The risk is the same for each pregnancy.
In a few rare cases, spinal intradural arachnoid cysts may be inherited as an autosomal dominant trait..
Some complications of arachnoid cysts can occur when a cyst is damaged because of minor head trauma. Trauma can cause the fluid within a cyst to leak into other areas (e.g., subarachnoid space). Blood vessels on the surface of a cyst may tear and bleed into the cyst (intracystic hemorrhage), increasing its size. If a blood vessel bleeds on the outside of a cyst, a collection of blood (hematoma) may result. In the cases of intracystic hemorrhage and hematoma, the individual may have symptoms of increased pressure within the cranium and signs of compression of nearby nerve (neural) tissue.
Arachnoid cysts can also occur secondary to other disorders such as Marfan’s syndrome, arachnoiditis, or agenesis of the corpus callosum. (For more information on these disorders, choose the specific disorder name as your search term in the Rare Disease Database.)[3]
Diagnosis
Diagnosis is principally by MRI. Frequently, arachnoid cysts are incidental findings on MRI scans performed for other clinical reasons. In practice, diagnosis of symptomatic arachnoid cysts requires symptoms to be present, and many with the disorder never develop symptoms.
Additional clinical assessment tools that may be useful in evaluating a patient with arachnoid cysts include the mini-mental state examination (MMSE), a brief questionnaire-based test used to assess cognition.[1] Myelograms are contraindicated for people with arachnoid cysts.
MRI
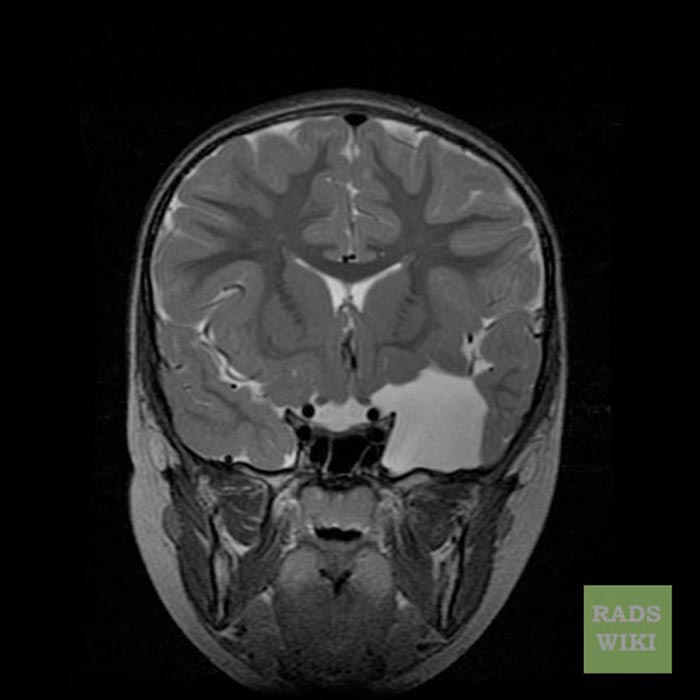
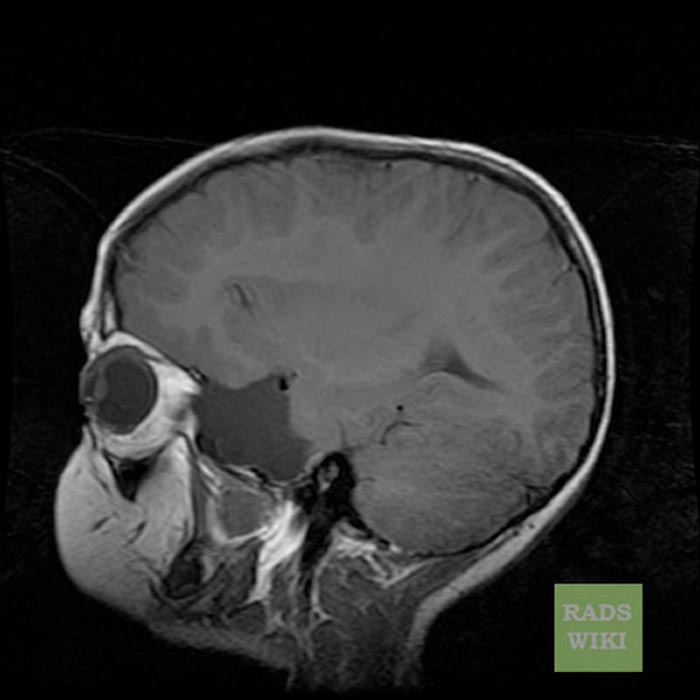
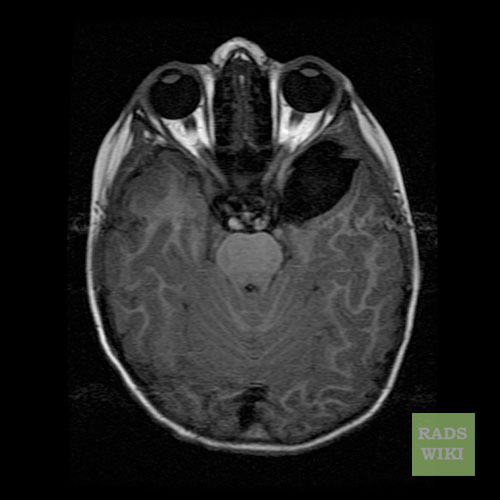
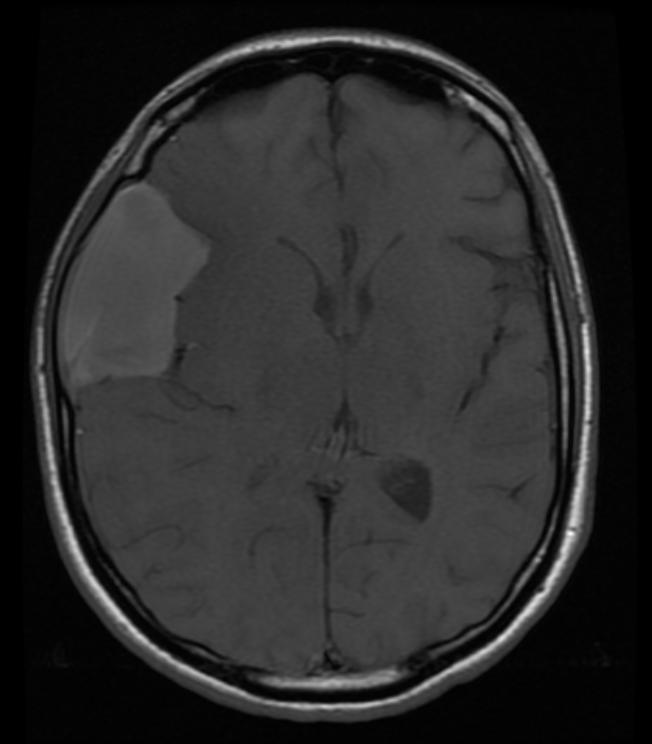
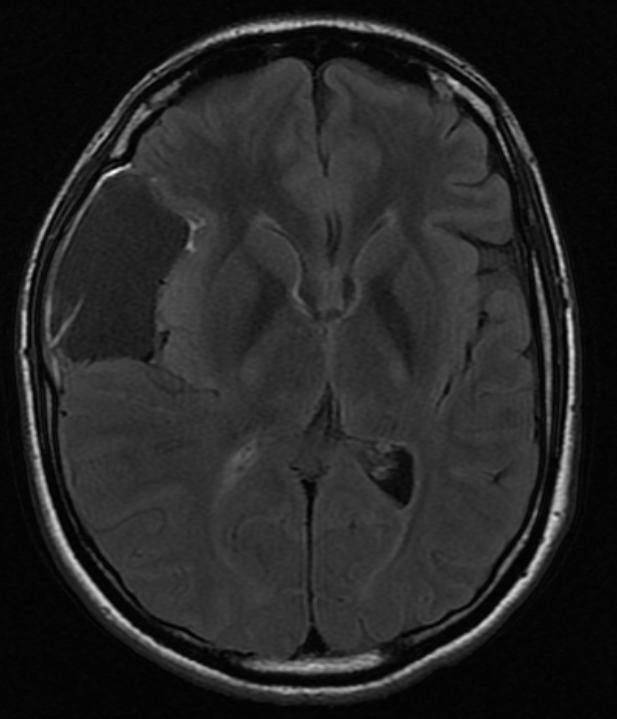
Patient #1: Left middle cranial fossa arachnoid cyst
-
Cor T2
-
Sag T1
-
Axial T1 FLAIR
-
Axial T2
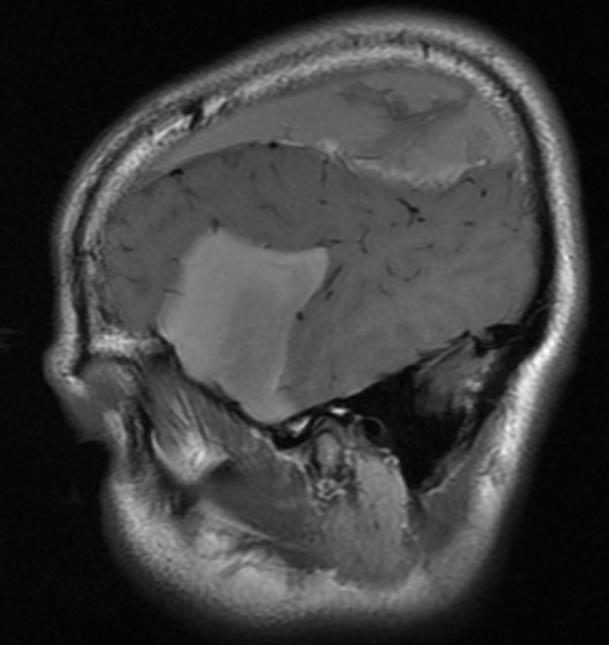
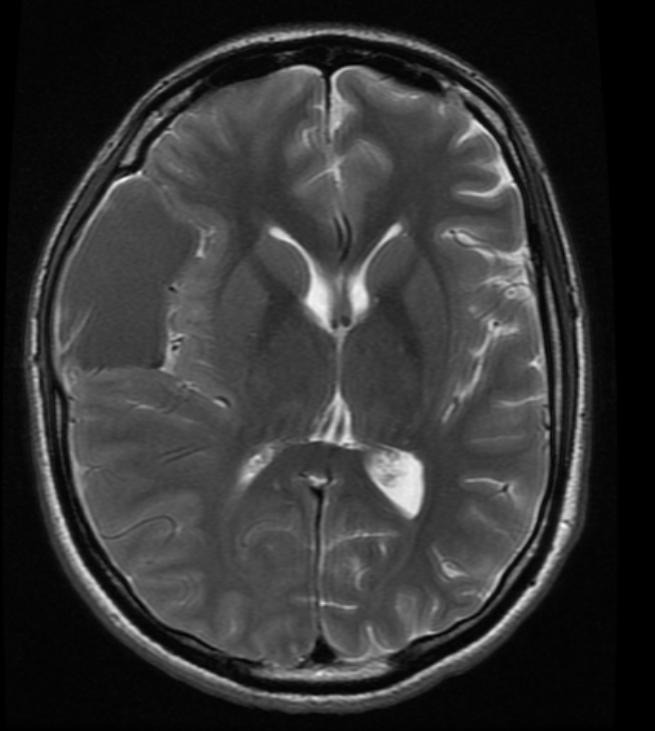
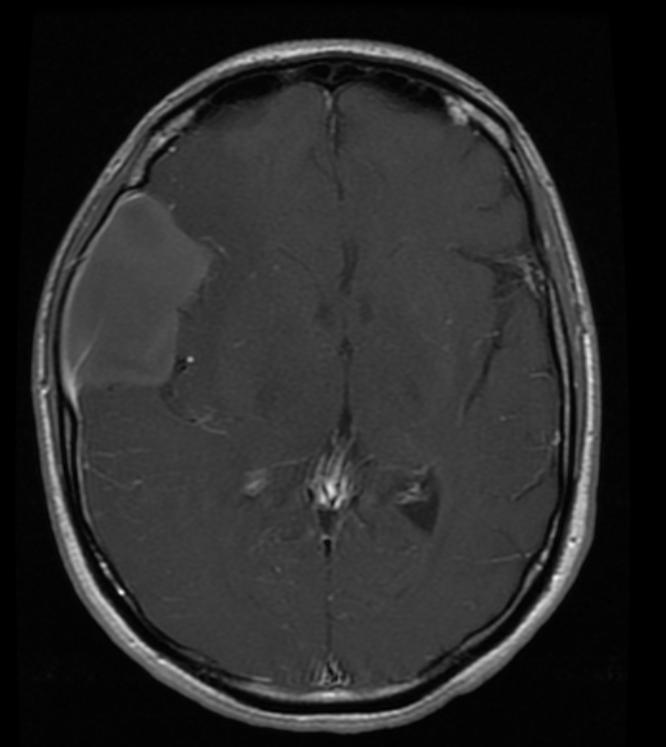
Patient #2: CT and MR images demonstrate a hemorrhagic arachnoid cyst
-
CT
-
Sag T1
-
Ax T1
-
Ax FLAIR
-
Ax T2
-
Ax T1 with GAD
Treatment/Management
Treatment for arachnoid cysts occurs when symptoms present themselves.[2] A variety of procedures may be used to decompress (remove pressure from) the cyst.
- Surgical placement of a cerebral shunt:[3]
- An internal shunt drains into the subdural compartment.[4]
- A cystoperitoneal shunt drains to the peritoneal cavity.
- Fenestration:
- Craniotomy with excision
- Various endoscopic techniques are proving effective,[5] including laser-assisted techniques.[6]
- Drainage by needle aspiration or burr hole. While these procedures are relatively simple, there is a high incidence of recurrence.
- Capsular resection[7]
- Pharmacological treatments may address specific symptoms such as seizures or pain.
A 1994 study found surgery necessary for good outcome in patients >65 years old when the cysts began displaying symptoms.[8]
Sleep aids are often necessary as most people with Arachnoid Cysts do not sleep.
Prognosis
Untreated, arachnoid cysts may cause permanent severe neurological damage due to the progressive expansion of the cyst(s) or hemorrhage (bleeding).[2] With treatment most individuals with arachnoid cysts do well with the double edge sword of developing surgical arachnoiditis which can cause its own specific problems and can lead to "popping" another cyst.
More specific prognoses are listed below:
- Patients with arachnoid cysts of the left temporal fossa who experienced impaired preoperative cognition had postoperative improvement.[9]
- Surgery can resolve psychiatric manifestations in selected cases.[10]
Epidemiology
Arachnoid cysts are seen in 4% of the population.[11] Only 20% of these have symptoms, usually from secondary hydrocephalus.[11]
A study that looked at 2,536 healthy young males found a prevalence of 1.7% (95% CI 1.2 to 2.3%). Only a small percentage of the detected abnormalities require urgent medical attention.[12]
See also
- Acoustic Neuroma
- Arachnoiditis
- Brain Tumors, General
- Dandy-Walker Syndrome
- Empty Sella Syndrome
- Epidermoids
- Midline Caves of the Brain
- Porencephaly
- Syringomyelia
- Bobble-Head Doll Syndrome
- Hyperprolactinemia
- Panhypopituitarism
- Arnold-Chiari Malformation
Patient Information
What are Arachnoid Cysts?
Arachnoid cysts are cerebrospinal fluid-filled sacs that are located between the brain or spinal cord and the arachnoid membrane, one of the three membranes that cover the brain and spinal cord. Primary arachnoid cysts are present at birth and are the result of developmental abnormalities in the brain and spinal cord that arise during the early weeks of gestation. Secondary arachnoid cysts are not as common as primary cysts and develop as a result of head injury, meningitis, or tumors, or as a complication of brain surgery. The majority of arachnoid cysts form outside the temporal lobe of the brain in an area of the skull known as the middle crania fossa. Arachnoid cysts involving the spinal cord are rarer. The location and size of the cyst determine the symptoms and when those symptoms begin. Most individuals with arachnoid cysts develop symptoms before the age of 20, and especially during the first year of life, but some people with arachnoid cysts never have symptoms. Males are four times more likely to have arachnoid cysts than females.
Typical symptoms of an arachnoid cyst around the brain include headache, nausea and vomiting, seizures, hearing and visual disturbances, vertigo, and difficulties with balance and walking. Arachnoid cysts around the spinal cord compress the spinal cord or nerve roots and cause symptoms such as progressive back and leg pain and tingling or numbness in the legs or arms. Diagnosis usually involves a brain scan using diffusion-weighted MRI (magnetic resonance imaging) which helps distinguish fluid-filled arachnoid cysts from other types of cysts.
Is there any treatment?
There has been active debate about how to treat arachnoid cysts. The need for treatment depends mostly upon the location and size of the cyst. If the cyst is small, not disturbing surrounding tissue, and not causing symptoms, some doctors will refrain from treatment. In the past, doctors placed shunts in the cyst to drain its fluid. Now with microneurosurgical techniques and endoscopic tools that allow for minimally invasive surgery, more doctors are opting to surgically remove the membranes of the cyst or open the cyst so its fluid can drain into the cerebrospinal fluid and be absorbed.
What is the prognosis?
Untreated, arachnoid cysts may cause permanent severe neurological damage when progressive expansion of the cyst(s) or hemorrhage injures the brain or spinal cord. Symptoms usually resolve or improve with treatment.
What research is being done?
The National Institute of Neurological Disorders and Stroke (NINDS) conducts research related to brain abnormalities and disorders of the nervous system such as arachnoid cysts in laboratories at the National Institutes of Health (NIH), and supports additional research through grants to major medical institutions across the country. Much of this research focuses on finding better ways to prevent, treat, and ultimately cure neurological disorders such as arachnoid cysts.
References
- ↑
- ↑ 2.0 2.1
- ↑ Strojnik T. "Different approaches to surgical treatment of arachnoid cysts", Wiener Klinische Wochenschrift.[1] 2006;118 Suppl 2:85-8. (PMID 16817052)
- ↑ Helland CA, Wester K. "Arachnoid cysts in adults: long-term follow-up of patients treated with internal shunts to the subdural compartment", Surg Neurol. 2006 Jul;66(1):56-61; discussion 61. (PMID 16793443)
- ↑ Greenfield JP, Souweidane MM. "Endoscopic management of intracranial cysts", Neurosurg Focus. 2005 Dec 15;19(6):E7. (PMID 16398484)
- ↑ Van Beijnum J, Hanlo PW, Han KS, Ludo Van der Pol W, Verdaasdonk RM, Van Nieuwenhuizen O. "Navigated laser-assisted endoscopic fenestration of a suprasellar arachnoid cyst in a 2-year-old child with bobble-head doll syndrome", J Neurosurg. 2006 May;104(5 Suppl):348-51. (PMID 16848093)
- ↑
- ↑ Caruso R, Salvati M, Cervoni L. "Primary intracranial arachnoid cyst in the elderly", Neurosurg Rev. 1994;17(3):195-8. (PMID 7838397)
- ↑ Wester K, Hugdahl K. "Arachnoid cysts of the left temporal fossa: impaired preoperative cognition and postoperative improvement." J Neurol Neurosurg Psychiatry 1995 Sep;59(3):293-8. (PMID 7673959)
- ↑ Kohn R, Lilly RB, Sokol MS, Malloy PF. "Psychiatric presentations of intracranial cysts", J Neuropsychiatry Clin Neurosci 1989; 1:60-66. (PMID 2577719)
- ↑ 11.0 11.1 Flaherty AW. The Massachusetts General Hospital Handbook of Neurology 2000 Jan 1;105. (ISBN 0-683-30576-X)
- ↑ Weber F, Knopf H. "Incidental findings in magnetic resonance imaging of the brains of healthy young men", J Neurol Sci. 2006 Jan 15;240(1-2):81-4. Epub 2005 Oct 26. (PMID 16256141)
External Links
Patient support sites: