COVID-19-associated diabetes mellitus
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Tayyaba Ali, M.D.[2]
Synonyms and keywords: New-onset Diabetes in COVID-19 Islet cell injury by SARS-CoV 2
Overview
Historical Perspective
- Diabetes mellitus is defined by insulin deficiency due to either diminished insulin release or end-organ insulin resistance.[1]
- Diabetes is an umbrella term for conditions such as type I (T1DM) and type II (T2DM) diabetes mellitus, gestational diabetes, and maturity-onset diabetes of the young (MODY).[1]
- Type 1 Diabetes Mellitus is caused by pancreatic β-cell failure or auto-immune destruction of the pancreatic β-cells. It generally presents in children and young adults.[1]
- Type 2 Diabetes Mellitus (T2DM) is defined by insulin resistance and presents in adults. Family history, hypertension, obesity, and dyslipidemia play a significant role in causing T2DM.[1]
- Around 422 million individuals worldwide have diabetes, the dominant part living in low-and middle-income nations, and 1.6 million deaths are straightforwardly credited to diabetes every year. In the course of recent decades, a consistent rise has been observed in both the incidence and the prevalence.[2]
- In China, in the year 2008, a study was done in which they compared 39 SARS-CoV patients with no previous history of diabetes, who never used steroids, with 39 matched healthy siblings.The results of the study revealed that 20 out of 39 SARS-CoV patients developed new-onset diabetes during the hospital stay. After 3 years of recovery from the SARS-CoV infection, only 5% of patients remained diabetic whereas blood sugar levels normalized in the rest of the patients with the infection recovery.[3]
- ACE2 is the primary receptor For SARS-CoV spike protein. SARS-CoV causes infection by binding to ACE2 receptors on the target cells.[4][5] The study suggested, SARS-CoV may damage islets and cause acute insulin dependent diabetes mellitus.[3]
Classification
There is no established system for the classification of [disease name].
OR
[Disease name] may be classified according to [classification method] into [number] subtypes/groups: [group1], [group2], [group3], and [group4].
OR
[Disease name] may be classified into [large number > 6] subtypes based on [classification method 1], [classification method 2], and [classification method 3]. [Disease name] may be classified into several subtypes based on [classification method 1], [classification method 2], and [classification method 3].
OR
Based on the duration of symptoms, [disease name] may be classified as either acute or chronic.
OR
If the staging system involves specific and characteristic findings and features: According to the [staging system + reference], there are [number] stages of [malignancy name] based on the [finding1], [finding2], and [finding3]. Each stage is assigned a [letter/number1] and a [letter/number2] that designate the [feature1] and [feature2].
OR
The staging of [malignancy name] is based on the [staging system].
OR
There is no established system for the staging of [malignancy name].
Pathophysiology
- Angiotensin-converting enzyme 2 (ACE2) receptors expressed in the tissues that are highly involved in body metabolism. These tissues comprise of pancreatic beta cells, adipose tissue, small intestine, and the kidneys. ACE2 receptors in the endocrine pancreas serve the entrance for Severe acute respiratory syndrome coronavirus 2 (SARS-CoV 2), which causes Corononavirus Disease 2019 (COVID-19). [6]
- Expression of ACE2 receptors and effector protease TMPRSS2 in pancreas are associated with SARS-CoV 2 infection.[7]
- The pancreas consists of nine different cell types such as acinar cells, ductal cells, beta cells, alpha cells, mesenchymal cells, and endothelial cells. These pancreatic cells express both ACE2 and TMPRSS2. The expression of ACE2 in pancreatic alpha and beta cells is further proved by immunohistochemistry. Both beta cells that secrete insulin and alpha cells that secrete glucagon, stained positive for SARS-CoV 2 Spike protein and thus, it is postulated that SARS-CoV 2 can infect pancreatic islet cells.[7]
- A recent experiement was conducted to study SARS-CoV 2 tropism that is the cellular response to an external stimulus in human cells and organoids. Researchers infect human pluripotent stem cells (hPSC)-derived pancreatic endocrine cells with SARS-CoV 2.[8]
- Researchers found when SARS-CoV 2 infect pancreatic cells, it downregulates the pathways including calcium signaling pathways, glucagon signaling pathways of alpha cells, and metabolic pathways that assist in insulin secretion from pancreatic beta cells.[8]
- Researchers further stained SARS-CoV 2 infected hPSC-derived pancreatic endocrine cells with a cell apoptotic marker (CASP3). As a result of this staining, they found a large number of CASP3 cells in infected hPSC-derived pancreatic cells. This indicates that change in metabolic pathways of the pancreas is mainly due to cell apoptosis, trigger by SARS-CoV 2. This experiment suggest that when SARS-CoV 2 binds to ACE2 in Pancreas, this will upregulate the genes responsible for apoptosis and downregulate the genes responsible for the cell survival. [8]
- ACE2 is the target receptor for both SARS-CoV and SARS-CoV 2. Researchers in China observed new-onset diabetes among SARS-CoV patients. Therefore in agreement with this, the SARS-CoV 2 might enter pancreatic islets through binding to ACE2, and cause acute β-cell injury, leading to intense hyperglycemia and transient Type 2 Diabetes Mellitus.[3]
- ACE2 serves as the negative regulator of the Renin-Angiotensin System (RAS) mainly by converting Ang (angiotensin) I and Ang II into Ang 1-9 and Ang 1-7, respectively.[9][10] When SARS-CoV and Sars-CoV 2 bind to ACE2 receptors, this will lead to the subsequent downregulation of surface ACE2 expression.[5][11][12]SARS-CoV 2 differs from SARS-CoV by 380 amino acid substitutions and thus has a stronger binding affinity than SARS-CoV, which explains the global impact of SARS-CoV 2 than the previous SARS-CoV outbreak.[13][14]
- ACE2 is the negative regulator of the Renin-Angiotensin system (RAS) and has protective benefits against many diseases and complications. SARS-CoV 2 binds to ACE2 receptors, this blocks all the protective benefits of the ACE2 pathway and shifts the cascade back to ACE/Ang II/AT1R-pathway, increasing Ang II, decreasing ACE2 and Ang-( 1-7)[15] as shown in the figure.
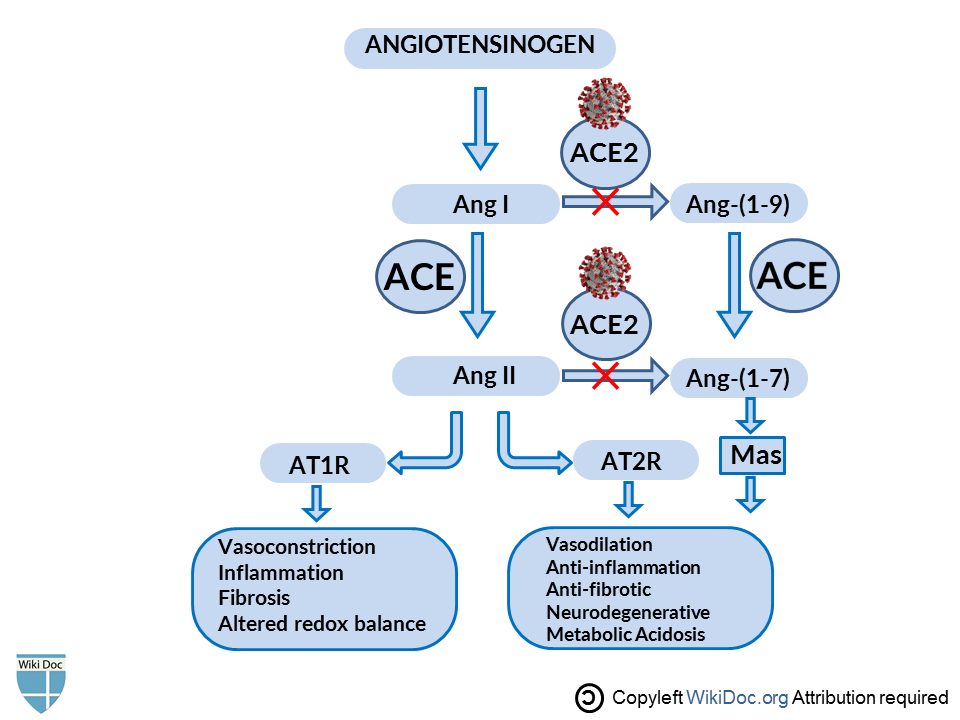
- Inhibition of RAS(Angiotensin→Ang1→Ang2) protects pancreatic β-cells from oxidative stress-related tissue damage, therefore improves insulin synthesis and secretion.[16]Hyperactivity of RAS works in contrast. In adipose tissue, Ras decreases insulin sensitivity, decreases glucose uptake. In pancreatic tissue, it decreases insulin secretion, increases islet oxidative stress and fibrosis, decrease perfusion.[17]
- In an experimental trial, pressor doses of Ang-II were given to healthy human subjects. As a result, researchers observed suppression of basal, pulsatile, and glucose-stimulated insulin release.[18]This loss of insulin release is supposed to be the contributing factor in the development of T2DM.[19]
Causes
Disease name] may be caused by [cause1], [cause2], or [cause3].
OR
Common causes of [disease] include [cause1], [cause2], and [cause3].
OR
The most common cause of [disease name] is [cause 1]. Less common causes of [disease name] include [cause 2], [cause 3], and [cause 4].
OR
The cause of [disease name] has not been identified. To review risk factors for the development of [disease name], click here.
Epidemiology and Demographics
Risk Factors
There are no established risk factors for [disease name].
OR
The most potent risk factor in the development of [disease name] is [risk factor 1]. Other risk factors include [risk factor 2], [risk factor 3], and [risk factor 4].
OR
Common risk factors in the development of [disease name] include [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4].
OR
Common risk factors in the development of [disease name] may be occupational, environmental, genetic, and viral.
Screening
There is insufficient evidence to recommend routine screening for [disease/malignancy].
OR
According to the [guideline name], screening for [disease name] is not recommended.
OR
According to the [guideline name], screening for [disease name] by [test 1] is recommended every [duration] among patients with [condition 1], [condition 2], and [condition 3].
Natural History, Complications, and Prognosis
If left untreated, [#]% of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
OR
Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
OR
Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%.
Diagnosis
History and Symptoms
According to a recent case reported of Diabetic ketoacidoses precipitated by Covid-19 in a patient with newly diagnosed diabetes mellitus. He was a previously healthy man presented with 1-week history of:
- Fever (38.5 °C)
- Vomiting,
- Polydipsia (intense thirst)
- Polyuria (production of abnormally large volumes of dilute urine)[20]
Physical Examination
- Mildly tachycardic
- Kusmmaul's breathing was not observed.[20]
Laboratory Findings
- Hyperglycemia
- High anion gap metabolic acidosis
- Ketonemia [20]
Electrocardiogram
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
There is no treatment for [disease name]; the mainstay of therapy is supportive care.
OR
Supportive therapy for [disease name] includes [therapy 1], [therapy 2], and [therapy 3].
OR
The majority of cases of [disease name] are self-limited and require only supportive care.
OR
[Disease name] is a medical emergency and requires prompt treatment.
OR
The mainstay of treatment for [disease name] is [therapy].
OR The optimal therapy for [malignancy name] depends on the stage at diagnosis.
OR
[Therapy] is recommended among all patients who develop [disease name].
OR
Pharmacologic medical therapy is recommended among patients with [disease subclass 1], [disease subclass 2], and [disease subclass 3].
OR
Pharmacologic medical therapies for [disease name] include (either) [therapy 1], [therapy 2], and/or [therapy 3].
OR
Empiric therapy for [disease name] depends on [disease factor 1] and [disease factor 2].
OR
Patients with [disease subclass 1] are treated with [therapy 1], whereas patients with [disease subclass 2] are treated with [therapy 2].
Surgery
Surgical intervention is not recommended for the management of [disease name].
OR
Surgery is not the first-line treatment option for patients with [disease name]. Surgery is usually reserved for patients with either [indication 1], [indication 2], and [indication 3]
OR
The mainstay of treatment for [disease name] is medical therapy. Surgery is usually reserved for patients with either [indication 1], [indication 2], and/or [indication 3].
OR
The feasibility of surgery depends on the stage of [malignancy] at diagnosis.
OR
Surgery is the mainstay of treatment for [disease or malignancy].
Primary Prevention
There are no established measures for the primary prevention of [disease name].
OR
There are no available vaccines against [disease name].
OR
Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
OR
[Vaccine name] vaccine is recommended for [patient population] to prevent [disease name]. Other primary prevention strategies include [strategy 1], [strategy 2], and [strategy 3].
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
OR
Effective measures for the secondary prevention of [disease name] include [strategy 1], [strategy 2], and [strategy 3].
References
- ↑ 1.0 1.1 1.2 1.3 King, H.; Aubert, R. E.; Herman, W. H. (1998). "Global Burden of Diabetes, 1995-2025: Prevalence, numerical estimates, and projections". Diabetes Care. 21 (9): 1414–1431. doi:10.2337/diacare.21.9.1414. ISSN 0149-5992.
- ↑ "Diabetes".
- ↑ 3.0 3.1 3.2 Yang, Jin-Kui; Lin, Shan-Shan; Ji, Xiu-Juan; Guo, Li-Min (2009). "Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes". Acta Diabetologica. 47 (3): 193–199. doi:10.1007/s00592-009-0109-4. ISSN 0940-5429.
- ↑ Turner, Anthony J; Hiscox, Julian A; Hooper, Nigel M (2004). "ACE2: from vasopeptidase to SARS virus receptor". Trends in Pharmacological Sciences. 25 (6): 291–294. doi:10.1016/j.tips.2004.04.001. ISSN 0165-6147.
- ↑ 5.0 5.1 Li, Wenhui; Moore, Michael J.; Vasilieva, Natalya; Sui, Jianhua; Wong, Swee Kee; Berne, Michael A.; Somasundaran, Mohan; Sullivan, John L.; Luzuriaga, Katherine; Greenough, Thomas C.; Choe, Hyeryun; Farzan, Michael (2003). "Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus". Nature. 426 (6965): 450–454. doi:10.1038/nature02145. ISSN 0028-0836.
- ↑ Bornstein, Stefan R.; Dalan, Rinkoo; Hopkins, David; Mingrone, Geltrude; Boehm, Bernhard O. (2020). "Endocrine and metabolic link to coronavirus infection". Nature Reviews Endocrinology. 16 (6): 297–298. doi:10.1038/s41574-020-0353-9. ISSN 1759-5029.
- ↑ 7.0 7.1 Hoffmann, Markus; Kleine-Weber, Hannah; Schroeder, Simon; Krüger, Nadine; Herrler, Tanja; Erichsen, Sandra; Schiergens, Tobias S.; Herrler, Georg; Wu, Nai-Huei; Nitsche, Andreas; Müller, Marcel A.; Drosten, Christian; Pöhlmann, Stefan (2020). "SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor". Cell. 181 (2): 271–280.e8. doi:10.1016/j.cell.2020.02.052. ISSN 0092-8674.
- ↑ 8.0 8.1 8.2 Yang, Liuliu; Han, Yuling; Nilsson-Payant, Benjamin E.; Gupta, Vikas; Wang, Pengfei; Duan, Xiaohua; Tang, Xuming; Zhu, Jiajun; Zhao, Zeping; Jaffré, Fabrice; Zhang, Tuo; Kim, Tae Wan; Harschnitz, Oliver; Redmond, David; Houghton, Sean; Liu, Chengyang; Naji, Ali; Ciceri, Gabriele; Guttikonda, Sudha; Bram, Yaron; Nguyen, Duc-Huy T.; Cioffi, Michele; Chandar, Vasuretha; Hoagland, Daisy A.; Huang, Yaoxing; Xiang, Jenny; Wang, Hui; Lyden, David; Borczuk, Alain; Chen, Huanhuan Joyce; Studer, Lorenz; Pan, Fong Cheng; Ho, David D.; tenOever, Benjamin R.; Evans, Todd; Schwartz, Robert E.; Chen, Shuibing (2020). "A Human Pluripotent Stem Cell-based Platform to Study SARS-CoV-2 Tropism and Model Virus Infection in Human Cells and Organoids". Cell Stem Cell. doi:10.1016/j.stem.2020.06.015. ISSN 1934-5909.
- ↑ Patel, Vaibhav B.; Zhong, Jiu-Chang; Grant, Maria B.; Oudit, Gavin Y. (2016). "Role of the ACE2/Angiotensin 1–7 Axis of the Renin–Angiotensin System in Heart Failure". Circulation Research. 118 (8): 1313–1326. doi:10.1161/CIRCRESAHA.116.307708. ISSN 0009-7330.
- ↑ Wang, Kaiming; Gheblawi, Mahmoud; Oudit, Gavin Y. (2020). "Angiotensin Converting Enzyme 2: A Double-Edged Sword". Circulation. doi:10.1161/CIRCULATIONAHA.120.047049. ISSN 0009-7322.
- ↑ Walls, Alexandra C.; Park, Young-Jun; Tortorici, M. Alejandra; Wall, Abigail; McGuire, Andrew T.; Veesler, David (2020). "Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein". Cell. 181 (2): 281–292.e6. doi:10.1016/j.cell.2020.02.058. ISSN 0092-8674.
- ↑ Zhou, Peng; Yang, Xing-Lou; Wang, Xian-Guang; Hu, Ben; Zhang, Lei; Zhang, Wei; Si, Hao-Rui; Zhu, Yan; Li, Bei; Huang, Chao-Lin; Chen, Hui-Dong; Chen, Jing; Luo, Yun; Guo, Hua; Jiang, Ren-Di; Liu, Mei-Qin; Chen, Ying; Shen, Xu-Rui; Wang, Xi; Zheng, Xiao-Shuang; Zhao, Kai; Chen, Quan-Jiao; Deng, Fei; Liu, Lin-Lin; Yan, Bing; Zhan, Fa-Xian; Wang, Yan-Yi; Xiao, Geng-Fu; Shi, Zheng-Li (2020). "A pneumonia outbreak associated with a new coronavirus of probable bat origin". Nature. 579 (7798): 270–273. doi:10.1038/s41586-020-2012-7. ISSN 0028-0836.
- ↑ Yan, Renhong; Zhang, Yuanyuan; Li, Yaning; Xia, Lu; Guo, Yingying; Zhou, Qiang (2020). "Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2". Science. 367 (6485): 1444–1448. doi:10.1126/science.abb2762. ISSN 0036-8075.
- ↑ Shang, Jian; Ye, Gang; Shi, Ke; Wan, Yushun; Luo, Chuming; Aihara, Hideki; Geng, Qibin; Auerbach, Ashley; Li, Fang (2020). "Structural basis of receptor recognition by SARS-CoV-2". Nature. 581 (7807): 221–224. doi:10.1038/s41586-020-2179-y. ISSN 0028-0836.
- ↑ Gheblawi, Mahmoud; Wang, Kaiming; Viveiros, Anissa; Nguyen, Quynh; Zhong, Jiu-Chang; Turner, Anthony J.; Raizada, Mohan K.; Grant, Maria B.; Oudit, Gavin Y. (2020). "Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System". Circulation Research. 126 (10): 1456–1474. doi:10.1161/CIRCRESAHA.120.317015. ISSN 0009-7330.
- ↑ Grankvist, K; Marklund, S L; Täljedal, I B (1981). "CuZn-superoxide dismutase, Mn-superoxide dismutase, catalase and glutathione peroxidase in pancreatic islets and other tissues in the mouse". Biochemical Journal. 199 (2): 393–398. doi:10.1042/bj1990393. ISSN 0264-6021.
- ↑ Bindom, Sharell M.; Lazartigues, Eric (2009). "The sweeter side of ACE2: Physiological evidence for a role in diabetes". Molecular and Cellular Endocrinology. 302 (2): 193–202. doi:10.1016/j.mce.2008.09.020. ISSN 0303-7207.
- ↑ Fliser, Danilo; Schaefer, Franz; Schmid, Daniela; Veldhuis, Johannes D.; Ritz, Eberhard (1997). "Angiotensin II Affects Basal, Pulsatile, and Glucose-Stimulated Insulin Secretion in Humans". Hypertension. 30 (5): 1156–1161. doi:10.1161/01.HYP.30.5.1156. ISSN 0194-911X.
- ↑ Gerich, J. E. (2002). "Is Reduced First-Phase Insulin Release the Earliest Detectable Abnormality in Individuals Destined to Develop Type 2 Diabetes?". Diabetes. 51 (Supplement 1): S117–S121. doi:10.2337/diabetes.51.2007.S117. ISSN 0012-1797.
- ↑ 20.0 20.1 20.2 Chee, Ying Jie; Ng, Shereen Jia Huey; Yeoh, Ester (2020). "Diabetic ketoacidosis precipitated by Covid-19 in a patient with newly diagnosed diabetes mellitus". Diabetes Research and Clinical Practice. 164: 108166. doi:10.1016/j.diabres.2020.108166. ISSN 0168-8227.