Aortoiliac disease: Difference between revisions
| (36 intermediate revisions by the same user not shown) | |||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
Aortoilliac disease also known as Aorotilliac occlusive disease or Leriche Syndrome is a type of Peripheral Arterial Disease (PAD). Peripheral Arterial Disease is caused by occlusion of an artery<ref>{{Cite journal | Aortoilliac disease also known as Aorotilliac occlusive disease or Leriche Syndrome is a type of [[Peripheral Arterial Disease]] (PAD). [[Peripheral Arterial Disease]] is caused by occlusion of an artery<ref>{{Cite journal | ||
| author = [[Edgardo Olvera Lopez]] & [[Arif Jan]] | | author = [[Edgardo Olvera Lopez]] & [[Arif Jan]] | ||
| title = Cardiovascular Disease | | title = Cardiovascular Disease | ||
| Line 11: | Line 11: | ||
| month = January | | month = January | ||
| pmid = 30571040 | | pmid = 30571040 | ||
}}</ref> due to atherosclerotic plaque buildup, thrombosis or embolism. PAD normally affects the distal femoral artery, but Aortoilliac disease is caused by occlusion of the infrarenal aorta and beyond. The Aorta gives off the renal branches at the L1/ L2 spine level and it branches into the Right and Left Common Illiac Arteries at the L4 spine level. Aortoilliac disease can include the Common Illiac arteries and it's branches.<ref>{{Cite journal | }}</ref> due to [[atherosclerotic]] plaque buildup, [[thrombosis]] or [[embolism]]. PAD normally affects the distal femoral artery, but Aortoilliac disease is caused by occlusion of the infrarenal aorta and beyond. The Aorta gives off the renal branches at the L1/ L2 [[spine]] level and it branches into the Right and Left Common Illiac Arteries at the L4 [[spine]] level. Aortoilliac disease can include the Common Illiac arteries and it's branches.<ref>{{Cite journal | ||
| author = [[Candace Wooten]], [[Munawar Hayat]], [[Maira du Plessis]], [[Alper Cesmebasi]], [[Michael Koesterer]], [[Kevin P. Daly]], [[Petru Matusz]], [[R. Shane Tubbs]] & [[Marios Loukas]] | | author = [[Candace Wooten]], [[Munawar Hayat]], [[Maira du Plessis]], [[Alper Cesmebasi]], [[Michael Koesterer]], [[Kevin P. Daly]], [[Petru Matusz]], [[R. Shane Tubbs]] & [[Marios Loukas]] | ||
| title = Anatomical significance in aortoiliac occlusive disease | | title = Anatomical significance in aortoiliac occlusive disease | ||
| Line 23: | Line 23: | ||
| pmid = 25065617 | | pmid = 25065617 | ||
}}</ref> Depending on it's underlying cause it can present acutely or chronically. | }}</ref> Depending on it's underlying cause it can present acutely or chronically. | ||
Acute causes include thrombosis and embolism, while chronic causes include atherosclerotic plaque formation | Acute causes include [[thrombosis]] and [[embolism]], while chronic causes include atherosclerotic plaque formation | ||
==Classification== | ==Classification== | ||
| Line 61: | Line 61: | ||
**Gadofosveset-enhanced MR angiography showed significant improvement (P < .001) compared with unenhanced MR angiography for diagnosis of clinically significant aortoiliac occlusive disease ( 50% stenosis) . | **Gadofosveset-enhanced MR angiography showed significant improvement (P < .001) compared with unenhanced MR angiography for diagnosis of clinically significant aortoiliac occlusive disease ( 50% stenosis) . | ||
**The improvement in diagnostic efficacy compared with unenhanced MR angiography was clearly demonstrated. There was an improvement in overall accuracy, sensitivity, and specificity. | **The improvement in diagnostic efficacy compared with unenhanced MR angiography was clearly demonstrated. There was an improvement in overall accuracy, sensitivity, and specificity. | ||
*CT Angiography | *CT Angiography <ref>{{Cite journal | ||
| author = [[Michael R. Jaff]], [[Christopher J. White]], [[William R. Hiatt]], [[Gerry R. Fowkes]], [[John Dormandy]], [[Mahmood Razavi]], [[Jim Reekers]] & [[Lars Norgren]] | |||
| title = An Update on Methods for Revascularization and Expansion of the TASC Lesion Classification to Include Below-the-Knee Arteries: A Supplement to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II): The TASC Steering Comittee(.) | |||
| journal = [[Annals of vascular diseases]] | |||
| volume = 8 | |||
| issue = 4 | |||
| pages = 343–357 | |||
| year = 2015 | |||
| month = | |||
| doi = 10.3400/avd.tasc.15-01000 | |||
| pmid = 26730266 | |||
}}</ref> <ref>{{Cite journal | |||
| author = [[Mahmoud Assaad]], [[Sunit Tolia]] & [[Marcel Zughaib]] | |||
| title = Leriche syndrome: The inferior mesenteric artery saves the lower extremity | |||
| journal = [[SAGE open medical case reports]] | |||
| volume = 5 | |||
| pages = 2050313X17740513 | |||
| year = 2017 | |||
| month = | |||
| doi = 10.1177/2050313X17740513 | |||
| pmid = 29147567 | |||
}}</ref> | |||
**CT angiographic examination is less invasive and less expensive than conventional angiography | **CT angiographic examination is less invasive and less expensive than conventional angiography | ||
**Improves resolution with decreased contrast load and acquisition time without increasing radiation exposure | **Improves resolution with decreased contrast load and acquisition time without increasing radiation exposure | ||
==Indications for Revascularization== | ==Indications for Revascularization== | ||
*Relief of symptomatic lower extremity ischemia, including claudication, rest pain, ulceration or gangrene, or embolization causing blue toe syndrome | *Relief of symptomatic lower extremity ischemia, including claudication, rest pain, ulceration or gangrene, or embolization causing blue toe syndrome | ||
| Line 181: | Line 203: | ||
==Classification== | ==Classification== | ||
*Aortoilliac disease may be classified according to Trans-Atlantic Intercontinental Consensus guidelines | *Aortoilliac disease may be classified according to Trans-Atlantic Intercontinental Consensus guidelines <ref>{{Cite journal | ||
<ref>{{Cite journal | |||
| author = [[Michael R. Jaff]], [[Christopher J. White]], [[William R. Hiatt]], [[Gerry R. Fowkes]], [[John Dormandy]], [[Mahmood Razavi]], [[Jim Reekers]] & [[Lars Norgren]] | | author = [[Michael R. Jaff]], [[Christopher J. White]], [[William R. Hiatt]], [[Gerry R. Fowkes]], [[John Dormandy]], [[Mahmood Razavi]], [[Jim Reekers]] & [[Lars Norgren]] | ||
| title = An Update on Methods for Revascularization and Expansion of the TASC Lesion Classification to Include Below-the-Knee Arteries: A Supplement to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II): The TASC Steering Comittee(.) | | title = An Update on Methods for Revascularization and Expansion of the TASC Lesion Classification to Include Below-the-Knee Arteries: A Supplement to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II): The TASC Steering Comittee(.) | ||
| Line 214: | Line 235: | ||
==Pathophysiology== | ==Pathophysiology== | ||
*The pathogenesis of aortoilliac disease is characterized by atherosclerotic plaque buildup, Thrombosis or an embolus. | *The pathogenesis of aortoilliac disease is characterized by [[atherosclerotic]] plaque buildup, [[Thrombosis]] or an [[embolus]]. | ||
* | **Atherosclerosis is the buildup of cholesterol plaques in the arteries. Damage to the endothelial layer of the vessel wall allows for inflammatory cells, mediators and fatty acids to enter the intimal layer of the artery. Overtime the plaques can enlarge and cause stenosis of the vessel lumen. Thrombosis occurs when a piece of the plaque dislodges and causes an occlusion. | ||
*On gross pathology, cholesterol plaques, fatty streaks, and areas of ulceration and hemorrhage are characteristic findings of atherosclerosis and thrombus formation in aortoilliac disease.<ref>{{Cite journal | *On gross pathology, cholesterol plaques, fatty streaks, and areas of [[ulceration]] and [[hemorrhage]] are characteristic findings of [[atherosclerosis]] and [[thrombus]] formation in aortoilliac disease.<ref>{{Cite journal | ||
| author = [[William Jr Insull]] | | author = [[William Jr Insull]] | ||
| title = The pathology of atherosclerosis: plaque development and plaque responses to medical treatment | | title = The pathology of atherosclerosis: plaque development and plaque responses to medical treatment | ||
| Line 243: | Line 264: | ||
==Clinical Features== | ==Clinical Features== | ||
Clinical features of aortoilliac disease include: | Clinical features of aortoilliac disease include: | ||
* Claudication of legs and buttocks<ref>{{Cite journal | * [[Claudication]] of legs and buttocks<ref>{{Cite journal | ||
| author = [[Wei-Jing Lee]], [[Yung-Ze Cheng]] & [[Hung-Jung Lin]] | | author = [[Wei-Jing Lee]], [[Yung-Ze Cheng]] & [[Hung-Jung Lin]] | ||
| title = Leriche syndrome | | title = Leriche syndrome | ||
| Line 266: | Line 287: | ||
| pmid = 30082092 | | pmid = 30082092 | ||
}}</ref> | }}</ref> | ||
* Pallor of lower limbs<ref>{{Cite journal | * [[Pallor]] of lower limbs<ref>{{Cite journal | ||
| author = [[Wei-Jing Lee]], [[Yung-Ze Cheng]] & [[Hung-Jung Lin]] | | author = [[Wei-Jing Lee]], [[Yung-Ze Cheng]] & [[Hung-Jung Lin]] | ||
| title = Leriche syndrome | | title = Leriche syndrome | ||
| Line 278: | Line 299: | ||
| pmid = 19384523 | | pmid = 19384523 | ||
}}</ref> | }}</ref> | ||
* Numbness of lower limbs<ref>{{Cite journal | * [[Numbness]] of lower limbs<ref>{{Cite journal | ||
| author = [[Naomi M. Hamburg]] & [[Mark A. Creager]] | | author = [[Naomi M. Hamburg]] & [[Mark A. Creager]] | ||
| title = Pathophysiology of Intermittent Claudication in Peripheral Artery Disease | | title = Pathophysiology of Intermittent Claudication in Peripheral Artery Disease | ||
| Line 325: | Line 346: | ||
| pmid = 19384523 | | pmid = 19384523 | ||
}}</ref> | }}</ref> | ||
* Erectile dysfunction<ref>{{Cite journal | * [[Erectile dysfunction]] <ref>{{Cite journal | ||
| author = [[Wei-Jing Lee]], [[Yung-Ze Cheng]] & [[Hung-Jung Lin]] | | author = [[Wei-Jing Lee]], [[Yung-Ze Cheng]] & [[Hung-Jung Lin]] | ||
| title = Leriche syndrome | | title = Leriche syndrome | ||
| Line 348: | Line 369: | ||
| pmid = 30082092 | | pmid = 30082092 | ||
}}</ref> | }}</ref> | ||
* Atrophy of affected muscles in the lower limb<ref>{{Cite journal | * [[Atrophy]] of affected muscles in the lower limb<ref>{{Cite journal | ||
| author = [[Naomi M. Hamburg]] & [[Mark A. Creager]] | | author = [[Naomi M. Hamburg]] & [[Mark A. Creager]] | ||
| title = Pathophysiology of Intermittent Claudication in Peripheral Artery Disease | | title = Pathophysiology of Intermittent Claudication in Peripheral Artery Disease | ||
| Line 363: | Line 384: | ||
==Differentiating Aortoilliac Disease from other Diseases== | ==Differentiating Aortoilliac Disease from other Diseases== | ||
*Aortoilliac disease must be differentiated from other diseases that cause lower limb claudication, lower limb weakness/atrophy, and loss of femoral pulses such as: | *Aortoilliac disease must be differentiated from other diseases that cause lower limb claudication, lower limb weakness/atrophy, and loss of femoral pulses such as: | ||
:*Peripheral artery disease of the Lower limbs | :*[[Peripheral artery disease]] of the Lower limbs <ref>{{Cite journal | ||
:*Compartment syndrome | | author = [[Gurbir Dhaliwal]] & [[Debabrata Mukherjee]] | ||
:*Chronic venous | | title = Peripheral arterial disease: Epidemiology, natural history, diagnosis and treatment | ||
| journal = [[The International journal of angiology : official publication of the International College of Angiology, Inc]] | |||
| volume = 16 | |||
| issue = 2 | |||
| pages = 36–44 | |||
| year = 2007 | |||
| month = Summer | |||
| pmid = 22477268 | |||
}}</ref> | |||
:*[[Compartment syndrome]] <ref>{{Cite journal | |||
| author = [[Brit Long]], [[Alex Koyfman]] & [[Michael Gottlieb]] | |||
| title = Evaluation and Management of Acute Compartment Syndrome in the Emergency Department | |||
| journal = [[The Journal of emergency medicine]] | |||
| year = 2019 | |||
| month = January | |||
| doi = 10.1016/j.jemermed.2018.12.021 | |||
| pmid = 30685220 | |||
}}</ref> | |||
:*[[Chronic venous insufficiency]] | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
* The prevalence of [disease | * The prevalence of [[peripheral arterial disease]] is approximately 200 million individuals worldwide.<ref>{{Cite journal | ||
| author = [[F. Gerry R. Fowkes]], [[Victor Aboyans]], [[Freya J. I. Fowkes]], [[Mary M. McDermott]], [[Uchechukwu K. A. Sampson]] & [[Michael H. Criqui]] | |||
| title = Peripheral artery disease: epidemiology and global perspectives | |||
| journal = [[Nature reviews. Cardiology]] | |||
| volume = 14 | |||
| issue = 3 | |||
| pages = 156–170 | |||
| year = 2017 | |||
| month = March | |||
| doi = 10.1038/nrcardio.2016.179 | |||
| pmid = 27853158 | |||
}}</ref> | |||
===Age=== | ===Age=== | ||
| Line 399: | Line 448: | ||
| pmid = 17223489 | | pmid = 17223489 | ||
}}</ref> | }}</ref> | ||
===Race=== | ===Race=== | ||
*There is no racial predilection for | *There is no racial predilection for aortoilliac disease. | ||
==Risk Factors== | ==Risk Factors== | ||
*Common risk factors in the development of aortoilliac disease are smoking, diabetes mellitus, dyslipidemia, and hypertension.<ref>{{Cite journal | *Common risk factors in the development of aortoilliac disease are smoking, [[diabetes mellitus]], [[dyslipidemia]], and [[hypertension]].<ref>{{Cite journal | ||
| author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | | author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | ||
| title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | | title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | ||
| Line 421: | Line 466: | ||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
*Early clinical features include intermittent [[claudication]], decreased lower limb pulses, and [[erectile dysfunction]].<ref>{{Cite journal | |||
*Early clinical features include intermittent claudication, decreased lower limb pulses, and erectile dysfunction.<ref>{{Cite journal | |||
| author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | | author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | ||
| title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | | title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | ||
| Line 433: | Line 477: | ||
| pmid = 17223489 | | pmid = 17223489 | ||
}}</ref> | }}</ref> | ||
*If left untreated, | *If left untreated, patients with aortoilliac disease may progress to develop [[critical limb ischemia]], muscle [[atrophy]], and poor wound healing.<ref>{{Cite journal | ||
| author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | | author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | ||
| title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | | title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | ||
| Line 444: | Line 488: | ||
| pmid = 17223489 | | pmid = 17223489 | ||
}}</ref> | }}</ref> | ||
* | *Prognosis is generally good, and the 5 year mortality rate of patients with [[peripheral arterial disease]] as a whole is approximately 33.2%. <ref>{{Cite journal | ||
| author = [[Jaime Caro]], [[Kristen Migliaccio-Walle]], [[Khajak J. Ishak]] & [[Irina Proskorovsky]] | |||
| title = The morbidity and mortality following a diagnosis of peripheral arterial disease: long-term follow-up of a large database | |||
| journal = [[BMC cardiovascular disorders]] | |||
| volume = 5 | |||
| pages = 14 | |||
| year = 2005 | |||
| month = June | |||
| doi = 10.1186/1471-2261-5-14 | |||
| pmid = 15972099 | |||
}}</ref> | |||
== Diagnosis == | == Diagnosis == | ||
===Diagnostic Criteria=== | ===Diagnostic Criteria=== | ||
*The diagnosis of aortoilliac disease is made when 3 of the following diagnostic criteria are met: | *The diagnosis of aortoilliac disease is made when 3 of the following diagnostic criteria are met: | ||
:* claudication<ref>{{Cite journal | :* [[claudication]]<ref>{{Cite journal | ||
| author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | | author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | ||
| title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | | title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | ||
| Line 472: | Line 525: | ||
| pmid = 17223489 | | pmid = 17223489 | ||
}}</ref> | }}</ref> | ||
:* erectile dysfunction<ref>{{Cite journal | :* [[erectile dysfunction]]<ref>{{Cite journal | ||
| author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | | author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | ||
| title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | | title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | ||
| Line 483: | Line 536: | ||
| pmid = 17223489 | | pmid = 17223489 | ||
}}</ref> | }}</ref> | ||
=== Symptoms === | === Symptoms === | ||
*Peripheral arterial disease may start out asymptomatic. Symptoms depend on the arteries affected. | *Peripheral arterial disease may start out asymptomatic. Symptoms depend on the arteries affected. | ||
*Symptoms of aortoilliac disease may include the following: | *Symptoms of aortoilliac disease may include the following: | ||
:* | :*[[claudication]] of lower limbs<ref>{{Cite journal | ||
| author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | | author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | ||
| title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | | title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | ||
| Line 499: | Line 551: | ||
| pmid = 17223489 | | pmid = 17223489 | ||
}}</ref> | }}</ref> | ||
:*erectile dysfunction<ref>{{Cite journal | :*[[erectile dysfunction]]<ref>{{Cite journal | ||
| author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | | author = [[L. Norgren]], [[W. R. Hiatt]], [[J. A. Dormandy]], [[M. R. Nehler]], [[K. A. Harris]] & [[F. G. R. Fowkes]] | ||
| title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | | title = Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) | ||
| Line 560: | Line 612: | ||
| pmid = 29147567 | | pmid = 29147567 | ||
}}</ref> | }}</ref> | ||
:*atrophy of lower limb<ref>{{Cite journal | :*[[atrophy]] of lower limb<ref>{{Cite journal | ||
| author = [[Keiichiro Kita]] | | author = [[Keiichiro Kita]] | ||
| title = Leriche syndrome (Aortoiliac occlusive disease) | | title = Leriche syndrome (Aortoiliac occlusive disease) | ||
| Line 583: | Line 635: | ||
| pmid = 29147567 | | pmid = 29147567 | ||
}}</ref> | }}</ref> | ||
:*pallor<ref>{{Cite journal | :*[[pallor]]<ref>{{Cite journal | ||
| author = [[Mahmoud Assaad]], [[Sunit Tolia]] & [[Marcel Zughaib]] | | author = [[Mahmoud Assaad]], [[Sunit Tolia]] & [[Marcel Zughaib]] | ||
| title = Leriche syndrome: The inferior mesenteric artery saves the lower extremity | | title = Leriche syndrome: The inferior mesenteric artery saves the lower extremity | ||
| Line 594: | Line 646: | ||
| pmid = 29147567 | | pmid = 29147567 | ||
}}</ref> | }}</ref> | ||
:*cyanosis<ref>{{Cite journal | :*[[cyanosis]]<ref>{{Cite journal | ||
| author = [[Mahmoud Assaad]], [[Sunit Tolia]] & [[Marcel Zughaib]] | | author = [[Mahmoud Assaad]], [[Sunit Tolia]] & [[Marcel Zughaib]] | ||
| title = Leriche syndrome: The inferior mesenteric artery saves the lower extremity | | title = Leriche syndrome: The inferior mesenteric artery saves the lower extremity | ||
| Line 605: | Line 657: | ||
| pmid = 29147567 | | pmid = 29147567 | ||
}}</ref> | }}</ref> | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
* | *Laboratory findings consistent with the diagnosis of Peripheral artery disease including aortoilliac disease include abnormal lipid panel <ref>{{Cite journal | ||
| author = [[Duane R. Hennion]] & [[Kelly A. Siano]] | |||
| title = Diagnosis and treatment of peripheral arterial disease | |||
| journal = [[American family physician]] | |||
| volume = 88 | |||
| issue = 5 | |||
| pages = 306–310 | |||
| year = 2013 | |||
| month = September | |||
| pmid = 24010393 | |||
}}</ref> and abnormal inflammatory markers. | |||
** Elevated [[cholesterol]] | |||
** Elevated [[LDL]] | |||
** Elevated [[ESR]] | |||
** Elevated [[CRP]]<ref>{{Cite journal | |||
| author = [[P. M. Ridker]], [[M. J. Stampfer]] & [[N. Rifai]] | |||
| title = Novel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease | |||
| journal = [[JAMA]] | |||
| volume = 285 | |||
| issue = 19 | |||
| pages = 2481–2485 | |||
| year = 2001 | |||
| month = May | |||
| pmid = 11368701 | |||
}}</ref> <ref>{{Cite journal | |||
| author = [[H. E. Stoffers]], [[A. D. Kester]], [[V. Kaiser]], [[P. E. Rinkens]] & [[J. A. Knottnerus]] | |||
| title = Diagnostic value of signs and symptoms associated with peripheral arterial occlusive disease seen in general practice: a multivariable approach | |||
| journal = [[Medical decision making : an international journal of the Society for Medical Decision Making]] | |||
| volume = 17 | |||
| issue = 1 | |||
| pages = 61–70 | |||
| year = 1997 | |||
| month = January-March | |||
| doi = 10.1177/0272989X9701700107 | |||
| pmid = 8994152 | |||
}}</ref> | |||
** Elevated [[homocysteine]] <ref>{{Cite journal | |||
| author = [[P. M. Ridker]], [[M. J. Stampfer]] & [[N. Rifai]] | |||
| title = Novel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease | |||
| journal = [[JAMA]] | |||
| volume = 285 | |||
| issue = 19 | |||
| pages = 2481–2485 | |||
| year = 2001 | |||
| month = May | |||
| pmid = 11368701 | |||
}}</ref> <ref>{{Cite journal | |||
| author = [[H. E. Stoffers]], [[A. D. Kester]], [[V. Kaiser]], [[P. E. Rinkens]] & [[J. A. Knottnerus]] | |||
| title = Diagnostic value of signs and symptoms associated with peripheral arterial occlusive disease seen in general practice: a multivariable approach | |||
| journal = [[Medical decision making : an international journal of the Society for Medical Decision Making]] | |||
| volume = 17 | |||
| issue = 1 | |||
| pages = 61–70 | |||
| year = 1997 | |||
| month = January-March | |||
| doi = 10.1177/0272989X9701700107 | |||
| pmid = 8994152 | |||
}}</ref> | |||
===Imaging Findings=== | ===Imaging Findings=== | ||
*CT angiography is the imaging modality of choice for aortoilliac disease. | *[[CT angiography]] is the imaging modality of choice for aortoilliac disease.<ref>{{Cite journal | ||
*On CT angiography, aortoilliac disease is characterized by occlusion of the Common Illiac, External Illiac, or Common Femoral Arteries. | | author = [[Daniel G. Clair]] & [[Jocelyn M. Beach]] | ||
*Doppler Ultrasound may demonstrate decreases blood flow in the Common Illiac, External Illiac, or Common Femoral Arteries. | | title = Strategies for managing aortoiliac occlusions: access, treatment and outcomes | ||
*Abdominal ultrasound may also be used to aid in diagnosis | | journal = [[Expert review of cardiovascular therapy]] | ||
| volume = 13 | |||
| issue = 5 | |||
| pages = 551–563 | |||
| year = 2015 | |||
| month = May | |||
| doi = 10.1586/14779072.2015.1036741 | |||
| pmid = 25907618 | |||
}}</ref> | |||
*On [[CT angiography]], aortoilliac disease is characterized by occlusion of the Common Illiac, External Illiac, or Common Femoral Arteries.<ref>{{Cite journal | |||
| author = [[Michael R. Jaff]], [[Christopher J. White]], [[William R. Hiatt]], [[Gerry R. Fowkes]], [[John Dormandy]], [[Mahmood Razavi]], [[Jim Reekers]] & [[Lars Norgren]] | |||
| title = An Update on Methods for Revascularization and Expansion of the TASC Lesion Classification to Include Below-the-Knee Arteries: A Supplement to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II): The TASC Steering Comittee(.) | |||
| journal = [[Annals of vascular diseases]] | |||
| volume = 8 | |||
| issue = 4 | |||
| pages = 343–357 | |||
| year = 2015 | |||
| month = | |||
| doi = 10.3400/avd.tasc.15-01000 | |||
| pmid = 26730266 | |||
}}</ref> <ref>{{Cite journal | |||
| author = [[Mahmoud Assaad]], [[Sunit Tolia]] & [[Marcel Zughaib]] | |||
| title = Leriche syndrome: The inferior mesenteric artery saves the lower extremity | |||
| journal = [[SAGE open medical case reports]] | |||
| volume = 5 | |||
| pages = 2050313X17740513 | |||
| year = 2017 | |||
| month = | |||
| doi = 10.1177/2050313X17740513 | |||
| pmid = 29147567 | |||
}}</ref> | |||
*Doppler [[Ultrasound]] may demonstrate decreases blood flow in the Common Illiac, External Illiac, or Common Femoral Arteries. <ref>{{Cite journal | |||
| author = [[S. Karacagil]], [[A. M. Lofberg]], [[B. Almgren]], [[A. Granbo]], [[M. L. Jonsson]], [[L. E. Lorelius]] & [[D. Bergqvist]] | |||
| title = Duplex ultrasound scanning for diagnosis of aortoiliac and femoropopliteal arterial disease | |||
| journal = [[VASA. Zeitschrift fur Gefasskrankheiten]] | |||
| volume = 23 | |||
| issue = 4 | |||
| pages = 325–329 | |||
| year = 1994 | |||
| month = | |||
| pmid = 7817613 | |||
}}</ref> <ref>{{Cite journal | |||
| author = [[Gurbir Dhaliwal]] & [[Debabrata Mukherjee]] | |||
| title = Peripheral arterial disease: Epidemiology, natural history, diagnosis and treatment | |||
| journal = [[The International journal of angiology : official publication of the International College of Angiology, Inc]] | |||
| volume = 16 | |||
| issue = 2 | |||
| pages = 36–44 | |||
| year = 2007 | |||
| month = Summer | |||
| pmid = 22477268 | |||
}}</ref> | |||
*Abdominal [[ultrasound]] may also be used to aid in diagnosis. <ref>{{Cite journal | |||
| author = [[Mahmoud Assaad]], [[Sunit Tolia]] & [[Marcel Zughaib]] | |||
| title = Leriche syndrome: The inferior mesenteric artery saves the lower extremity | |||
| journal = [[SAGE open medical case reports]] | |||
| volume = 5 | |||
| pages = 2050313X17740513 | |||
| year = 2017 | |||
| month = | |||
| doi = 10.1177/2050313X17740513 | |||
| pmid = 29147567 | |||
}}</ref> | |||
=== Other Diagnostic Studies === | === Other Diagnostic Studies === | ||
*Peripheral Arterial disease including aortoilliac disease may also be diagnosed using Ankle Brachial Index. | *[[Peripheral Arterial disease]] including aortoilliac disease may also be diagnosed using [[Ankle Brachial Index]]. <ref>{{Cite journal | ||
*Ankle Brachial Index < 0.9 is | | author = [[Mahmoud Assaad]], [[Sunit Tolia]] & [[Marcel Zughaib]] | ||
| title = Leriche syndrome: The inferior mesenteric artery saves the lower extremity | |||
| journal = [[SAGE open medical case reports]] | |||
| volume = 5 | |||
| pages = 2050313X17740513 | |||
| year = 2017 | |||
| month = | |||
| doi = 10.1177/2050313X17740513 | |||
| pmid = 29147567 | |||
}}</ref> | |||
*[[Ankle Brachial Index]] < 0.9 is suggestive of [[Peripheral Arterial Disease]]. <ref>{{Cite journal | |||
| author = [[Gurbir Dhaliwal]] & [[Debabrata Mukherjee]] | |||
| title = Peripheral arterial disease: Epidemiology, natural history, diagnosis and treatment | |||
| journal = [[The International journal of angiology : official publication of the International College of Angiology, Inc]] | |||
| volume = 16 | |||
| issue = 2 | |||
| pages = 36–44 | |||
| year = 2007 | |||
| month = Summer | |||
| pmid = 22477268 | |||
}}</ref> | |||
== Treatment == | == Treatment == | ||
=== Medical Therapy === | === Medical Therapy === | ||
*The mainstay of therapy for Aortoilliac disease is surgical. <ref>{{Cite journal | |||
| author = [[Daniel G. Clair]] & [[Jocelyn M. Beach]] | |||
| title = Strategies for managing aortoiliac occlusions: access, treatment and outcomes | |||
| journal = [[Expert review of cardiovascular therapy]] | |||
| volume = 13 | |||
| issue = 5 | |||
| pages = 551–563 | |||
| year = 2015 | |||
| month = May | |||
| doi = 10.1586/14779072.2015.1036741 | |||
| pmid = 25907618 | |||
}}</ref> | |||
*[[Cilastazol]] a [[phosphodiesterase inhibitor]] can be used for symptomatic relief of [[Peripheral Arterial Disease]]. | |||
=== Surgery === | === Surgery === | ||
*Surgical revascularization is the mainstay of therapy for aortoilliac disease. | *[[Surgical revascularization]] is the mainstay of therapy for aortoilliac disease.<ref>{{Cite journal | ||
*Aortofemoral | | author = [[Daniel G. Clair]] & [[Jocelyn M. Beach]] | ||
*[ | | title = Strategies for managing aortoiliac occlusions: access, treatment and outcomes | ||
| journal = [[Expert review of cardiovascular therapy]] | |||
| volume = 13 | |||
| issue = 5 | |||
| pages = 551–563 | |||
| year = 2015 | |||
| month = May | |||
| doi = 10.1586/14779072.2015.1036741 | |||
| pmid = 25907618 | |||
}}</ref> | |||
*Open repair: | |||
**[[Aortofemoral bypass]] with or without [[endarterectomy]] can be used in the treatment of aortoilliac disease.<ref>{{Cite journal | |||
| author = [[Faith Quenzer]], [[Joel Stillings]] & [[Jacqueline Le]] | |||
| title = Dead Legs: A Case of Bilateral Leg Paralysis | |||
| journal = [[Clinical practice and cases in emergency medicine]] | |||
| volume = 1 | |||
| issue = 4 | |||
| pages = 315–318 | |||
| year = 2017 | |||
| month = November | |||
| doi = 10.5811/cpcem.2017.5.34091 | |||
| pmid = 29849356 | |||
}}</ref> <ref>{{Cite journal | |||
| author = [[Miju Bae]], [[Sung Woon Chung]], [[Chung Won Lee]], [[Up Huh]], [[Min Su Kim]] & [[Seung Hwan Song]] | |||
| title = Risk factors associated with postoperative prosthetic graft patency in Leriche syndrome | |||
| journal = [[Asian journal of surgery]] | |||
| volume = 42 | |||
| issue = 1 | |||
| pages = 235–239 | |||
| year = 2019 | |||
| month = January | |||
| doi = 10.1016/j.asjsur.2018.08.009 | |||
| pmid = 30442465 | |||
}}</ref> | |||
*Endovascular Surgery: | |||
**[[Stent]] placement is another treatment option for aortoilliac disease. <ref>{{Cite journal | |||
| author = [[Faith Quenzer]], [[Joel Stillings]] & [[Jacqueline Le]] | |||
| title = Dead Legs: A Case of Bilateral Leg Paralysis | |||
| journal = [[Clinical practice and cases in emergency medicine]] | |||
| volume = 1 | |||
| issue = 4 | |||
| pages = 315–318 | |||
| year = 2017 | |||
| month = November | |||
| doi = 10.5811/cpcem.2017.5.34091 | |||
| pmid = 29849356 | |||
}}</ref> <ref>{{Cite journal | |||
| author = [[Mahmoud Assaad]], [[Sunit Tolia]] & [[Marcel Zughaib]] | |||
| title = Leriche syndrome: The inferior mesenteric artery saves the lower extremity | |||
| journal = [[SAGE open medical case reports]] | |||
| volume = 5 | |||
| pages = 2050313X17740513 | |||
| year = 2017 | |||
| month = | |||
| doi = 10.1177/2050313X17740513 | |||
| pmid = 29147567 | |||
}}</ref> | |||
=== Prevention === | === Prevention === | ||
* | *Effective measures for the primary prevention of [[Peripheral arterial disease]] including aortoilliac disease include: <ref>{{Cite journal | ||
| author = [[Saurabh Aggarwal]], [[Rohit Seth Loomba]] & [[Rohit Arora]] | |||
| title = Preventive aspects in peripheral artery disease | |||
| journal = [[Therapeutic advances in cardiovascular disease]] | |||
| volume = 6 | |||
| issue = 2 | |||
| pages = 53–70 | |||
| year = 2012 | |||
| month = April | |||
| doi = 10.1177/1753944712437359 | |||
| pmid = 22337767 | |||
}}</ref> | |||
**Smoking cessation | |||
** Control of [[hyperlipidemia]], [[Hypertension]], [[Diabetes Mellitus]] | |||
** Low fat diet | |||
**Increase exercise | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
Latest revision as of 04:34, 3 February 2019
Editors-In-Chief: Alexandra Almonacid M.D. [1]and Jeffrey J. Popma M.D. [2]
Overview
Aortoilliac disease also known as Aorotilliac occlusive disease or Leriche Syndrome is a type of Peripheral Arterial Disease (PAD). Peripheral Arterial Disease is caused by occlusion of an artery[1] due to atherosclerotic plaque buildup, thrombosis or embolism. PAD normally affects the distal femoral artery, but Aortoilliac disease is caused by occlusion of the infrarenal aorta and beyond. The Aorta gives off the renal branches at the L1/ L2 spine level and it branches into the Right and Left Common Illiac Arteries at the L4 spine level. Aortoilliac disease can include the Common Illiac arteries and it's branches.[2] Depending on it's underlying cause it can present acutely or chronically. Acute causes include thrombosis and embolism, while chronic causes include atherosclerotic plaque formation
Classification
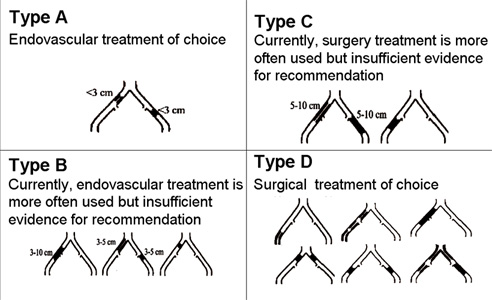
===Morphological Stratification of Iliac Lesions-Trans-Atlantic Intersociety Consensus Classification === [3]
TASC Type A iliac lesions
- Single stenosis less than 3 cm of the CIA or EIA (unilateral/bilateral)
- TASC Type B iliac lesions
- Single stenosis 3 to 10 cm in length, not extending into the CFA
- Total of 2 stenosis less than 5 cm long in the CIA and/or EIA and not extending into the CFA
- Unilateral CIA occlusion
- TASC Type C iliac lesions
- Bilateral 5 to 10 cm long stenosis of the CIA and/or EIA, note extending into the CFA
- Unilateral EIA occlusion not extending into the CFA
- Unilateral EIA stenosis extending into the CFA
- Bilateral CIA occlusion
- TASC Type D iliac lesions
- Diffuse, multiple unilateral stenosis involving the CIA, EIA and CFA (usually more than 10 cm long)
- Unilateral occlusion involving both the CIA and EIA
- Bilateral EIA occlusions
- Diffuse disease involving the aorta and both iliac arteries
- Iliac stenosis in a patient with an abdominal aortic anuerysm or other lesion requiring aortic or iliac surgery
Diagnosis
- MR angiography
- Gadofosveset-enhanced MR angiography showed significant improvement (P < .001) compared with unenhanced MR angiography for diagnosis of clinically significant aortoiliac occlusive disease ( 50% stenosis) .
- The improvement in diagnostic efficacy compared with unenhanced MR angiography was clearly demonstrated. There was an improvement in overall accuracy, sensitivity, and specificity.
- CT Angiography [4] [5]
- CT angiographic examination is less invasive and less expensive than conventional angiography
- Improves resolution with decreased contrast load and acquisition time without increasing radiation exposure
Indications for Revascularization
- Relief of symptomatic lower extremity ischemia, including claudication, rest pain, ulceration or gangrene, or embolization causing blue toe syndrome
- Restoration y/o preservation of inflow to the lower extremity in the setting of pre-existing or anticipated distal bypass
- Procurement of access to more proximal vascular beds for anticipated invasive procedures. Occasionally revascularization is indicated to rescue flow-limiting dissection complicating access for other invasive procedures
Technical Issues
- Endovascular Access
- Ipsilateral femoral artery
- Contralateral femoral artery
- Brachial artery: In patients with flush occlusions at the aortic bifurcation
- Multiple access sites may be required for successful treatment:
- Bilateral femoral
- Femoral/brachial
Treatment Options
PTA
- Endovascular treatment of iliac stenoses
- High technical success rates
- Low morbidity.
- Iliac PTA/stenting
- High rates of patency
- Improvement in functional outcome for the individual patient
- Stent placement
- Balloon expandable stent: Useful in Ostial Lesions
- Greater radial force
- Allow greater precision for placement
- Self-expandable stent
- Longer lesions in which the proximal vessel maybe several millimeters larger than the distal vessel
- Used predominantly in common iliac artery orificial occlusions
- Balloon expandable stent: Useful in Ostial Lesions
Surgical
Complications
- Intraoperative complications
- Dissection
- Extravasation
- Arterial rupture
- Postoperative complications
- Pseudoaneurysm formation at the access site
- Distal embolization
- Hematoma
Prognosis
- Ideal Iliac PTA Lesions
- Stenotic lesion
- Non-calcified
- Discrete (< 3cm)
- Patent run – off vessels (> 2)
- Non- diabetic patients
- Predictors of long-term failure
- Clinical status: CLI vs claudicant
- Smoking
- Women?
- Vessel diameter < 8mm
- Outflow status
- Lack of antiplatelet regimen
- Number of stents
- Occlusion vs. stenosis
Historical Perspective
- Aortoilliac disease/Leriche's syndrome was first described by Dr. Robert Graham, a Scottish surgeon, in 1841.[6][7]
- The symptoms of Aortoillliac disease described together as a syndrome was first discovered by Dr. Rene Leriche a French physician in 1940.[8][9]
- In 1940, Dr. Leriche performed the first surgery to treat Aortoilliac disease/ Leriche syndrome.[10]
Classification
- Aortoilliac disease may be classified according to Trans-Atlantic Intercontinental Consensus guidelines [11] into 4 subtypes/groups:
- TASC Type A iliac lesions
- Single stenosis less than 3 cm of the CIA or EIA (unilateral/bilateral)
- TASC Type B iliac lesions
- Single stenosis 3 to 10 cm in length, not extending into the CFA
- Total of 2 stenosis less than 5 cm long in the CIA and/or EIA and not extending into the CFA
- Unilateral CIA occlusion
- TASC Type C iliac lesions
- Bilateral 5 to 10 cm long stenosis of the CIA and/or EIA, note extending into the CFA
- Unilateral EIA occlusion not extending into the CFA
- Unilateral EIA stenosis extending into the CFA
- Bilateral CIA occlusion
- TASC Type D iliac lesions
- Diffuse, multiple unilateral stenosis involving the CIA, EIA and CFA (usually more than 10 cm long)
- Unilateral occlusion involving both the CIA and EIA
- Bilateral EIA occlusions
- Diffuse disease involving the aorta and both iliac arteries
- Iliac stenosis in a patient with an abdominal aortic anuerysm or other lesion requiring aortic or iliac surgery
Pathophysiology
- The pathogenesis of aortoilliac disease is characterized by atherosclerotic plaque buildup, Thrombosis or an embolus.
- Atherosclerosis is the buildup of cholesterol plaques in the arteries. Damage to the endothelial layer of the vessel wall allows for inflammatory cells, mediators and fatty acids to enter the intimal layer of the artery. Overtime the plaques can enlarge and cause stenosis of the vessel lumen. Thrombosis occurs when a piece of the plaque dislodges and causes an occlusion.
- On gross pathology, cholesterol plaques, fatty streaks, and areas of ulceration and hemorrhage are characteristic findings of atherosclerosis and thrombus formation in aortoilliac disease.[12]
- On microscopic histopathological analysis, foam cells, necrotic core, fibrous cap and inflammatory infiltrate are characteristic findings of atherosclerosis and thrombus formation in aortoilliac disease.[13]
Clinical Features
Clinical features of aortoilliac disease include:
- Claudication of legs and buttocks[14][15]
- Pallor of lower limbs[16]
- Numbness of lower limbs[17]
- Weakness and soreness of lower limbs[18][19]
- Loss of femoral pulses[20]
- Erectile dysfunction [21][22]
- Atrophy of affected muscles in the lower limb[23]
Differentiating Aortoilliac Disease from other Diseases
- Aortoilliac disease must be differentiated from other diseases that cause lower limb claudication, lower limb weakness/atrophy, and loss of femoral pulses such as:
- Peripheral artery disease of the Lower limbs [24]
- Compartment syndrome [25]
- Chronic venous insufficiency
Epidemiology and Demographics
- The prevalence of peripheral arterial disease is approximately 200 million individuals worldwide.[26]
Age
- Aortoilliac disease is more commonly observed among patients aged 30-60 years old.[27]
- Aortoilliac disease is more commonly observed among middle aged and elderly patients.
Gender
- Males are more commonly affected with aortoilliac disease than Females.[28]
Race
- There is no racial predilection for aortoilliac disease.
Risk Factors
- Common risk factors in the development of aortoilliac disease are smoking, diabetes mellitus, dyslipidemia, and hypertension.[29]
Natural History, Complications and Prognosis
- Early clinical features include intermittent claudication, decreased lower limb pulses, and erectile dysfunction.[30]
- If left untreated, patients with aortoilliac disease may progress to develop critical limb ischemia, muscle atrophy, and poor wound healing.[31]
- Prognosis is generally good, and the 5 year mortality rate of patients with peripheral arterial disease as a whole is approximately 33.2%. [32]
Diagnosis
Diagnostic Criteria
- The diagnosis of aortoilliac disease is made when 3 of the following diagnostic criteria are met:
- claudication[33]
- weak lower limb pulses[34]
- erectile dysfunction[35]
Symptoms
- Peripheral arterial disease may start out asymptomatic. Symptoms depend on the arteries affected.
- Symptoms of aortoilliac disease may include the following:
- claudication of lower limbs[36]
- erectile dysfunction[37]
- cold extremities[38]
- weight loss[39]
- pain in buttocks[40]
Physical Examination
- Patients with aortoilliac disease can appear normal or distressed in appearance.
- Physical examination may be remarkable for:
Laboratory Findings
- Laboratory findings consistent with the diagnosis of Peripheral artery disease including aortoilliac disease include abnormal lipid panel [46] and abnormal inflammatory markers.
- Elevated cholesterol
- Elevated LDL
- Elevated ESR
- Elevated CRP[47] [48]
- Elevated homocysteine [49] [50]
Imaging Findings
- CT angiography is the imaging modality of choice for aortoilliac disease.[51]
- On CT angiography, aortoilliac disease is characterized by occlusion of the Common Illiac, External Illiac, or Common Femoral Arteries.[52] [53]
- Doppler Ultrasound may demonstrate decreases blood flow in the Common Illiac, External Illiac, or Common Femoral Arteries. [54] [55]
- Abdominal ultrasound may also be used to aid in diagnosis. [56]
Other Diagnostic Studies
- Peripheral Arterial disease including aortoilliac disease may also be diagnosed using Ankle Brachial Index. [57]
- Ankle Brachial Index < 0.9 is suggestive of Peripheral Arterial Disease. [58]
Treatment
Medical Therapy
- The mainstay of therapy for Aortoilliac disease is surgical. [59]
- Cilastazol a phosphodiesterase inhibitor can be used for symptomatic relief of Peripheral Arterial Disease.
Surgery
- Surgical revascularization is the mainstay of therapy for aortoilliac disease.[60]
- Open repair:
- Aortofemoral bypass with or without endarterectomy can be used in the treatment of aortoilliac disease.[61] [62]
- Endovascular Surgery:
Prevention
- Effective measures for the primary prevention of Peripheral arterial disease including aortoilliac disease include: [65]
- Smoking cessation
- Control of hyperlipidemia, Hypertension, Diabetes Mellitus
- Low fat diet
- Increase exercise
References
- ↑ Edgardo Olvera Lopez & Arif Jan (2018). "Cardiovascular Disease". PMID 30571040. Unknown parameter
|month=ignored (help) - ↑ Candace Wooten, Munawar Hayat, Maira du Plessis, Alper Cesmebasi, Michael Koesterer, Kevin P. Daly, Petru Matusz, R. Shane Tubbs & Marios Loukas (2014). "Anatomical significance in aortoiliac occlusive disease". Clinical anatomy (New York, N.Y.). 27 (8): 1264–1274. doi:10.1002/ca.22444. PMID 25065617. Unknown parameter
|month=ignored (help) - ↑ Michael R. Jaff, Christopher J. White, William R. Hiatt, Gerry R. Fowkes, John Dormandy, Mahmood Razavi, Jim Reekers & Lars Norgren (2015). "An Update on Methods for Revascularization and Expansion of the TASC Lesion Classification to Include Below-the-Knee Arteries: A Supplement to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II): The TASC Steering Comittee(.)". Annals of vascular diseases. 8 (4): 343–357. doi:10.3400/avd.tasc.15-01000. PMID 26730266.
- ↑ Michael R. Jaff, Christopher J. White, William R. Hiatt, Gerry R. Fowkes, John Dormandy, Mahmood Razavi, Jim Reekers & Lars Norgren (2015). "An Update on Methods for Revascularization and Expansion of the TASC Lesion Classification to Include Below-the-Knee Arteries: A Supplement to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II): The TASC Steering Comittee(.)". Annals of vascular diseases. 8 (4): 343–357. doi:10.3400/avd.tasc.15-01000. PMID 26730266.
- ↑ Mahmoud Assaad, Sunit Tolia & Marcel Zughaib (2017). "Leriche syndrome: The inferior mesenteric artery saves the lower extremity". SAGE open medical case reports. 5: 2050313X17740513. doi:10.1177/2050313X17740513. PMID 29147567.
- ↑ W. E. BARNETT, W. W. MOORMAN & B. A. MERRICK (1952). "Thrombotic obliteration of the abdominal aorta: a report of six cases". Annals of internal medicine. 37 (5): 944–965. PMID 12986605. Unknown parameter
|month=ignored (help) - ↑ Wei-Jing Lee, Yung-Ze Cheng & Hung-Jung Lin (2008). "Leriche syndrome". International journal of emergency medicine. 1 (3): 223. doi:10.1007/s12245-008-0039-x. PMID 19384523. Unknown parameter
|month=ignored (help) - ↑ R. Leriche & A. Morel (1948). "The Syndrome of Thrombotic Obliteration of the Aortic Bifurcation". Annals of surgery. 127 (2): 193–206. PMID 17859070. Unknown parameter
|month=ignored (help) - ↑ Wei-Jing Lee, Yung-Ze Cheng & Hung-Jung Lin (2008). "Leriche syndrome". International journal of emergency medicine. 1 (3): 223. doi:10.1007/s12245-008-0039-x. PMID 19384523. Unknown parameter
|month=ignored (help) - ↑ Wei-Jing Lee, Yung-Ze Cheng & Hung-Jung Lin (2008). "Leriche syndrome". International journal of emergency medicine. 1 (3): 223. doi:10.1007/s12245-008-0039-x. PMID 19384523. Unknown parameter
|month=ignored (help) - ↑ Michael R. Jaff, Christopher J. White, William R. Hiatt, Gerry R. Fowkes, John Dormandy, Mahmood Razavi, Jim Reekers & Lars Norgren (2015). "An Update on Methods for Revascularization and Expansion of the TASC Lesion Classification to Include Below-the-Knee Arteries: A Supplement to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II): The TASC Steering Comittee(.)". Annals of vascular diseases. 8 (4): 343–357. doi:10.3400/avd.tasc.15-01000. PMID 26730266.
- ↑ William Jr Insull (2009). "The pathology of atherosclerosis: plaque development and plaque responses to medical treatment". The American journal of medicine. 122 (1 Suppl): S3–S14. doi:10.1016/j.amjmed.2008.10.013. PMID 19110086. Unknown parameter
|month=ignored (help) - ↑ William Jr Insull (2009). "The pathology of atherosclerosis: plaque development and plaque responses to medical treatment". The American journal of medicine. 122 (1 Suppl): S3–S14. doi:10.1016/j.amjmed.2008.10.013. PMID 19110086. Unknown parameter
|month=ignored (help) - ↑ Wei-Jing Lee, Yung-Ze Cheng & Hung-Jung Lin (2008). "Leriche syndrome". International journal of emergency medicine. 1 (3): 223. doi:10.1007/s12245-008-0039-x. PMID 19384523. Unknown parameter
|month=ignored (help) - ↑ Omobolawa Y. Kukoyi, Nicholas Masse & Michael A. Ward (2018). "Man with Bilateral Lower Extremity Weakness". The Journal of emergency medicine. 55 (3): e77–e78. doi:10.1016/j.jemermed.2018.06.007. PMID 30082092. Unknown parameter
|month=ignored (help) - ↑ Wei-Jing Lee, Yung-Ze Cheng & Hung-Jung Lin (2008). "Leriche syndrome". International journal of emergency medicine. 1 (3): 223. doi:10.1007/s12245-008-0039-x. PMID 19384523. Unknown parameter
|month=ignored (help) - ↑ Naomi M. Hamburg & Mark A. Creager (2017). "Pathophysiology of Intermittent Claudication in Peripheral Artery Disease". Circulation journal : official journal of the Japanese Circulation Society. 81 (3): 281–289. doi:10.1253/circj.CJ-16-1286. PMID 28123169. Unknown parameter
|month=ignored (help) - ↑ Wei-Jing Lee, Yung-Ze Cheng & Hung-Jung Lin (2008). "Leriche syndrome". International journal of emergency medicine. 1 (3): 223. doi:10.1007/s12245-008-0039-x. PMID 19384523. Unknown parameter
|month=ignored (help) - ↑ Omobolawa Y. Kukoyi, Nicholas Masse & Michael A. Ward (2018). "Man with Bilateral Lower Extremity Weakness". The Journal of emergency medicine. 55 (3): e77–e78. doi:10.1016/j.jemermed.2018.06.007. PMID 30082092. Unknown parameter
|month=ignored (help) - ↑ Wei-Jing Lee, Yung-Ze Cheng & Hung-Jung Lin (2008). "Leriche syndrome". International journal of emergency medicine. 1 (3): 223. doi:10.1007/s12245-008-0039-x. PMID 19384523. Unknown parameter
|month=ignored (help) - ↑ Wei-Jing Lee, Yung-Ze Cheng & Hung-Jung Lin (2008). "Leriche syndrome". International journal of emergency medicine. 1 (3): 223. doi:10.1007/s12245-008-0039-x. PMID 19384523. Unknown parameter
|month=ignored (help) - ↑ Omobolawa Y. Kukoyi, Nicholas Masse & Michael A. Ward (2018). "Man with Bilateral Lower Extremity Weakness". The Journal of emergency medicine. 55 (3): e77–e78. doi:10.1016/j.jemermed.2018.06.007. PMID 30082092. Unknown parameter
|month=ignored (help) - ↑ Naomi M. Hamburg & Mark A. Creager (2017). "Pathophysiology of Intermittent Claudication in Peripheral Artery Disease". Circulation journal : official journal of the Japanese Circulation Society. 81 (3): 281–289. doi:10.1253/circj.CJ-16-1286. PMID 28123169. Unknown parameter
|month=ignored (help) - ↑ Gurbir Dhaliwal & Debabrata Mukherjee (2007). "Peripheral arterial disease: Epidemiology, natural history, diagnosis and treatment". The International journal of angiology : official publication of the International College of Angiology, Inc. 16 (2): 36–44. PMID 22477268. Unknown parameter
|month=ignored (help) - ↑ Brit Long, Alex Koyfman & Michael Gottlieb (2019). "Evaluation and Management of Acute Compartment Syndrome in the Emergency Department". The Journal of emergency medicine. doi:10.1016/j.jemermed.2018.12.021. PMID 30685220. Unknown parameter
|month=ignored (help) - ↑ F. Gerry R. Fowkes, Victor Aboyans, Freya J. I. Fowkes, Mary M. McDermott, Uchechukwu K. A. Sampson & Michael H. Criqui (2017). "Peripheral artery disease: epidemiology and global perspectives". Nature reviews. Cardiology. 14 (3): 156–170. doi:10.1038/nrcardio.2016.179. PMID 27853158. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ Jaime Caro, Kristen Migliaccio-Walle, Khajak J. Ishak & Irina Proskorovsky (2005). "The morbidity and mortality following a diagnosis of peripheral arterial disease: long-term follow-up of a large database". BMC cardiovascular disorders. 5: 14. doi:10.1186/1471-2261-5-14. PMID 15972099. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ L. Norgren, W. R. Hiatt, J. A. Dormandy, M. R. Nehler, K. A. Harris & F. G. R. Fowkes (2007). "Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)". Journal of vascular surgery. 45 Suppl S: S5–67. doi:10.1016/j.jvs.2006.12.037. PMID 17223489. Unknown parameter
|month=ignored (help) - ↑ Keiichiro Kita (2017). "Leriche syndrome (Aortoiliac occlusive disease)". Journal of general and family medicine. 18 (5): 297–298. doi:10.1002/jgf2.63. PMID 29264049. Unknown parameter
|month=ignored (help) - ↑ Mahmoud Assaad, Sunit Tolia & Marcel Zughaib (2017). "Leriche syndrome: The inferior mesenteric artery saves the lower extremity". SAGE open medical case reports. 5: 2050313X17740513. doi:10.1177/2050313X17740513. PMID 29147567.
- ↑ Mahmoud Assaad, Sunit Tolia & Marcel Zughaib (2017). "Leriche syndrome: The inferior mesenteric artery saves the lower extremity". SAGE open medical case reports. 5: 2050313X17740513. doi:10.1177/2050313X17740513. PMID 29147567.
- ↑ Keiichiro Kita (2017). "Leriche syndrome (Aortoiliac occlusive disease)". Journal of general and family medicine. 18 (5): 297–298. doi:10.1002/jgf2.63. PMID 29264049. Unknown parameter
|month=ignored (help) - ↑ Mahmoud Assaad, Sunit Tolia & Marcel Zughaib (2017). "Leriche syndrome: The inferior mesenteric artery saves the lower extremity". SAGE open medical case reports. 5: 2050313X17740513. doi:10.1177/2050313X17740513. PMID 29147567.
- ↑ Mahmoud Assaad, Sunit Tolia & Marcel Zughaib (2017). "Leriche syndrome: The inferior mesenteric artery saves the lower extremity". SAGE open medical case reports. 5: 2050313X17740513. doi:10.1177/2050313X17740513. PMID 29147567.
- ↑ Mahmoud Assaad, Sunit Tolia & Marcel Zughaib (2017). "Leriche syndrome: The inferior mesenteric artery saves the lower extremity". SAGE open medical case reports. 5: 2050313X17740513. doi:10.1177/2050313X17740513. PMID 29147567.
- ↑ Duane R. Hennion & Kelly A. Siano (2013). "Diagnosis and treatment of peripheral arterial disease". American family physician. 88 (5): 306–310. PMID 24010393. Unknown parameter
|month=ignored (help) - ↑ P. M. Ridker, M. J. Stampfer & N. Rifai (2001). "Novel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease". JAMA. 285 (19): 2481–2485. PMID 11368701. Unknown parameter
|month=ignored (help) - ↑ H. E. Stoffers, A. D. Kester, V. Kaiser, P. E. Rinkens & J. A. Knottnerus (1997). "Diagnostic value of signs and symptoms associated with peripheral arterial occlusive disease seen in general practice: a multivariable approach". Medical decision making : an international journal of the Society for Medical Decision Making. 17 (1): 61–70. doi:10.1177/0272989X9701700107. PMID 8994152. Unknown parameter
|month=ignored (help) - ↑ P. M. Ridker, M. J. Stampfer & N. Rifai (2001). "Novel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease". JAMA. 285 (19): 2481–2485. PMID 11368701. Unknown parameter
|month=ignored (help) - ↑ H. E. Stoffers, A. D. Kester, V. Kaiser, P. E. Rinkens & J. A. Knottnerus (1997). "Diagnostic value of signs and symptoms associated with peripheral arterial occlusive disease seen in general practice: a multivariable approach". Medical decision making : an international journal of the Society for Medical Decision Making. 17 (1): 61–70. doi:10.1177/0272989X9701700107. PMID 8994152. Unknown parameter
|month=ignored (help) - ↑ Daniel G. Clair & Jocelyn M. Beach (2015). "Strategies for managing aortoiliac occlusions: access, treatment and outcomes". Expert review of cardiovascular therapy. 13 (5): 551–563. doi:10.1586/14779072.2015.1036741. PMID 25907618. Unknown parameter
|month=ignored (help) - ↑ Michael R. Jaff, Christopher J. White, William R. Hiatt, Gerry R. Fowkes, John Dormandy, Mahmood Razavi, Jim Reekers & Lars Norgren (2015). "An Update on Methods for Revascularization and Expansion of the TASC Lesion Classification to Include Below-the-Knee Arteries: A Supplement to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II): The TASC Steering Comittee(.)". Annals of vascular diseases. 8 (4): 343–357. doi:10.3400/avd.tasc.15-01000. PMID 26730266.
- ↑ Mahmoud Assaad, Sunit Tolia & Marcel Zughaib (2017). "Leriche syndrome: The inferior mesenteric artery saves the lower extremity". SAGE open medical case reports. 5: 2050313X17740513. doi:10.1177/2050313X17740513. PMID 29147567.
- ↑ S. Karacagil, A. M. Lofberg, B. Almgren, A. Granbo, M. L. Jonsson, L. E. Lorelius & D. Bergqvist (1994). "Duplex ultrasound scanning for diagnosis of aortoiliac and femoropopliteal arterial disease". VASA. Zeitschrift fur Gefasskrankheiten. 23 (4): 325–329. PMID 7817613.
- ↑ Gurbir Dhaliwal & Debabrata Mukherjee (2007). "Peripheral arterial disease: Epidemiology, natural history, diagnosis and treatment". The International journal of angiology : official publication of the International College of Angiology, Inc. 16 (2): 36–44. PMID 22477268. Unknown parameter
|month=ignored (help) - ↑ Mahmoud Assaad, Sunit Tolia & Marcel Zughaib (2017). "Leriche syndrome: The inferior mesenteric artery saves the lower extremity". SAGE open medical case reports. 5: 2050313X17740513. doi:10.1177/2050313X17740513. PMID 29147567.
- ↑ Mahmoud Assaad, Sunit Tolia & Marcel Zughaib (2017). "Leriche syndrome: The inferior mesenteric artery saves the lower extremity". SAGE open medical case reports. 5: 2050313X17740513. doi:10.1177/2050313X17740513. PMID 29147567.
- ↑ Gurbir Dhaliwal & Debabrata Mukherjee (2007). "Peripheral arterial disease: Epidemiology, natural history, diagnosis and treatment". The International journal of angiology : official publication of the International College of Angiology, Inc. 16 (2): 36–44. PMID 22477268. Unknown parameter
|month=ignored (help) - ↑ Daniel G. Clair & Jocelyn M. Beach (2015). "Strategies for managing aortoiliac occlusions: access, treatment and outcomes". Expert review of cardiovascular therapy. 13 (5): 551–563. doi:10.1586/14779072.2015.1036741. PMID 25907618. Unknown parameter
|month=ignored (help) - ↑ Daniel G. Clair & Jocelyn M. Beach (2015). "Strategies for managing aortoiliac occlusions: access, treatment and outcomes". Expert review of cardiovascular therapy. 13 (5): 551–563. doi:10.1586/14779072.2015.1036741. PMID 25907618. Unknown parameter
|month=ignored (help) - ↑ Faith Quenzer, Joel Stillings & Jacqueline Le (2017). "Dead Legs: A Case of Bilateral Leg Paralysis". Clinical practice and cases in emergency medicine. 1 (4): 315–318. doi:10.5811/cpcem.2017.5.34091. PMID 29849356. Unknown parameter
|month=ignored (help) - ↑ Miju Bae, Sung Woon Chung, Chung Won Lee, Up Huh, Min Su Kim & Seung Hwan Song (2019). "Risk factors associated with postoperative prosthetic graft patency in Leriche syndrome". Asian journal of surgery. 42 (1): 235–239. doi:10.1016/j.asjsur.2018.08.009. PMID 30442465. Unknown parameter
|month=ignored (help) - ↑ Faith Quenzer, Joel Stillings & Jacqueline Le (2017). "Dead Legs: A Case of Bilateral Leg Paralysis". Clinical practice and cases in emergency medicine. 1 (4): 315–318. doi:10.5811/cpcem.2017.5.34091. PMID 29849356. Unknown parameter
|month=ignored (help) - ↑ Mahmoud Assaad, Sunit Tolia & Marcel Zughaib (2017). "Leriche syndrome: The inferior mesenteric artery saves the lower extremity". SAGE open medical case reports. 5: 2050313X17740513. doi:10.1177/2050313X17740513. PMID 29147567.
- ↑ Saurabh Aggarwal, Rohit Seth Loomba & Rohit Arora (2012). "Preventive aspects in peripheral artery disease". Therapeutic advances in cardiovascular disease. 6 (2): 53–70. doi:10.1177/1753944712437359. PMID 22337767. Unknown parameter
|month=ignored (help)