Relapsing fever laboratory tests
|
Relapsing fever Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Relapsing fever laboratory tests On the Web |
|
American Roentgen Ray Society Images of Relapsing fever laboratory tests |
|
Risk calculators and risk factors for Relapsing fever laboratory tests |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Laboratory Findings
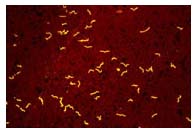
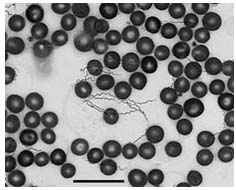
- The definitive diagnosis of TBRF is based on the observation of Borrelia spirochetes in smears of peripheral blood, bone marrow, or cerebrospinal fluid in a symptomatic person. Although best visualized by dark field microscopy, the organisms can also be detected by Wright-Giemsa or acridine orange-stained preparations.
- The organisms are best detected in blood obtained while a person is febrile. With subsequent febrile episodes, the number of circulating spirochetes decreases, making it harder to detect spirochetes on a peripheral blood smear. Even during the initial episode spirochetes will only be seen 70% of the time.
Blood samples obtained before antibiotic treatment can be cultured using BSK medium or by inoculating immature mice. The spirochete will usually be evident within 24 hours if the blood was drawn during a febrile episode.
Although not valuable for making an immediate diagnosis, serologic testing is available through public health laboratories and some private laboratories. Acute serum should be taken within 7 days of symptom onset and convalescent serum should be taken at least 21 days after symptoms start. Early antibiotic treatment may blunt the antibody response and the antibody levels may wane quickly during the months after exposure. To confirm the diagnosis of TBRF, Borrelia specific antibody titers should be increased between acute and convalescent serum samples and convalescent serum antibody levels should be at least two standard deviations above pooled negative controls. Serologic testing for TBRF is not standardized and results may vary by lab. Patients with TBRF may have false-positive tests for Lyme disease because of the similarity of proteins between the two organisms.
Incidental laboratory findings include normal to increased white blood cell count with a left shift towards immature cells, a mildly increased serum bilirubin level, mild to moderate thrombocytopenia (low platelet count), elevated ESR and slightly prolonged coagulation tests, PT and APTT.