Clevidipine clinical studies
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]
Clinical Studies
14.1 Perioperative Hypertension
Cleviprex was evaluated in two double-blind, randomized, parallel, placebo-controlled, multicenter trials of cardiac surgery patients—pre-operative use in ESCAPE-1 (n=105) and post-operative use in ESCAPE-2 (n=110). Patients were undergoing coronary artery bypass grafting, with or without valve replacement. Inclusion in ESCAPE-1 required a systolic pressure ≥160 mmHg. In ESCAPE-2, the entry criterion was systolic pressure of ≥140 mmHg within 4 hours of the completed surgery. The mean baseline blood pressure was 178/77 mmHg in ESCAPE -1 and 150/71 mmHg in ESCAPE 2. The population of both studies included 27% females and 47% patients older than age 65.
Cleviprex was infused in ESCAPE-1 preoperatively for 30 minutes, until treatment failure, or until induction of anesthesia, whichever came first. Cleviprex was infused in ESCAPE-2 postoperatively for a minimum of 30 minutes unless alternative therapy was required. The maximum infusion time allowed in the ESCAPE studies was 60 minutes.
In both studies infusion of Cleviprex was started at a dose of 1- 2 mg/hour and was titrated upwards, as tolerated, in doubling increments every 90 seconds up to an infusion rate of 16 mg/hour in order to achieve the desired blood pressure-lowering effect. At doses above 16 mg/hour increments were 7 mg/hour. The average Cleviprex infusion rate in ESCAPE-1 was 15.3 mg/hour and in ESCAPE-2 it was 5.1 mg/hour. The mean duration of exposure in the same ESCAPE studies was 30 minutes for the Cleviprex treated patients.
Approximately 4% of Cleviprex-treated subjects in ESCAPE-1 and 41% in ESCAPE-2 were on concomitant vasodilators during the first 30 minutes of Cleviprex administration.
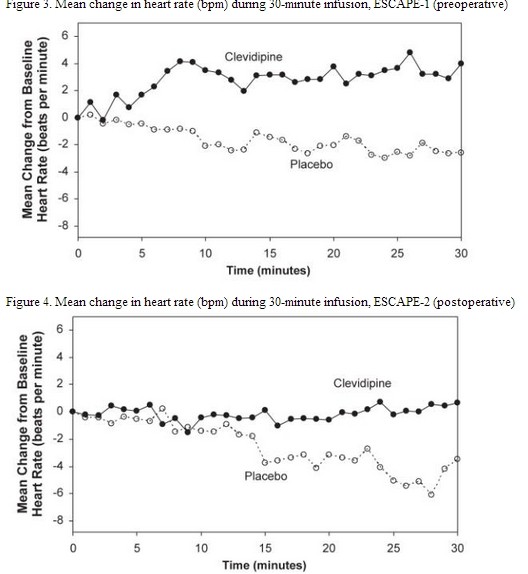
Cleviprex lowered blood pressure within 2-4 minutes. The change in systolic blood pressure over 30 minutes for ESCAPE-1 (preoperative) and ESCAPE-2 (postoperative) are shown in Figure 1 and 2.
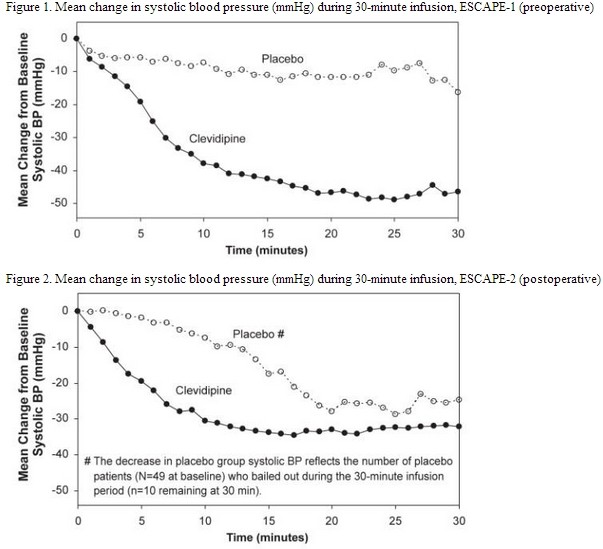 |
The change in heart rate over 30 minutes for ESCAPE-1 (preoperative) and ESCAPE-2 (postoperative) are shown in Figure 3 and 4.
 |
In three Phase 3 open-label clinical trials (ECLIPSE), 1512 patients were randomized to receive Cleviprex, nitroglycerin (perioperative hypertension), sodium nitroprusside (perioperative hypertension), or nicardipine (postoperative hypertension), for the treatment of hypertension in cardiac surgery. The mean exposure in the ECLIPSE studies was 8 hours at 4.5 mg/hour for the 752 patients who were treated with Cleviprex. Blood pressure control was assessed by measuring the magnitude and duration of SBP excursions outside the predefined pre- and post-operative SBP target range of 75-145 mmHg and the predefined intra-operative SBP range of 65-135 mmHg. In general, blood pressure control was similar with the four treatments.
14.2 Severe Hypertension
Cleviprex was evaluated in an open-label, uncontrolled clinical trial (VELOCITY) in 126 patients with severe hypertension (SBP >180 mmHg or diastolic blood pressure [DBP] >115 mmHg). Cleviprex infusion was initiated at 2 mg/hour and up-titrated every 3 minutes, doubling up to a maximum dose of 32 mg/hour as required to achieve a prespecified target blood pressure range within 30 minutes (primary endpoint). The transition to oral antihypertensive therapy was assessed for up to 6 hours following cessation of Cleviprex infusion.
The blood pressure effect in this study is shown in Figure 5. The average infusion rate was 9.5 mg/hour. The mean duration of Cleviprex exposure was 21 hours.
Figure 5. Mean percent change in SBP (%) during the first 30 minutes of infusion, VELOCITY (severe hypertension)
 |
Oral antihypertensive therapy was instituted 1 hour prior to the anticipated cessation of Cleviprex infusion. Transition to oral antihypertensive therapy within 6 hours after discontinuing Cleviprex infusion was successful in 91% (115/126) of patients. No patient had IV antihypertensive therapy reinstituted following transition to oral therapy.
14.3 Essential Hypertension
Cleviprex was evaluated in a randomized, placebo-controlled, single-blind, parallel 72 hour continuous infusion study in 61 mild to moderate essential hypertensives. The mean baseline blood pressure was 151/86 mmHg.
Subjects were randomized to placebo or to 2, 4, 8, or 16 mg/hour. Doses above 2 mg/hour were started at 2 mg/hour and force-titrated in 2-fold increments at 3-minute intervals. Blood pressure, heart rate, and blood levels of clevidipine were measured during the infusion period. Blood levels were monitored 1 hour after the infusion was discontinued. Blood pressure and heart rate were monitored for 8 hours and also at 96 hours after the termination of infusion. Systolic blood pressure effect was related to the concentration of clevidipine and plateaued at higher measured concentrations, with the maximal effect estimated at 25% of baseline systolic blood pressure. The estimated infusion rate necessary to achieve half of this maximal effect was approximately 10 mg/hour.[1]
References
- ↑ "CLEVIPREX (CLEVIDIPINE) EMULSION [THE MEDICINES COMPANY]". Retrieved 27 February 2014.