PEComa
| PEComa | |
 | |
|---|---|
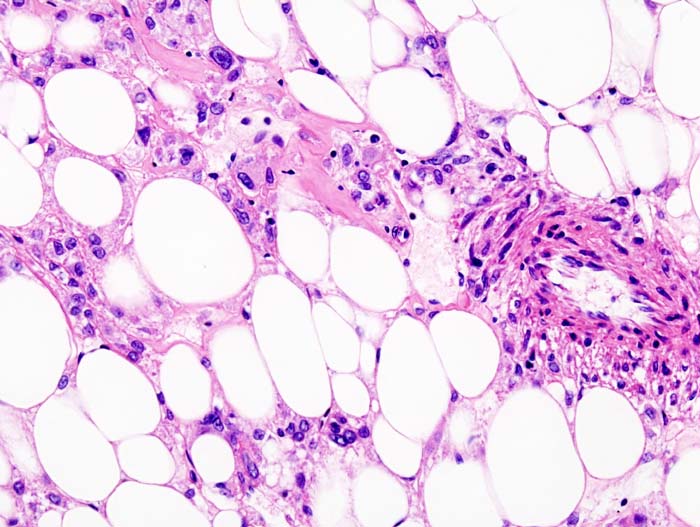
| Histopathologic image of renal angiomyolipoma. Nephrectomy specimen. H&E stain. | |
| MeSH | D054973 |
|
WikiDoc Resources for PEComa |
|
Articles |
|---|
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on PEComa at Clinical Trials.gov Clinical Trials on PEComa at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on PEComa
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating PEComa Risk calculators and risk factors for PEComa
|
|
Healthcare Provider Resources |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Zahir Ali Shaikh, MD[2]
Synonyms and keywords:
Overview
The World Health Organization defines Perivascular Epithelioid Cell Tumors (PEComas) as mesenchymal tumors composed of histologically and immunohistochemically distinctive perivascular epithelioid cells (PECs).
Historical Perspective
PEComas was first discovered by Pea and Colleagues in 1991, where they first noticed this unusual cell in both Angiolyolipoma (AML) and Clear Cell Sugar Tumor of Lung (CCST).[1]
In 1992, Bonetti and Colleagues proposed a cellular link between AML, CCST and lymphangioleiomyomatosis (LAM), their association with Tuberous Sclerosis Complex (TSC) and advanced the concept of a family of neoplasms composed of these distinctive cells which were immunoreactive with melanocytes markers and exhibit and epitheloid appearance, a clear acidophilic cytoplasm and a perivascular distribution.[2]
In 1996, Zamboni et al reported the first case of Pancreatic CCST and suggested the name PEComa for these neoplasms composed of a pure proliferation of Perivascular Epirhloid Cells (PECs).[3]
Classification
The World Health Organization defines Perivascular Epithelioid Cell Tumors (PEComas) as mesenchymal tumors composed of histologically and immunohistochemically distinctive perivascular epithelioid cells (PECs)[4]
There is no established system for the classification of PEComas because of the rarity of disease, but the PEComas are a group of tumors that includes following:[5]
- Angiomyolipoma (AML)
- Clear Cell Sugar Tumor Of Lung (CCST)
- Lymphangileiomyomatosis (LAM)
- PEComas Not Otherwise Specified (PEComas-NOS); which includes Clear Cell Myomelanocytic Tumor of falciform ligament/ligamentum teres, Abdominopelvic Sarcoma of perivascular epethelioid cells, primary extrapulmonary clear cell sugar tumor.
Pathophysiology
Perivascular Epithlioid Cell (PEC) is a cell type constantly present in a group of tumors called PEComas. It has no normal counterpart.
PEC expresses myogenic and melanocytic markers such as HMB45 and Actin.[6]
Microscopic Pathology
Perivascular Epithlioid Cells (PECs) are perivascular epithelioid cells with a clear/granular cytoplasm and round, oval, centrally located nucleus without prominent nucleoli. They have mild to any atypia.[6]
On ultrastructural analysis PEC contains microfilament bundles with electron dense condensation, numerous mitochondria and membrane bound dense granules.[7]
Genetics
The precursor cell of PEComas is currently unknown. Genetically, PECs are linked to the tuberous sclerosis genes TSC1 and TSC2.[6]
Causes
PEComas are cause by genetic factors. Mutations in the tuberous sclerosis genes TSC1 and TSC2 has been associated.[6]
Differentiating PEComa from other Diseases
PEComas must be differentiated from:[8]
- Epithelioid Smooth Muscle cell tumors(epithelioid leiomyosarcoma and epithelioid leiomyoma),
- Malignant Melanoma,
- Clear cell sarcoma of tendon and aponeroses(melanoma of soft parts),
- Alveolar soft part sarcoma,
- Endometrial stromal sarcoma with clear cell features,
- Carcinoma (especially renal cell and adrenocortical carcinoma)
- Paraganglioma
- Any other tumor with focal or prominent clear cell change
Epidemiology and Demographics
Patients of all age groups may develop PEComas, but the mean age at diagnosis is 54 years.[9]
Women are more commonly affected by PEComas than men.
Risk Factors
There are no established risk factors for PEComas, but the risk increases in patients with Tuberous Sclerosis as the PECs are associated with TSC1 and TSC2 genes.
Screening
There is insufficient evidence to recommend routine screening for PEComas.
Natural History, Complications, and Prognosis
- Clinically most PEComas follow a benign course.[10]
- Malignant PEComas-NOS are also reported and seen in uterus. Other sites including jejunum, prostate, pelvis, skull base, somatic soft tissue and broad ligament.
- Folpe and Colleagues suggested criteria for malignancy based of following 03 factors:[8]
- Size greater than 8.0 cm
- Mitotic count of 1/50 high power field (HPF)
- Necrosis
- They are categorized as Benign, Uncertain malignant potential and Malignant on the presence of none, 1, or 2 or more of the above three criteria.
Diagnosis
Immunohistochemical markers
PECs typically stain for melanocytic markers (HMB-45, HMSA-1, Melan A (Mart 1), microophthalmia transcription factor (Mitf)), myogenic markers (actin)and less commonly desmin. Immunoreactivity for vimentin is unclear.[6]
Diagnostic Study of Choice
The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: [criterion 1], [criterion 2], [criterion 3], and [criterion 4].
OR
The diagnosis of [disease name] is based on the [criteria name] criteria, which include [criterion 1], [criterion 2], and [criterion 3].
OR
The diagnosis of [disease name] is based on the [definition name] definition, which includes [criterion 1], [criterion 2], and [criterion 3].
OR
There are no established criteria for the diagnosis of [disease name].
History and Symptoms
The majority of patients with [disease name] are asymptomatic.
OR
The hallmark of [disease name] is [finding]. A positive history of [finding 1] and [finding 2] is suggestive of [disease name]. The most common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3]. Common symptoms of [disease] include [symptom 1], [symptom 2], and [symptom 3]. Less common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3].
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Laboratory Findings
There are no diagnostic laboratory findings associated with PEComas.
Electrocardiogram
There are no ECG findings associated with PEComas.
X-ray
There are no x-ray findings associated with PEDComas.
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with PEComas.
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with PEComas.
Treatment
Medical Therapy
There is no treatment for [disease name]; the mainstay of therapy is supportive care.
OR
Supportive therapy for [disease name] includes [therapy 1], [therapy 2], and [therapy 3].
OR
The majority of cases of [disease name] are self-limited and require only supportive care.
OR
[Disease name] is a medical emergency and requires prompt treatment.
OR
The mainstay of treatment for [disease name] is [therapy].
OR The optimal therapy for [malignancy name] depends on the stage at diagnosis.
OR
[Therapy] is recommended among all patients who develop [disease name].
OR
Pharmacologic medical therapy is recommended among patients with [disease subclass 1], [disease subclass 2], and [disease subclass 3].
OR
Pharmacologic medical therapies for [disease name] include (either) [therapy 1], [therapy 2], and/or [therapy 3].
OR
Empiric therapy for [disease name] depends on [disease factor 1] and [disease factor 2].
OR
Patients with [disease subclass 1] are treated with [therapy 1], whereas patients with [disease subclass 2] are treated with [therapy 2].
Surgery
Surgical intervention is not recommended for the management of [disease name].
OR
Surgery is not the first-line treatment option for patients with [disease name]. Surgery is usually reserved for patients with either [indication 1], [indication 2], and [indication 3]
OR
The mainstay of treatment for [disease name] is medical therapy. Surgery is usually reserved for patients with either [indication 1], [indication 2], and/or [indication 3].
OR
The feasibility of surgery depends on the stage of [malignancy] at diagnosis.
OR
Surgery is the mainstay of treatment for [disease or malignancy].
Primary Prevention
There are no established measures for the primary prevention of PEComas.
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
OR
Effective measures for the secondary prevention of [disease name] include [strategy 1], [strategy 2], and [strategy 3].
References
- ↑ Pea M, Bonetti F, Zamboni G, Martignoni G, Fiore-Donati L, Doglioni C (1991). "Clear cell tumor and angiomyolipoma". Am J Surg Pathol. 15 (2): 199–202. PMID 2025321.
- ↑ Bonetti F, Pea M, Martignoni G, Zamboni G (1992). "PEC and sugar". Am J Surg Pathol. 16 (3): 307–8. PMID https://www.ncbi.nlm.nih.gov/pubmed/1599021 Check
|pmid=value (help). - ↑ Zamboni G, Pea M, Martignoni G, Zancanaro C, Faccioli G, Gilioli E; et al. (1996). "Clear cell "sugar" tumor of the pancreas. A novel member of the family of lesions characterized by the presence of perivascular epithelioid cells". Am J Surg Pathol. 20 (6): 722–30. PMID https://www.ncbi.nlm.nih.gov/pubmed/8651352 Check
|pmid=value (help). - ↑ Fletcher, Christopher (2002). Pathology and genetics of tumours of soft tissue and bone. Lyon: IARC Press. ISBN 9789283224136.
- ↑ Fletcher, Christopher (2013). WHO classification of tumours of soft tissue and bone. Lyon: IARC Press. ISBN 978-9283224341.
- ↑ 6.0 6.1 6.2 6.3 6.4 Martignoni G, Pea M, Reghellin D, Zamboni G, Bonetti F (2008). "PEComas: the past, the present and the future". Virchows Arch. 452 (2): 119–32. doi:10.1007/s00428-007-0509-1. PMC 2234444. PMID https://www.ncbi.nlm.nih.gov/pubmed/18080139 Check
|pmid=value (help). - ↑ D. A. Weeks, R. L. Malott, M. Arnesen, C. Zuppan, D. Aitken & G. Mierau (1991). "Hepatic angiomyolipoma with striated granules and positivity with melanoma--specific antibody (HMB-45): a report of two cases". Ultrastructural pathology. 15 (4–5): 563–571. PMID 1755113. Unknown parameter
|month=ignored (help) - ↑ 8.0 8.1 Folpe AL, Mentzel T, Lehr HA, Fisher C, Balzer BL, Weiss SW (2005). "Perivascular epithelioid cell neoplasms of soft tissue and gynecologic origin: a clinicopathologic study of 26 cases and review of the literature". Am J Surg Pathol. 29 (12): 1558–75. PMID https://www.ncbi.nlm.nih.gov/pubmed/16327428 Check
|pmid=value (help). - ↑ Vang R, Kempson RL (2002). "Perivascular epithelioid cell tumor ('PEComa') of the uterus: a subset of HMB-45-positive epithelioid mesenchymal neoplasms with an uncertain relationship to pure smooth muscle tumors". Am J Surg Pathol. 26 (1): 1–13. PMID https://www.ncbi.nlm.nih.gov/pubmed/11756764 Check
|pmid=value (help). - ↑ Fletcher, Christopher (2013). WHO classification of tumours of soft tissue and bone. Lyon: IARC Press. ISBN 978-9283224341.