Sandbox:FB
\INTRO
Rhinitis implies inflammation of the nasal mucous membranes, inflammatory cell infiltrates are not characteristic or found in all disorders considered to be rhinitis. Rhinitis refers to a heterogeneous group of nasal disorders characterized by one or more of the following symptoms: sneezing, nasal itching, rhinorrhea, and nasal congestion-pmid 24007929
(PMID:18662584)-Rhinitis is a significant cause of widespread morbidity, medical treatment costs, reduced work productivity, and lost school days. Although sometimes mistakenly viewed as a trivial disease, symptoms of allergic and nonallergic rhinitis may significantly affect a patient's quality of life and can be associated with conditions such as fatigue, headache, cognitive impairment, and sleep disturbance. . The financial burden to society for allergic rhinitis is substantial. The total direct ($7.3 billion) and indirect costs ($4.28 billion, including loss of productivity) estimated in the United States for 2002 were $11.58 billion(PMID: 15025839 ((2004 publication, check more recent burden))
Historical Perspective
(some natural hx embedded) Rhinitis is a very frequent disease, sometimes mistakenly treated as a trivial disease. It is a significant cause of lost school and work days. Rhinitis results in more than two million absent school days annually in the United state, and it has a huge financial impact on the society.PMID18662584. Rhinitis can be allergic, non-allergic, infectious, hormonal, occupational, and other factors.18662584,24007929. Chronic rhinitis symptoms are among the most common problems presenting to physicians(pmid 17153005). Allergic rhinitis is the most common type of chronic rhinitis, but 30–50 % of patients with rhinitis have non-allergic triggers.24007929. Allergic rhinitis (AR) is rarely found in isolation, it is frequently associated with asthma and the coexistence is rather complex. It is also associated with sinusitis, which is a frequent extension of rhinitis(rhinosinusitis), and a frequently missed diagnosis-16634358. Other comorbid disorders associated with allergic rhinitis are chronic middle ear effusions, and lymphoid hypertrophy with obstructive sleep apnea, disordered sleep, and consequent behavioral and educational effects.PMID:16634358. Nonallergic rhinitis is often characterized by onset after age 20, female predominance, nasal hyperactivity, perennial symptoms, and nasal eosinophilia in approximately one-third of the population.PMID:17153005 Severe allergic rhinitis is associated with a diminished quality of life, disordered sleep and impaired work performance. PMID:18662584
NARES was first described in 1981 by Jacobs et al. 16579871, 7204783
23762613-Primary atrophic rhinitis or ozaena is a well-known disease for ages and was first described by Fraenkel in the latter part of the nineteenth century [1]. The disease is characterized by a sclerotic change in the mucous membrane and abnormal patency of the nasal passages due to atrophic changes in the mucosa and underlying bones, along with thick viscid secretions which, when dry, emit a characteristic foul smell. Atrophic rhinitis can be classified into two types, that is, a primary or idiopathic type where the etiology is not known and a secondary type where the disease develops secondary to some other primary disease. The condition is predominantly seen in young and middle aged adults, especially females (F : M = 5.6 : 1) [2]. Its prevalence varies in different regions of the world. It is a common condition in tropical countries such as India. In the countries with higher prevalence, primary atrophic rhinitis can affect 0.3%–1.0% of the population [3]. The exact etiology of primary atrophic rhinitis is unknown though many theories and hypotheses have been postulated for explanation of atrophic rhinitis. The factors blamed for its genesis are specific infections, autoimmunity, chronic sinus infection, hormonal imbalance, poor nutritional status, heredity, and iron deficiency
8820180-1996 article on atrophic rhinitis, in bookmark
Although asthma and other forms of allergic disease have been described in antiquity, ‘hay fever’ is surprisingly modern. Very rare descriptions can be traced back to Islamic texts of the 9th century and European texts of the 16th century. It was only in the early 19th century that the disease was carefully described, and at that time it was regarded as most unusual (3). In the 19th century, the disease followed the industrialization of westernized countries (4). By the end of the 19th century it had become commonplace in both Europe and North America. However, the prevalence of allergic rhinitis was still low and has considerably increased during the past 50 years. In some countries, over 50% of adolescents are reporting symptoms of allergic rhinitis (5). Using a conservative estimate, allergic rhinitis occurs in over 500 million people around the world. The prevalence of allergic rhinitis is increasing in most countries of the world, and particularly in areas with low or medium levels of prevalence. However, it may be plateauing or even decreasing in the highest prevalence areas. Rhinitis and allergic diseases are now taken seriously and the European Union (6) or countries such as Canada have specific programs to better understand, manage and prevent allergic diseases.(ARIA)
Allergic disease is a product of a genetic predisposition, epigenetic events, and environmental exposures. This complexity underlies why epidemiologic results often show marked variability when studies are performed in different populations and locations.Epidemiological studies demonstrate marked variability globally in the prevalence of both rhinitis symptoms and allergy tests. Self-reported seasonal or perennial rhinitis symptoms significantly overestimate the prevalence of AR defined by a positive history and positive allergy tests. Positive allergy tests are also common in those without self-reported rhinitis symptoms.Allergic rhinitis (AR) is one of the most common conditions seen by otolaryngologists and was the most common diagnosis reported in the year 2000 Otolaryngology Workforce study.[1] Determining who has AR and who does not has been surprisingly problematic, which makes epidemiologic studies subject to some interpretation. However understanding the epidemiology of allergy testing, AR, and non-AR provides clinically useful insights into the nature of allergic conditions. It is widely cited that AR is more prevalent in children, In the United States, rhinoconjunctivitis symptoms increased from 13.4% to 19.1% over 8 years (n = 2422; 13-year-olds to 14-year-olds).[9] Burden of disease
Estimates of the direct costs of AR in the United States have ranged from $1.6 to $4.9 billion dollars and estimates of indirect costs have ranged from $0.1 to $9.7 billion.[10] Quality of life diminishes in self-reported AR across multiple domains, with sleep disturbance reported in 88% of children and 57% of adults.[11, 12] Decreased productivity at school and work (“presenteeism”) has been described in children and adults.[11, 13] .25182349
PMID: 22056609 Allergic and nonallergic rhinitis have each been associated with asthma.8, 9, 10 and 11 Allergic rhinitis is also associated with eczema8 and 10 and reactions to foods—mainly to foods of plant origin, such as fruits from the Rosaceae family, tree nuts, peanuts, and some vegetables.12, 13, 14 and 15 Individuals who are allergic to birch pollen, in particular, have reported symptoms in the mucosa of the oropharyngeal area when eating such foods.12, 13 and 15 Although the period during which patients with rhinitis have the most symptoms (the pollen season) is short, especially for individuals with sensitization to only 1 of leaf tree, grass, or weed pollen, oral symptoms to pollen-related food allergens can persist throughout the year. Children with allergic rhinitis are more likely to have a persistent disease than are children with nonallergic rhinitis, who seem to remit. Among children with allergic rhinitis, sensitization to inhaled allergens seems to precede symptoms of rhinitis rather than symptoms of rhinitis preceding sensitization. OAS is common among school-aged children with allergic rhinitis who are sensitized to birch.Allergic rhinitis, nonallergic rhinitis, and sensitization without rhinitis were all significantly associated with asthma, eczema, and food hypersensitivity among 4- and 8-year-olds (Table IV). Allergic rhinitis was the only disorder associated with OAS. Twenty-five percent of children with allergic rhinitis also had OAS. Comparing children with allergic rhinitis and sensitization to birch to children with allergic rhinitis with sensitization other than birch, the proportions of OAS were 31% and 5%, respectively (P < .001). Sensitization to timothy was not associated with OAS (data not shown).Nonallergic rhinitis in the pediatric population has not been well studied, probably because there are several causes of blocked or runny noses in children. Recurrent viral infections that produce runny nose as the main symptom can be misclassified as prolonged, noninfectious rhinitis. An enlarged or chronically infected adenoid can mimic rhinitis symptoms. It is important to note that 73% of 4-year-olds with nonallergic rhinitis undergo remission by age 8 years. The high prevalence of food hypersensitivity among children with allergic rhinitis probably results from cross-reactions to pollen among children who are sensitized to birch. Symptoms corresponding to OAS were reported by 25% of children with allergic rhinitis.
Classification
PMID:18662584,PMID: 24007929
| Classification of Rhinitis[1][2] | ||
|---|---|---|
| Class | Types/causes | |
| Allergic rhinitis | US Joint Task Force on Practice Parameters(JTF) classification of allergic rhinitis | Seasonal |
| Perennial | ||
| Episodic | ||
| Allergic Rhinitis and its Impact on Asthma(ARIA) classification of allergic rhinitis | Intermittent | |
| Persistent | ||
| Nonallergic rhinitis | Vasomotor rhinitis | Irritant triggered |
| Cold air/Dry air | ||
| Exercise | ||
| Undetermined or poorly defined triggers | ||
| Gustatory rhinitis | ||
| Infectious | Acute | |
| Chronic | ||
| NARES
(Nonallergic rhinitis with eosinophilia syndrome) |
||
| Occupational rhinitis | IgE-mediated
(caused by protein and chemical allergens) |
|
| Immune mechanism uncertain
(caused by chemical respiratory sensitizers) |
||
| Work-aggravated rhinitis | ||
| Other rhinitis syndromes | Hormonally induced | Gestational |
| Menstrual cycle related | ||
| Drug-induced | Rhinitis medicamentosa | |
| Oral contraceptives | ||
| Antihypertensives and cardiovascular agents | ||
| Aspirin/NSAIDs | ||
| Other drugs | ||
| Atrophic rhinitis | ||
| Rhinitis associated with inflammatory-immunologic disorders | Granulomatous infections | |
| Wegener granulomatosis | ||
| Sarcoidosis | ||
| Midline granuloma | ||
| Churg-Strauss | ||
| Relapsing polychondritis | ||
| Amyloidosis | ||
Modified Classification of Allergic Rhinitis According to Severity of Symptoms and Quality of Life Impairment(pmid24007929, 18331513,
| |
|---|---|
| Type | Clinical characteristic |
| Intermittent | Symptoms are present on fewer than four days a week and for less than four weeks |
| Persistent | Symptoms are present on more than four days a week and for more than four consecutive weeks |
| |
Episodic rhinitis-symptoms are elicited by sporadic exposure to inhalant allergens not normally present in the person's daily environment(Diseases of the sinuses: a comprehensive textbook of diagnosis and treatment.pg134)
Pathophysiology
- PMID:
- 20176255-patho
Anatomy of the nose-11516776,10565476
The nose is an olfactory and respiratory organ
The nasal cavity is divided by a vertical partition (the “nasal septum”) into a right and left side.The nasal cavity is the most superior part of the respiratory tract. It extends from the vestibule to the nasopharynx.
- The vestibule refers to the area surrounding the external opening to the nasal cavity.
- The olfactory region is located at the apex of the nasal cavity. It is lined by olfactory cells with olfactory receptors.
- The respiratory region is the largest, and is lined by ciliated psudeostratified epithelium. Within the epithelium are interspersed mucus-secreting goblet cells.
Projecting out of the lateral walls of the nasal cavity are curved shelves of bone. They are called conchae (or turbinates). The are three conchae – inferior, middle and superior.
The inferior, middle, and superior turbinates in the nasal cavity promote air filtration, humidification, and temperature regulation
They project into the nasal cavity, creating four pathways for the air to flow. These pathways are called meatuses:
- Inferior meatus: Lies between the inferior concha and floor of the nasal cavity.
- Middle meatus: Lies between the inferior and middle concha.
- Superior meatus: Lies between the middle and superior concha.
- Spheno-ethmoidal recess: Lies superiorly and posteriorly to the superior concha.
hey project into the nasal cavity, creating four pathways for the air to flow. These pathways are called meatuses:
- Inferior meatus: Lies between the inferior concha and floor of the nasal cavity.
- Middle meatus: Lies between the inferior and middle concha.
- Superior meatus: Lies between the middle and superior concha.
- Spheno-ethmoidal recess: Lies superiorly and posteriorly to the superior concha.
The paranasal sinuses drain into the nasal cavity.Auditory/eustachian tubes open into the nasopharynx at the level of the inferior meatus.
nasal tissues are highly vascular, vascular changes can lead to significant nasal obstruction
Vasoconstriction and consequent decreases in nasal airway resistance result from sympathetic nerve stimulation. Parasympathetic nerve stimulation promotes secretion from nasal airway glands and nasal congestion
Pathophysiology of allergic rhinitis
Common allergens causing allergic rhinitis include proteins and glycoproteins in airborne dust mite fecal particles, cockroach residues, animal danders, molds, and pollens
On inhalation, allergen particles are deposited in nasal mucus, with subsequent elution of allergenic proteins and diffusion into nasal tissues. In addition, small-molecular-weight chemicals in occupational agents or drugs can act as haptens that react with self-proteins in the airway to form complete allergens
Causes
PMID:18662584,PMID: 24007929, 18331513
| Classification of Rhinitis | ||
|---|---|---|
| Class | Types/causes | |
| Allergic rhinitis | US Joint Task Force on Practice Parameters(JTF)classification of allergic rhinitis | Seasonal |
| Perennial | ||
| Episodic | ||
| Allergic Rhinitis and its Impact on Asthma(ARIA)classification of allergic rhinitis | Intermittent | |
| Persistent | ||
| Nonallergic rhinitis | Vasomotor rhinitis | Irritant triggered |
| Cold air/Dry air | ||
| Exercise | ||
| Undetermined or poorly defined triggers | ||
| Gustatory rhinitis | ||
| Infectious | Acute | |
| Chronic | ||
| NARES
(Nonallergic rhinitis with eosinophilia syndrome) |
||
| Occupational rhinitis | IgE-mediated
(caused by protein and chemical allergens) |
|
| Immune mechanism uncertain
(caused by chemical respiratory sensitizers) |
||
| Work-aggravated rhinitis | ||
| Other rhinitis syndromes | Hormonally induced | Gestational |
| Menstrual cycle related | ||
| Drug-induced | Rhinitis medicamentosa | |
| Oral contraceptives | ||
| Antihypertensives and cardiovascular agents | ||
| Aspirin/NSAIDs | ||
| Other drugs | ||
| Atrophic rhinitis | ||
| Rhinitis associated with inflammatory-immunologic
disorders |
Granulomatous infections | |
| Wegener granulomatosis | ||
| Sarcoidosis | ||
| Midline granuloma | ||
| Churg-Strauss | ||
| Relapsing polychondritis | ||
| Amyloidosis | ||
Differential Diagnosis
| Differential Diagnosis of Rhinitis—Conditions that Might Mimic Symptoms of Rhinitis
pmid24007929, 18331513 | |
|---|---|
| Pathology | Causes |
| Nasal polyps |
|
| Structural/mechanical factors |
|
| Cerebrospinal rhinorrhea | |
| Ciliary dyskinesia syndrome | |
Diagnosis
Determining the etiology of rhinitis, whether it is allergic, nonallergic or perhaps, an overlap of both conditions poses a diagnostic challenge.Not only are presenting symptoms of allergic, nonallergic, and mixed rhinitis often indistinguishable from one another, but also the differential diagnosis of nonallergic rhinitis is extensive. PMID:17153005
MANAGEMENT
Appropriate management of rhinitis may be an important component in effective management of coexisting or complicating respiratory conditions, such as asthma, sinusitis, and sleep apnea
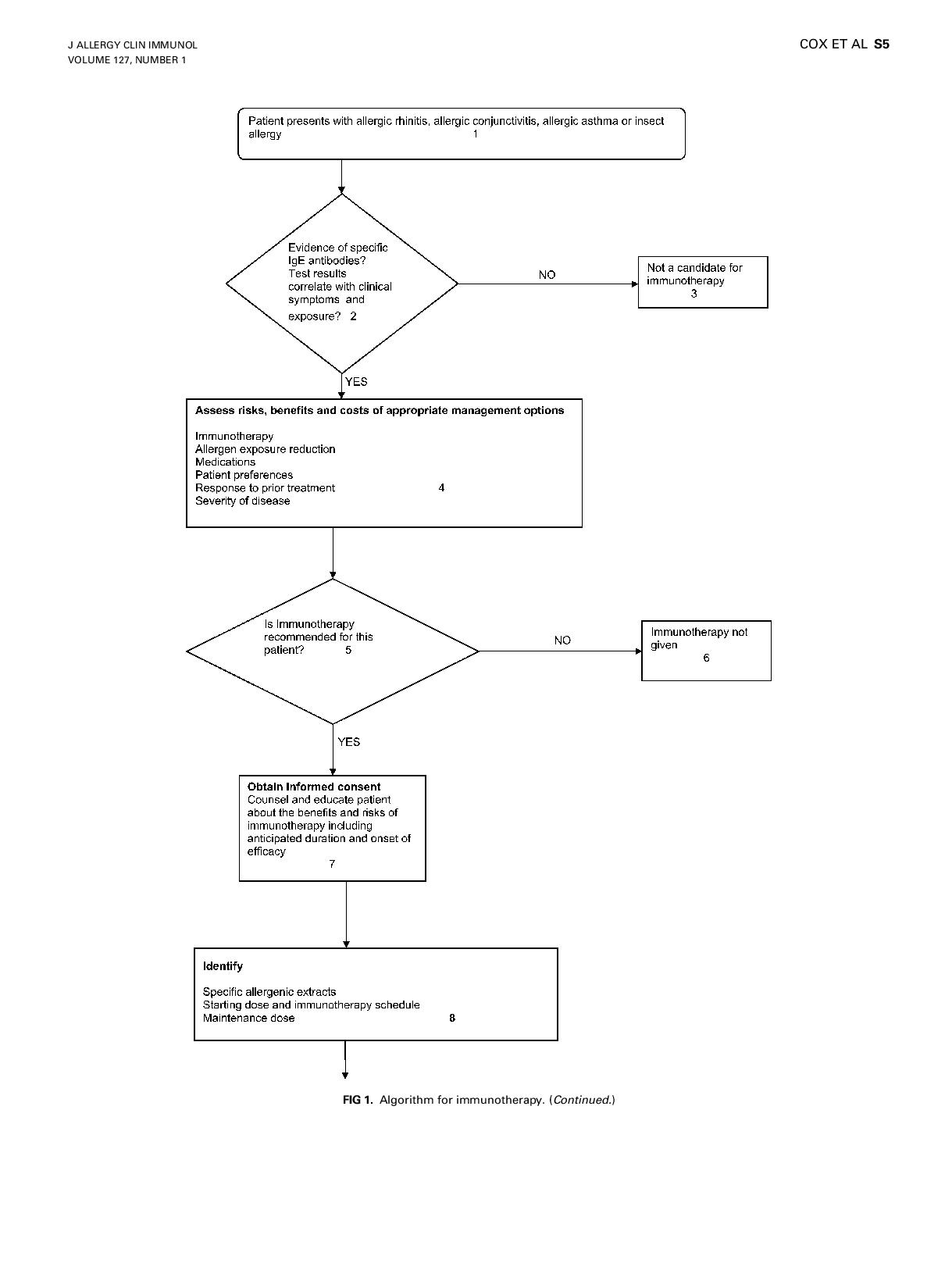
Algorithm for allergen immunotherapy.PMID:21122901
(PMID:17153005)In summary, the epidemiological data and characterization of allergic and nonallergic rhinitis has been reviewed. Chronic rhinitis symptoms are among the most common problems presenting to physicians. When approaching this problem the diagnostic challenge is to determine the etiology, specifically whether it is allergic, nonallergic, or perhaps an overlap of both conditions. Estimates of the prevalence of allergic rhinitis range from as low as 9% to as high as 42%. Although the prevalence of nonallergic rhinitis has not been studied definitively, it appears to be very common with an estimated prevalence in the United States of approximately 19 million. In comparison, the prevalence of mixed rhinitis is approximately 26 million, and allergic rhinitis ("pure" and "mixed" combined) 58 million. Challenges in the differential diagnosis of rhinitis result from two major factors. Not only are presenting symptoms of allergic, nonallergic, and mixed rhinitis often indistinguishable from one another, but also the differential diagnosis of nonallergic rhinitis is extensive. Nonallergic rhinitis is often characterized by onset after age 20, female predominance, nasal hyperactivity, perennial symptoms, and nasal eosinophilia in approximately one-third of the population. Positive tests for relevant specific IgE sensitivity in the setting of rhinitis do not rule out "mixed rhinitis" and may not rule out nonallergic rhinitis. The significance of symptom exacerbation by nonallergic triggers in the setting of allergic rhinitis remains to be determined. Goals for the future include reaching a consensus on the definitions of rhinitis and rhinitis subtypes including the establishment of mixed rhinitis, updating guidelines for the interpretation of nonrelevant positive tests for specific IgE sensitivity, and reaching agreement on the nonallergic triggers that best define VMR or VMR subtypes. Only then can the most applicable research results be obtained. The desired result is the delivery of the most appropriate treatment, specifically tailored to the accurate diagnosis of patients with rhinitis.
Complications
Sinusitis- rarely occurs in the absence of rhinitis(rhinosinusitis, nose and sinuses are contiguous structures sharing vascular, neuronal and interconnecting anatomic pathways. Overlap in clinical presentation btw rhinitis n rhinosinusitis often make differentiation btw d two diagnosis difficult. Page 133
Recurrent or chronic rhinitis-one of the most common medical conditions presenting for medical care in developed countries. Allergic-30-60million pple annually in the US(10-30% adult, up to 40% children. Nearly 3x as many pple suffer from allergic c\o pure nonallergic. In general, btw 44-87% of pxts evaluated for recurrent or chronic rhinitis present a 'mixed' combination of both allergic and nonallergic triggers.pg 133(use original ref). Rhinitis viewed as some as a minor dx, sig consequences to poor control-px morbidity(decreased QOL, increased medical costs, lost time/poor performance at sch/work. Rhinitis asso w sig comorbidities-conjunctivitis, sinus dx, asthma, otitis media, sleep apnea. Pg 133 Allergic rhinitis freq asso w allergic conjunctivitis(conjunctival redness, swelling, itching n excess lacrimation. Rx of underlying allergic rhinitis helps relieve ocular symptoms
Rhinitis-condition xterised by a constellation of nasal symptoms such as congestion, ant n post rhinorrhea, sneezing, itching
Textbook: Diseases of the sinuses: a comprehensive textbook of diagnosis and treatment(pg140), ISBN: 978-1-4939-0264-4 (Print) 978-1-4939-0265-1 (Online)
{{cite book |last1=Romeo |first1=Jonathan |last2=Dykewicz |first2=Mark |title=Diseases of the Sinuses |publisher=Springer New York |date=2014 |pages=133-152 |chapter=Chapter 9:Differential Diagnosis of Rhinitis and Rhinosinusitis |isbn=978-1-4939-0265-1}}
Jonathan Romeo DO, Mark S. Dykewicz MD
Chronic rhinosinusitis in children: PMID: 24007929
certain indections can lead to granulomatous nasal lesions, lesions can be ulcerative w formation of crust that can lead to nasal obstruction or bleeding. Tb,syphylis,leprosy,sporotrichosis,blastomycosis,histoplasmosis and coccidioidomycosis must be considered in pxts w ulcerative nasal lesions(pg 140)
Congenital syphilitic rhinorrhea: Congenital syphilis presents at birth or during infancy. Classical triad has been .described as rhinitis, pseudoparalysis and maculopapular rash. It can present as a hemolytic/bleeding disorder with anemia, jaundice, hepatoslenomegaly, and thrombocytopenia. Respiratory distress is also very common.PMCID: PMC1455023
Epidemiology of rhinitis: allergic and nonallergic. (PMID:17153005)
Rhinitis: a dose of epidemiological reality
Diagnosis and Management of Rhinitis: Complete Guidelines of the Joint Task Force on Practice Parameters in Allergy, Asthma and Immunology
Gestational rhinitis: pmid 26601995
chronic nasal dysfunction: pmid 26488532
Rhinitis risk: pmid 24028857
Asthma and rhinitis in cleaning workers: pmid 23931651
Rhinitis in children: pmid 25616224
Non-allergic rhinitis: pmid 26669462
Economic impact and quality-of-life burden of allergic rhinitis: PMID PMID: 15025839
The economic impact of allergic rhinitis and current guidelines for treatment.PMID: 21277528
- The diagnosis and management of rhinitis: an updated practice parameter: PMID: 18662584
- Recommendations for the pharmacologic management of allergic rhinitis: PMID: 25582158
Phenotypes and endotypes of rhinitis and their impact on management: a PRACTALL report. (PMID:25620381)
Classification of Nonallergic Rhinitis Syndromes With a Focus on Vasomotor Rhinitis, Proposed to be Known henceforth as Nonallergic Rhinopathy. (PMID:24229372)
Epidemiology of vasomotor rhinitis. (PMID:24229078)
Comparative analysis of allergic rhinitis in children and adults.
Recommendations for the pharmacologic management of allergic rhinitis.PMID:25582158
Rhinitis in the geriatric population. (PMID:20465792)
- Eipidemiology(more info)
- (PMID: 25645524)
Allergic rhinitis (AR) is one of the most common diseases affecting adults.1 It is the most common chronic disease in children in the United States today2 and is the fifth most chronic disease in the United States overall.3 Allergic rhinitis is estimated to affect nearly 1 in every 6 Americans and generates $2 to $5 billion in direct health expenditures annually.4,5 It can impair quality of life and, through loss of work and school, is responsible for as much as $2 to $4 billion in lost productivity annually.4,5 Not surprisingly, there are myriad diagnostic tests and treatments used in managing patients with this disorder, yet there is considerable variation in their use. This clinical practice guideline (CPG) was undertaken to optimize the care of patients with AR by addressing quality improvement opportunities through an evaluation of the available evidence and an assessment of the harm-benefit balance of various diagnostic and management options.
Non-allergic rhinitis: a case report and review.
Nozad CH, Michael LM, Betty Lew D, Michael CF.
Clin Mol Allergy. 2010 Feb 3;8:1. doi: 10.1186/1476-7961-8-1.
- PMID:
- 20181075Free PMC Article
Similar articles
- ↑ Wallace DV, Dykewicz MS, Bernstein DI, Blessing-Moore J, Cox L, Khan DA; et al. (2008). "The diagnosis and management of rhinitis: an updated practice parameter". J Allergy Clin Immunol. 122 (2 Suppl): S1–84. doi:10.1016/j.jaci.2008.06.003. PMID PMID:18662584 Check
|pmid=value (help). - ↑ Sacre-Hazouri JA (2012). "[Chronic rhinosinusitis in children]". Rev Alerg Mex. 59 (1): 16–24. PMID 24007929 PMID: 24007929 Check
|pmid=value (help).