Perphenazine
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aparna Vuppala, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING
See full prescribing information for complete Boxed Warning.
|
Overview
Perphenazine is a {{{drugClass}}} that is FDA approved for the {{{indicationType}}} of {{{indication}}}. There is a Black Box Warning for this drug as shown here. Common adverse reactions include .
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Condition1
Perphenazine is indicated for use in the treatment of schizophrenia and for the control of severe nausea and vomiting in adults.
Perphenazine has not been shown effective for the management of behavioral complications in patients with mental retardation.
- Dosing Information
- Dosage
Condition2
- Dosing Information
- Dosage
Condition3
- Dosing Information
- Dosage
Condition4
- Dosing Information
- Dosage
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Perphenazine in adult patients.
Non–Guideline-Supported Use
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Perphenazine in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding FDA-Labeled Use of Perphenazine in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Perphenazine in pediatric patients.
Non–Guideline-Supported Use
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Perphenazine in pediatric patients.
Contraindications
- Perphenazine products are contraindicated in comatose or greatly obtunded patients and in patients receiving large doses of central nervous system depressants (barbiturates, alcohol, narcotics, analgesics, or antihistamines); in the presence of existing blood dyscrasias, bone marrow depression, or liver damage; and in patients who have shown hypersensitivity to perphenazine products, their components, or related compounds.
Perphenazine products are also contraindicated in patients with suspected or established subcortical brain damage, with or without hypothalamic damage, since a hyperthermic reaction with temperatures in excess of 104°F may occur in such patients, sometimes not until 14 to 16 hours after drug administration. Total body ice-packing is recommended for such a reaction; antipyretics may also be useful.
Warnings
|
WARNING
See full prescribing information for complete Boxed Warning.
|
- Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Perphenazine is not approved for the treatment of patients with dementia-related psychosis (see BOXED WARNING).
Tardive dyskinesia, a syndrome consisting of potentially irreversible, involuntary, dyskinetic movements, may develop in patients treated with antipsychotic drugs. Older patients are at increased risk for development of tardive dyskinesia. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely upon prevalence estimates to predict, at the inception of antipsychotic treatment, which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
Both the risk of developing the syndrome and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome, and thereby may possibly mask the underlying disease process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, especially in the elderly, antipsychotics should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that 1) is known to respond to antipsychotic drugs, and 2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on antipsychotics, drug discontinuation should be considered. However, some patients may require treatment despite the presence of the syndrome.
(For further information about the description of tardive dyskinesia and its clinical detection, please refer to INFORMATION FOR PATIENTS and ADVERSE REACTIONS.)
Neuroleptic Malignant Syndrome (NMS) A potentially fatal symptom complex, sometimes referred to as Neuroleptic Malignant Syndrome (NMS), has been reported in association with antipsychotic drugs. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmias).
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever and primary central nervous system (CNS) pathology.
The management of NMS should include 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy, 2) intensive symptomatic treatment and medical monitoring, and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
If hypotension develops, epinephrine should not be administered since its action is blocked and partially reversed by perphenazine. If a vasopressor is needed, norepinephrine may be used. Severe, acute hypotension has occurred with the use of phenothiazines and is particularly likely to occur in patients with mitral insufficiency or pheochromocytoma. Rebound hypertension may occur in pheochromocytoma patients.
Perphenazine products can lower the convulsive threshold in susceptible individuals; they should be used with caution in alcohol withdrawal and in patients with convulsive disorders. If the patient is being treated with an anticonvulsant agent, increased dosage of that agent may be required when perphenazine products are used concomitantly.
Perphenazine products should be used with caution in patients with psychic depression.
Perphenazine may impair the mental and/or physical abilities required for the performance of hazardous tasks such as driving a car or operating machinery; therefore, the patient should be warned accordingly.
Perphenazine products are not recommended for pediatric patients under 12 years of age.
Usage in Pregnancy Non-teratogenic Effects
Neonates exposed to antipsychotic drugs, during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery. There have been reports of agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder in these neonates. These complications have varied in severity; while in some cases symptoms have been self-limited, in other cases neonates have required intensive care unit support and prolonged hospitalization.
Perphenazine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Safe use of perphenazine during pregnancy and lactation has not been established; therefore, in administering the drug to pregnant patients, nursing mothers, or women who may become pregnant, the possible benefits must be weighed against the possible hazards to mother and child.
Precautions
Leukopenia, Neutropenia and Agranulocytosis In clinical trial and postmarketing experience, events of leukopenia/neutropenia and agranulocytosis have been reported temporally related to antipsychotic agents.
Possible risk factors for leukopenia/neutropenia include preexisting low white blood cell count (WBC) and history of drug induced leukopenia/neutropenia. Patients with a preexisting low WBC or a history of drug induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and should discontinue perphenazine tablets USP at the first sign of a decline in WBC in the absence of other causative factors.
Patients with neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count <1000/mm3) should discontinue perphenazine tablets USP and have their WBC followed until recovery.
The possibility of suicide in depressed patients remains during treatment and until significant remission occurs. This type of patient should not have access to large quantities of this drug.
As with all phenothiazine compounds, perphenazine should not be used indiscriminately. Caution should be observed in giving it to patients who have previously exhibited severe adverse reactions to other phenothiazines. Some of the untoward actions of perphenazine tend to appear more frequently when high doses are used. However, as with other phenothiazine compounds, patients receiving perphenazine products in any dosage should be kept under close supervision.
Antipsychotic drugs elevate prolactin levels; the elevation persists during chronic administration. Tissue culture experiments indicate that approximately one-third of human breast cancers are prolactin dependent in vitro, a factor of potential importance if the prescription of these drugs is contemplated in a patient with a previously detected breast cancer. Although disturbances such as galactorrhea, amenorrhea, gynecomastia, and impotence have been reported, the clinical significance of elevated serum prolactin levels is unknown for most patients. An increase in mammary neoplasms has been found in rodents after chronic administration of antipsychotic drugs. Neither clinical studies nor epidemiologic studies conducted to date, however, have shown an association between chronic administration of these drugs and mammary tumorigenesis; the available evidence is considered too limited to be conclusive at this time.
The antiemetic effect of perphenazine may obscure signs of toxicity due to overdosage of other drugs, or render more difficult the diagnosis of disorders such as brain tumors or intestinal obstruction.
A significant, not otherwise explained, rise in body temperature may suggest individual intolerance to perphenazine, in which case it should be discontinued.
Patients on large doses of a phenothiazine drug who are undergoing surgery should be watched carefully for possible hypotensive phenomena. Moreover, reduced amounts of anesthetics or central nervous system depressants may be necessary.
Since phenothiazines and central nervous system depressants (opiates, analgesics, antihistamines, barbiturates) can potentiate each other, less than the usual dosage of the added drug is recommended and caution is advised when they are administered concomitantly.
Use with caution in patients who are receiving atropine or related drugs because of additive anticholinergic effects and also in patients who will be exposed to extreme heat or phosphorus insecticides.
The use of alcohol should be avoided, since additive effects and hypotension may occur. Patients should be cautioned that their response to alcohol may be increased while they are being treated with perphenazine products. The risk of suicide and the danger of overdose may be increased in patients who use alcohol excessively due to its potentiation of the drug’s effect.
Blood counts and hepatic and renal functions should be checked periodically. The appearance of signs of blood dyscrasias requires the discontinuance of the drug and institution of appropriate therapy. If abnormalities in hepatic tests occur, phenothiazine treatment should be discontinued. Renal function in patients on long-term therapy should be monitored; if blood urea nitrogen (BUN) becomes abnormal, treatment with the drug should be discontinued.
The use of phenothiazine derivatives in patients with diminished renal function should be undertaken with caution.
Use with caution in patients suffering from respiratory impairment due to acute pulmonary infections, or in chronic respiratory disorders such as severe asthma or emphysema.
In general, phenothiazines, including perphenazine, do not produce psychic dependence. Gastritis, nausea and vomiting, dizziness, and tremulousness have been reported following abrupt cessation of high-dose therapy. Reports suggest that these symptoms can be reduced by continuing concomitant antiparkinson agents for several weeks after the phenothiazine is withdrawn.
The possibility of liver damage, corneal and lenticular deposits, and irreversible dyskinesias should be kept in mind when patients are on long-term therapy.
Because photosensitivity has been reported, undue exposure to the sun should be avoided during phenothiazine treatment.
- Description
Adverse Reactions
Clinical Trials Experience
There is limited information regarding Clinical Trial Experience of Perphenazine in the drug label.
Body as a Whole
Cardiovascular
Digestive
Endocrine
Hematologic and Lymphatic
Metabolic and Nutritional
Musculoskeletal
Neurologic
Respiratory
Skin and Hypersensitivy Reactions
Special Senses
Urogenital
Miscellaneous
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Perphenazine in the drug label.
Body as a Whole
Cardiovascular
Digestive
Endocrine
Hematologic and Lymphatic
Metabolic and Nutritional
Musculoskeletal
Neurologic
Respiratory
Skin and Hypersensitivy Reactions
Special Senses
Urogenital
Miscellaneous
Drug Interactions
- Drug Interactions
Metabolism of a number of medications, including antipsychotics, antidepressants, ß-blockers, and antiarrhythmics, occurs through the cytochrome P450 2D6 isoenzyme (debrisoquine hydroxylase). Approximately 10% of the Caucasian population has reduced activity of this enzyme, so-called “poor” metabolizers. Among other populations the prevalence is not known. Poor metabolizers demonstrate higher plasma concentrations of antipsychotic drugs at usual doses, which may correlate with emergence of side effects. In one study of 45 elderly patients suffering from dementia treated with perphenazine, the 5 patients who were prospectively identified as poor P450 2D6 metabolizers had reported significantly greater side effects during the first 10 days of treatment than the 40 extensive metabolizers, following which the groups tended to converge. Prospective phenotyping of elderly patients prior to antipsychotic treatment may identify those at risk for adverse events.
The concomitant administration of other drugs that inhibit the activity of P450 2D6 may acutely increase plasma concentrations of antipsychotics. Among these are tricyclic antidepressants and selective serotonin reuptake inhibitors, e.g., fluoxetine, sertraline and paroxetine. When prescribing these drugs to patients already receiving antipsychotic therapy, close monitoring is essential and dose reduction may become necessary to avoid toxicity. Lower doses than usually prescribed for either the antipsychotic or the other drug may be required.
Use in Specific Populations
Pregnancy
- Pregnancy Category
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Perphenazine in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Perphenazine during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Perphenazine with respect to nursing mothers.
Pediatric Use
There is no FDA guidance on the use of Perphenazine with respect to pediatric patients.
Geriatic Use
There is no FDA guidance on the use of Perphenazine with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Perphenazine with respect to specific gender populations.
Race
There is no FDA guidance on the use of Perphenazine with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Perphenazine in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Perphenazine in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Perphenazine in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Perphenazine in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
- Intravenous
Monitoring
There is limited information regarding Monitoring of Perphenazine in the drug label.
- Description
IV Compatibility
There is limited information regarding IV Compatibility of Perphenazine in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- Description
Management
- Description
Chronic Overdose
There is limited information regarding Chronic Overdose of Perphenazine in the drug label.
Pharmacology
There is limited information regarding Perphenazine Pharmacology in the drug label.
Mechanism of Action
- Perphenazine has actions at all levels of the central nervous system, particularly the hypothalamus. However, the site and mechanism of action of therapeutic effect are not known.
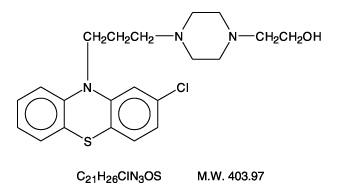
Structure
- Perphenazine (4-[3-(2-chlorophenothiazin-10-yl)propyl]-1-piperazineethanol), a piperazinyl phenothiazine, having the chemical formula, C21H26CIN3OS. It is available as oral tablets containing 2 mg, 4 mg, 8 mg, and 16 mg of perphenazine.
- Inactive ingredients: lactose (monohydrate), hydroxypropyl cellulose, hydroxypropyl methylcellulose, magnesium stearate, microcrystalline cellulose, polyethylene glycol, starch (corn), titanium dioxide, and polysorbate 80. Its structural formula is:
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Perphenazine in the drug label.
Pharmacokinetics
Following oral administration of perphenazine tablets, mean peak plasma perphenazine concentrations were observed between 1 to 3 hours. The plasma elimination half-life of perphenazine was independent of dose and ranged between 9 and 12 hours. In a study in which normal volunteers (n=12) received perphenazine 4 mg q8h for 5 days, steady-state concentrations of perphenazine were reached within 72 hours. Mean (%CV) Cmax and Cmin values for perphenazine and 7-hydroxyperphenazine at steady-state are listed below:

Peak 7-hydroxyperphenazine concentrations were observed between 2 to 4 hours with a terminal phase half-life ranging between 9.9 to 18.8 hours. Perphenazine is extensively metabolized in the liver to a number of metabolites by sulfoxidation, hydroxylation, dealkylation, and glucuronidation. The pharmacokinetics of perphenazine covary with the hydroxylation of debrisoquine which is mediated by cytochrome P450 2D6 (CYP 2D6) and thus is subject to genetic polymorphism – i.e., 7% to 10% of Caucasians and a low percentage of Asians have little or no activity and are called “poor metabolizers.” Poor metabolizers of CYP 2D6 will metabolize perphenazine more slowly and will experience higher concentrations compared with normal or “extensive” metabolizers.
Nonclinical Toxicology
There is limited information regarding Nonclinical Toxicology of Perphenazine in the drug label.
Clinical Studies
There is limited information regarding Clinical Studies of Perphenazine in the drug label.
How Supplied
Storage
There is limited information regarding Perphenazine Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Perphenazine |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Perphenazine |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Information for Patients This information is intended to aid in the safe and effective use of this medication. It is not a disclosure of all possible adverse or intended effects.
Given the likelihood that a substantial proportion of patients exposed chronically to antipsychotics will develop tardive dyskinesia, it is advised that all patients in whom chronic use is contemplated be given, if possible, full information about this risk. The decision to inform patients and/or their guardians must obviously take into account the clinical circumstances and the competency of the patient to understand the information provided.
Precautions with Alcohol
- Alcohol-Perphenazine interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- ®[1]
Look-Alike Drug Names
- A® — B®[2]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Empty citation (help)
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Perphenazine
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Perphenazine |Label Name=Perphenazine11.png
}}
{{#subobject:
|Label Page=Perphenazine |Label Name=Perphenazine11.png
}}