Pericarditis resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mugilan Poongkunran M.B.B.S [2]
| Pericarditis Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Synonyms and keywords: Myopericarditis, perimyocarditis
Overview
Pericarditis is the inflammation of the fibroelastic sac surrounding the heart (pericardium). Pericarditis is divided into acute (<6 weeks), subacute (6 weeks to 6 months) and chronic (>6 months) and it can be dry, fibrinous or effusive independently of the etiology. Myopericarditis, or perimyocarditis refers to acute pericarditis associated with myocardial inflammation that leads to global or regional myocardial dysfunction and elevation in the concentration of troponins, creatine kinase MB, myoglobin and tumour necrosis factor.[1] Always suspect pericarditis in the presence of pleuritic chest pain and pericardial friction rub. NSAIDs are the mainstay of the treatment of acute pericarditis; ibuprofen is the most preferred drug due to its favorable effect on the coronary flow.[2]
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
- Autoimmune: Rheumatoid arthritis, Sjögren’s syndrome, SLE, systemic sclerosis, systemic vasculitis
- Bacterial: Coxiella burnetii, pneumococcus, staphylococcus, streptococcus, tuberculosis[3]
- Cardiovascular: Dressler's syndrome, postpericardiotomy syndrome, post-traumatic pericarditis[4]
- Idiopathic
- Metabolic: Myxedema, uremia
- Neoplastic: Breast cancer, leukemia, lung cancer, lymphoma
- Viral: Adenovirus, CMV, coxsackie, EBV, echovirus, HBV, HIV, human herpes virus 6, influenza, mumps, parvovirus B19, rubella, varicella[3]
Diagnosis
Shown below is an algorithm summarizing the diagnostic approach to acute pericarditis in adults.[2][5][4]
|
Click on boxes to expand/collapse detailed information.
|
Characterize the symptoms
Symptoms associated with pericardial effusion:
❑ With a hemodynamically significant pericardial effusion
Other etiology associated symptoms: Obtain a detailed history❑ Infections
❑ Systemic illness ❑ Others Examine the patientVital signs
Cardiovascular system Auscultation
❑ Murmur (in concomitant heart disease)
Palpation
Percussion Respiratory system ❑ Wheeze or rales Abdomen ❑ Pulsatile hepatomegaly (in constrictive pericarditis) Order tests (urgent)Order laboratory tests (urgent): ❑ CBC (leucocytosis) Order electrocardiogram (urgent): ❑ Typical findings in pericarditis
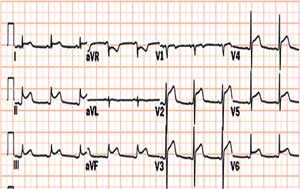 ❑ Electrical alternans (in cardiac tamponade) Order imaging (urgent):

Does the patient have at least two of the following criteria for the diagnosis of acute pericarditis?❑ Characteristic chest pain
❑ Suggestive ECG changes
❑ Suggestive echocardiography changes
Does the patient have any sign of myocarditis?❑ Elevated cardiac enzymes, or Does the patient have any signs suspicious of acute pericarditis?❑ Ongoing fever | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
Treatment of Acute Pericarditis
Shown below is an algorithm summarizing the management of acute pericarditis in adults.[2][5][4]
|
Click on boxes to expand/collapse detailed information.
|
Does the patient have high risk features?High risk features include: ManagementInitiate medical therapy
Administer Aspirin
❑ Stop anticoagulants if patient develops pericardial effusion
Administer Colchicine
Order tests to identify the specific etiology Order pericardiocentesis in case of
ManagementTreat cardiac tamponade Initiate medical therapy
Administer aspirin
❑ Stop anticoagulants if patient develops pericardial effusion
Administer colchicine
Order tests to identify the specific etiology ManagementInitiate medical therapy
Colchicine Administer gastroprotective agents
Avoid steroids Educate about life style modification ❑ In case of pericarditis, avoid sternous physical activity until symptom resolution
ManagementIntitate medical therapy ❑ Administer High-dose aspirin
❑ Administer gastroprotective agents
❑ Stop anticoagulants if patient develops pericardial effusion Life style modification
Follow up as outpatient❑ Observe for recurrences or constriction Admit to the hospital❑ Indication that the underlying cause may not be viral or idiopathic in nature.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment of Recurrent Pericarditis
Shown below is an algorithm summarizing the management of recurrent pericarditis in adults which encompass the incessant type (relapses on discontinuation of anti-inflammatory) and the intermittent type (widely varying symptom free interval without medical therapy).[2][5][4]
| Recurrent pericarditis | |||||||||||||||||||||||||||||||||||||||||||||||||
Characterize the clinical, EKG and imaging findings ❑ Characteristic acute pericarditis symptoms
| |||||||||||||||||||||||||||||||||||||||||||||||||
Initiate medical therapy NSAIDs
❑ Indomethacin:
Aspirin
❑ Stop anticoagulants if patient develops pericardial effusion
Colchicine:
Life style modification ❑ Excercise restriction until symptom resolution | |||||||||||||||||||||||||||||||||||||||||||||||||
| Multiple relapses | |||||||||||||||||||||||||||||||||||||||||||||||||
| Positive response | No response | ||||||||||||||||||||||||||||||||||||||||||||||||
Taper steroids ❑ Taper dose over a three-month period
❑ Add colchicine or NSAIDs at the end of tapering of steroids | ❑ Add azathioprine (75–100 mg/day) or cyclophosphamide | ||||||||||||||||||||||||||||||||||||||||||||||||
| Treatment failure | |||||||||||||||||||||||||||||||||||||||||||||||||
Pericardiectomy ❑ Maintain the patient on steroid free regimen for several weeks before the procedure ❑ Order tests to identify the specific etiology and treat accordingly | |||||||||||||||||||||||||||||||||||||||||||||||||
Etiology Specific Management
| Clinical subgroups | Specific investigations | Treatment |
|---|---|---|
| Viral pericarditis | ❑ Perform testing for viral etiologies in immunocompromised and HIV infected patients not responding to intial management ❑ Diagnostic pericardiocentesis ❑ Analysis of pericardial fluid (transudate or exudate) ❑ PCR or in-situ hybridisation |
❑ CMV pericarditis: Hyperimmunoglobulin OD 4 ml/kg on day 0, 4,and 8; 2 ml/kg on day 12 and 16 ❑ Coxsackie B pericarditis: Interferon alpha or beta 2,5 Mio. IU/m2 surface area s.c. 3 x per week ❑ Adenovirus and parvovirus B19 perimyocarditis: Immunoglobulin 10 g IV at day 1 and 3 for 6-8 hours |
| Purulent pericarditis | ❑ Diagnostic pericardiocentesis in cases of high clinical suspicion ❑ Gram stain, acid fast stain, fungal stain, and cultures of the pericardial fluid ❑ Protein, glucose and cell count of the pericardial fluid ❑ Gram stain, acid fast stain, fungal stain, and cultures of other body fluids |
❑ Therapeutic pericardiocentesis or pericardial window ❑ Pericardiectomy may be used in treatment of recurrent pericardial effusion and in patients with dense adhesions, loculated and thick purulent effusion ❑ Antimicrobial therapy in case of bacterial etiology ❑ Intiate antistaphylococcal antibiotic plus aminoglycoside, followed by tailored antibiotic therapy according to pericardial fluid and blood cultures ❑ Empiric regimen can be started for the following ❑ Immunosuppression ❑ Concurrent infection at another body site ❑ Presence of intravascular lines or prosthetic devices ❑ Recent antimicrobial therapy ❑ Antifungal therapy in case of fungal etiology |
| Tuberculous pericarditis | ❑ Diagnostic pericardiocentesis in all suspected tuberculous pericarditis patients ❑ PCR of pericardial fluid ❑ High adenosine deaminase activity and interferon gamma concentration in pericardial effusion ❑ Pericardial biopsy (rapid diagnosis) ❑ Tuberculin skin test (not helpful) ❑ CT scan and/or MRI of the chest ❑ Culture of sputum, gastric aspirate, and/or urine ❑ Enzyme-linked immunospot (ELISPOT) ❑ Serum titres of antimyolemmal and antimyosin antibodies |
❑Anti-tuberculosis chemotherapy ❑ Emperic therapy in TB endemic areas and in cases with high clinical suspicion ❑ Pericardiectomy is warranted in the setting of persistent constrictive pericarditis or when no general improvement after 4-8 weeks following antituberculosis chemotherapy ❑ Prednisone can be used. |
| Neoplastic pericarditis | ❑ CT scan and/or MRI of the chest ❑ Diagnostic pericardiocentesis when other tests couldnt identify malignancy ❑ Cytology and tumour markers ❑ Pericardial biopsy |
❑ Systemic antineoplastic treatment ❑ Assess the life expectancy of the patients before proceeding with the treatment ❑ Better prognosis patients should be treated more aggressively ❑ Advanced malignancy should be treated palliatively with pericardiocentesis ❑ Recurrence of pericardial effusion is prevented using any of the following techniques ❑ Prolonged pericardiocentesis ❑ Pericardial sclerosis ❑ Pericardiotomy ❑ Intrapericardial chemotherapy |
| Pericarditis in renal failure | ❑ Renal function test ❑ Diagnostic pericardiocentesis ❑ Pericardial biopsy |
❑ Uremic pericarditis ❑ Hemodialysis or peritoneal dialysis ❑ Heparin-free haemodialysis should be used ❑ Dialysis-associated pericarditis ❑ Pericardiocentesis for large effusion ❑ Pericardiotomy in non resolving effusion |
| Pericarditis in systemic autoimmune disease | ❑ Diagnostic pericardiocentesis ❑ Elevated lymphocytes and mononuclear cells > 5000/mm3 ❑ Antisarcolemmal antibodies ❑ Exclusion of viral and bacterial etiologies |
❑ NSAIDs or aspirin or colchicine ❑ Systemic corticosteroid can be used ❑ Intrapericardial steroids has less side effects and is highly effective |
Do's
- Always suspect acute pericarditis in the presence of characteristic pleuritic chest pain and pericardial friction rub. Also suspect pericarditis in a patient with persistent fever and pericardial effusion or new unexplained cardiomegaly.
- Exclude significant effusion and cardiac tamponade. Suspect acute cardiac tamponade in any patient presenting with Beck's triad: hypotension, muffled heart sounds and distended neck veins (or elevated jugular venous pressure).[9]
- Heparin is recommended under strict observation for patients who need anticoagulant therapy.
- Restrict systemic corticosteroid therapy to connective tissue diseases, autoreactive or uremic pericarditis. Use intrapericardial application to avoid systemic side effects. Use moderate initial dosing of steroids followed by a slow taper. Introduce ibuprofen or colchicine early during tapering of steroids.
- Order an analysis of pericardial effusion for different etiologies according to the clinical presentation.
- Assess for the presence of coagulopathy or the intake of antithrombotic medications before choosing the modality of drainage of the pericardial fluid.
- Choose pericardiocentesis rather than surgical drainage as a therapeutic option unless the patient has an indication for surgical drainage. Consider surgical drainage in aortic dissection and myocardial rupture.[10]
- When surgical drainage is indicated but the patient has severe hypotension prohibiting the induction of anesthesia, perform pericardiocentesis in the operating room before surgery.[10]
- Monitor closely patients who underwent pericardiocentesis for postdrainage decompensation.
Don'ts
- When cardiac tamponade is suspected, do not delay its treatment.
- Avoid pericardiocentesis in cases where the diagnosis can be made based on systemic features or when the effusions are very small or resolving with anti-inflammatory treatment.
- Don't perform pericardiocentesis in aortic dissection and ruptured ventricular aneurysm and avoid it in cases of uncorrected coagulopathy, anticoagulant therapy, thrombocytopenia < 50,000/mm 3 , small, posterior, and loculated effusions.
References
- ↑ Imazio M (2012). "Contemporary management of pericardial diseases". Curr Opin Cardiol. 27 (3): 308–17. doi:10.1097/HCO.0b013e3283524fbe. PMID 22450720.
- ↑ 2.0 2.1 2.2 2.3 Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y; et al. (2004). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology". Eur Heart J. 25 (7): 587–610. doi:10.1016/j.ehj.2004.02.002. PMID 15120056.
- ↑ 3.0 3.1 Imazio M, Spodick DH, Brucato A, Trinchero R, Adler Y (2010). "Controversial issues in the management of pericardial diseases". Circulation. 121 (7): 916–28. doi:10.1161/CIRCULATIONAHA.108.844753. PMID 20177006.
- ↑ 4.0 4.1 4.2 4.3 Lange RA, Hillis LD (2004). "Clinical practice. Acute pericarditis". N Engl J Med. 351 (21): 2195–202. doi:10.1056/NEJMcp041997. PMID 15548780.
- ↑ 5.0 5.1 5.2 Klein AL, Abbara S, Agler DA, Appleton CP, Asher CR, Hoit B; et al. (2013). "American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography". J Am Soc Echocardiogr. 26 (9): 965–1012.e15. doi:10.1016/j.echo.2013.06.023. PMID 23998693.
- ↑ Khandaker MH, Espinosa RE, Nishimura RA; et al. (2010). "Pericardial disease: diagnosis and management". Mayo Clinic Proceedings. Mayo Clinic. 85 (6): 572–93. doi:10.4065/mcp.2010.0046. PMC 2878263. PMID 20511488. Unknown parameter
|month=ignored (help) - ↑ "WHO launches World health report 2013". Euro Surveill. 18 (33): 20559. 2013. PMID 23968879.
- ↑ 8.0 8.1 8.2 8.3 Goldfinger S (2014). "A randomized trial of colchicine for acute pericarditis". N Engl J Med. 370 (8): 780. doi:10.1056/NEJMc1315351#SA1. PMID 24552334.
- ↑ Sternbach, G.; Beck, C. "Claude Beck: cardiac compression triads". J Emerg Med. 6 (5): 417–9. PMID 3066820.
- ↑ 10.0 10.1 Schiavone WA (2013). "Cardiac tamponade: 12 pearls in diagnosis and management". Cleve Clin J Med. 80 (2): 109–16. doi:10.3949/ccjm.80a.12052. PMID 23376916.