Varicose veins pathophysiology
|
Varicose veins Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Varicose veins pathophysiology On the Web |
|
American Roentgen Ray Society Images of Varicose veins pathophysiology |
|
Risk calculators and risk factors for Varicose veins pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
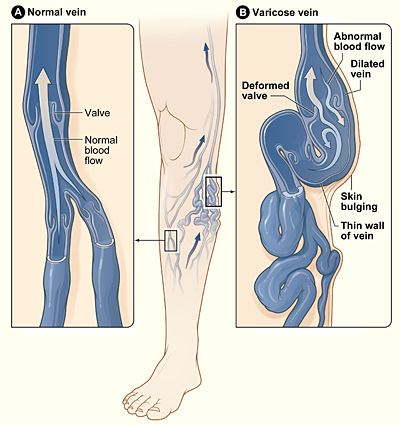
Varicose veins are normal veins that have become dilated beyond 3mm. They usually occur in lower limbs. The superficial and deep veins are connected by perforating veins (also have valves), which also prevent the backflow of blood from deep to superficial veins. Due to obesity, pregnancy, intra-abdominal mass, post-thrombotic destruction of the perforating veins' valves, etc. sustained high pressures can develop in superficial veins. This causes dilation of superficial veins and the development of varicose veins over time. If unattended, they worsen over time and might be associated with pain, discomfort, localized dermatitis, discoloration, and/or ulceration. Because of slowed blood flow, they can also be associated with the formation of blood clots in the dilated veins.
Pathogenesis
Varicose veins originate from sustained raised blood pressure in the superficial veins. Veins are normally gated by a one-way bicuspid valve system that prevents the backward flow of blood. The venous system of limbs is divided by fascia into two sub-systems- Superficial veins and Deep veins. These two venous systems are connected intermittently by perforating veins that travel across fascia. The deep veins are a high-pressure system supported by muscle and deep fascia, which prevent abnormal dilatation of these veins. Additionally, the muscles surrounding the deep veins help in pumping blood towards the heart. The one-way valves and the negative pressure generated by the emptying of deep veins help the blood in superficial veins flow into the deep veins via the perforant/perforating collateral veins[1]. The superficial veins are not supported by fascia. The valves in perforating collateral veins allow blood to flow from superficial to deep veins only. They inhibit backward blood flow from deep to superficial veins. Even though the pressure inside them is low, they are prone to dilation when exposed to high pressure.
The pathogenesis of varicose veins is multifactorial. Most of the risk factors for varicose veins either cause the weakening/destruction of valves of perforating veins or cause raise the overall pressure in the veins. There are several risk factors for varicose veins[2]:
- Age: With advancing age, the valves of the veins are exposed to wear and tear. This can lead to the development of the incompetence of the one-way valves[3] that regulate the venous blood flow. This leads to backward leaking of pressure from deep veins to the superficial veins. This leads to increased prevalence of varicose veins in the elderly.
- Sex: It has been found that females are more prone to develop varicose veins. It has been hypothesized that estrogen plays are role in this. Estrogen caused increased relaxation of veins, limiting proper closure of the valves[4]. Varicose portions of veins often have higher density of estrogen receptors when compared with non-varicose portions of the veins[5]. Oral contraceptive pills may increase the chances of varicose veins.
- Pregnancy: During pregnancy, several physiologic changes occur. These changes help make sure that the fetus gets proper nutrition and increase the chances of its survival. The expansion of intravascular blood volume is one of these changes. Previous pregnancies have been found to be an independent risk factor for varicose veins in women[6]. Hormonal changes of pregnancy also play a role in this predispostion.
- Family history: Positive family history is present in a lot of cases varicose veins. The association seems to be more with prevalence rather than incidence[7]. In 2019, a genetic makeup study for varicose veins' patients revealed that most patients shared a host of abnormal genes that are responsible for angiogenesis[8]. This might help in development of new therapies targeting these genes.
- Obesity: Obese patients have been to be associated with significantly higher CEAP clinical stages as compared to non-obese patients even in people with similar anatomical patterns of venous incompetence[9]. The obese patients were observed to have significantly more saphenofemoral reflux[10].
- Prolonged standing: People in prolonged hours of standing tend to develop Varicose veins. Prolonged standing can raise the venous pressure in the legs.
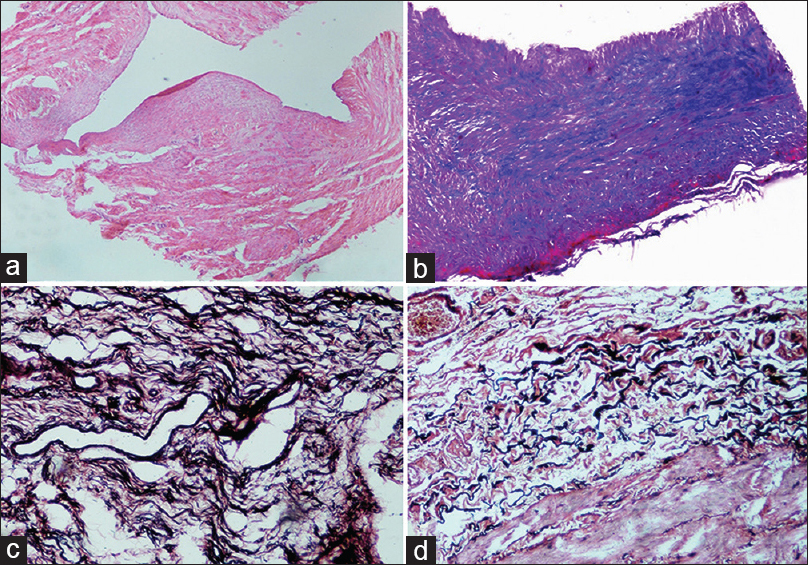
Gross pathology
Varicose Veins have a tortuous, beady appearance on gross examination.

Microscopic pathology
References
- ↑ Meissner MH (2005). "Lower extremity venous anatomy". Semin Intervent Radiol. 22 (3): 147–56. doi:10.1055/s-2005-921948. PMC 3036282. PMID 21326687.
- ↑ https://www.mayoclinic.org/diseases-conditions/varicose-veins/symptoms-causes/syc-20350643
- ↑ van Langevelde K, Srámek A, Rosendaal FR (2010). "The effect of aging on venous valves". Arterioscler Thromb Vasc Biol. 30 (10): 2075–80. doi:10.1161/ATVBAHA.110.209049. PMID 20671232.
- ↑ Raffetto JD, Qiao X, Beauregard KG, Khalil RA (2010). "Estrogen receptor-mediated enhancement of venous relaxation in female rat: implications in sex-related differences in varicose veins". J Vasc Surg. 51 (4): 972–81. doi:10.1016/j.jvs.2009.11.074. PMC 2847594. PMID 20347696.
- ↑ Mashiah A, Berman V, Thole HH, Rose SS, Pasik S, Schwarz H; et al. (1999). "Estrogen and progesterone receptors in normal and varicose saphenous veins". Cardiovasc Surg. 7 (3): 327–31. doi:10.1016/s0967-2109(98)00132-x. PMID 10386751.
- ↑ Krasiński Z, Sajdak S, Staniszewski R, Dzieciuchowicz L, Szpurek D, Krasińska B; et al. (2006). "[Pregnancy as a risk factor in development of varicose veins in women]". Ginekol Pol. 77 (6): 441–9. PMID 16964695.
- ↑ Ahti TM, Mäkivaara LA, Luukkaala T, Hakama M, Laurikka JO (2009). "Effect of family history on the incidence of varicose veins: a population-based follow-up study in Finland". Angiology. 60 (4): 487–91. doi:10.1177/0003319709335510. PMID 19625267.
- ↑ Shadrina AS, Sharapov SZ, Shashkova TI, Tsepilov YA (2019). "Varicose veins of lower extremities: Insights from the first large-scale genetic study". PLoS Genet. 15 (4): e1008110. doi:10.1371/journal.pgen.1008110. PMC 6490943. PMID 30998689.
- ↑ van Rij AM, De Alwis CS, Jiang P, Christie RA, Hill GB, Dutton SJ; et al. (2008). "Obesity and impaired venous function". Eur J Vasc Endovasc Surg. 35 (6): 739–44. doi:10.1016/j.ejvs.2008.01.006. PMID 18313335.
- ↑ Mahapatra S, Ramakrishna P, Gupta B, Anusha A, Para MA (2018). "Correlation of obesity & comorbid conditions with chronic venous insufficiency: Results of a single-centre study". Indian J Med Res. 147 (5): 471–476. doi:10.4103/ijmr.IJMR_1844_16. PMC 6094506. PMID 30082571.
- ↑ "Varicose Veins". https://teachmesurgery.com/vascular/venous/varicose-veins/. External link in
|website=(help) - ↑ https://peir.path.uab.edu/wiki/Main_Page
- ↑ Naik B, Kumar M, Khanna AK, Suman PK. Clinico-histopathological study of varicose vein and role of matrix metalloproteinases-1, matrix metalloproteinases-9 and tissue inhibitor of matrix metalloproteinase-1 in varicose vein formation. Indian J Pathol Microbiol [serial online] 2016 [cited 2020 Jul 10];59:25-30. Available from: http://www.ijpmonline.org/text.asp?2016/59/1/25/178217