Macrocytic anemia laboratory findings: Difference between revisions
| Line 28: | Line 28: | ||
* If Part II is abnormal, Part III is basically a repeat of Part I after a course of antibiotics/vermicides. | * If Part II is abnormal, Part III is basically a repeat of Part I after a course of antibiotics/vermicides. | ||
* If this is abnormal, an malabsorptive cause is implicated. | * If this is abnormal, an malabsorptive cause is implicated. | ||
===Hematological findings=== | |||
MCV is often >110. Hct can often be as low as 15. Elevated LDH and bilirubin are seen since dyserythopoesis leads to destruction of >90% of RBC precursors. Hypersegmentation of PMNs is quite sensitive (>5% with 5 or more lobes or >1% with 6 lobes). Reticulocyte, WBC and platelets are low to normal. In one series of patients with B12 deficiency, 64% had a MCV greater than 100, and only 29% had anemia. | |||
In general the [[blood film]] can point towards vitamin deficiency: | |||
*Decreased [[red blood cell]] (RBC) count and [[hemoglobin]] levels | |||
*Increased [[mean corpuscular volume]] (MCV >95 fl often >110) and [[mean corpuscular hemoglobin]] (MCH) | |||
*The [[reticulocyte]] count is normal | |||
*The [[platelet]] count may be reduced. | |||
*[[Neutrophil granulocyte]]s may show multisegmented nuclei ("senile neutrophil"). This is thought to be due to decreased production and a compensatory prolonged lifespan for circulating neutrophils. | |||
*[[Anisocytosis]] (increased variation in RBC size) and [[poikilocytosis]] (abnormally shaped RBCs). | |||
*Macrocytes (larger than normal RBCs) are present. | |||
*Ovalocytes (oval shaped RBCs) are present. | |||
*[[Bone marrow]] (not normally checked in a patient suspected of megaloblastic anemia) shows megaloblastic [[hyperplasia]]. | |||
*[[Howell-Jolly body|Howell-Jolly bodies]] (chromosomal remnant) also present. | |||
'''Blood chemistries will also show:''' | |||
*Increased homocysteine and methylmalonic acid in B12 deficiency | |||
*Increased homocysteine in folate defiency | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
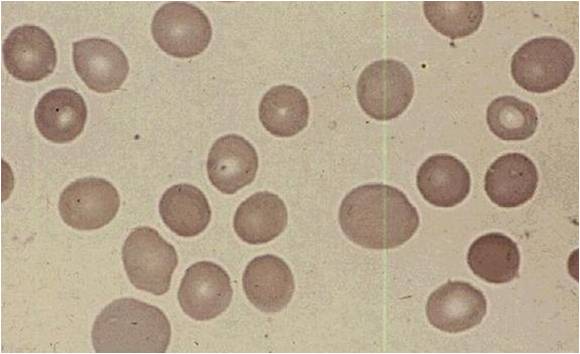
Image:Peripheral blood in megaloblastic anemia 0001.jpg|Peripheral blood in megaloblastic anemia | |||
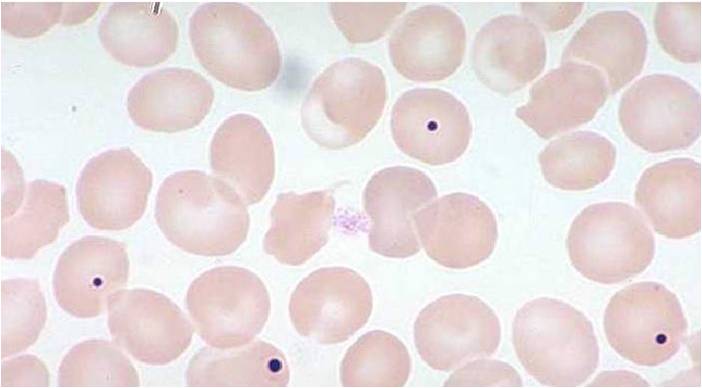
Image:Howell-Jolly bodies 0001.jpg|Howell-Jolly bodies | |||
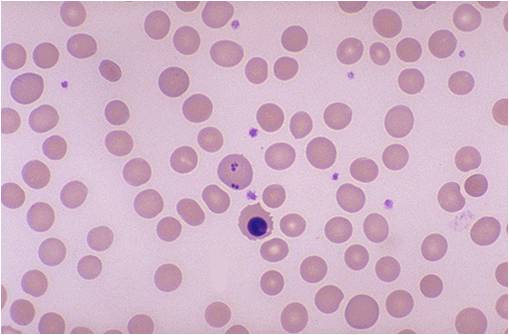
Image:Howell-Jolly bodies and erythroblast.jpg|Howell-Jolly bodies and erythroblast | |||
</gallery> | |||
</div> | |||
==References== | ==References== | ||
Revision as of 14:44, 21 September 2012
|
Macrocytic anemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Macrocytic anemia laboratory findings On the Web |
|
American Roentgen Ray Society Images of Macrocytic anemia laboratory findings |
|
Risk calculators and risk factors for Macrocytic anemia laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Macrocytosis is the enlargement of red blood cells with near-constant haemoglobin concentration, and is defined by a mean corpuscular volume (MCV) of greater than 100 femtolitres (the precise criterion varies between laboratories).
Laboratory diagnosis
- Measurement of homocysteine and Methyl malanoic acid can help confirm and differentiate from folate deficiency.
- Both are elevated in B12 deficiency while only homocysteine is elevate in folate deficiency.
- If PA is based on low serum level, Anti-IF antibodies are confirmatory but only present in 50%.
- Anti-pareital cell Abs are more sensitive (90%) but less specific.
Schilling Test
- Dietary B12 is bound to factors that are cleaved off by acid leaving B12 free to bind to R factors secreted by the saliva and gastric juice.
- B12 bound to R factor is not absorbed, but instead requires the alkaline pancreatic secretions and proteases in the duodenum to be freed from R factor.
- Free B12 can then bind to IF where it is transported to the ileum where a specific receptor then takes up the complex. Therefore, normal B12 absorption and action are dependent of 5 things:
- Dietary intake
- Acid in the stomach
- Pancreatic secretions
- Secretion of IF by Gastric parietal cells
- An ileum that can absorb the IF-B12 complex
- The Schilling test is designed to test the different components of this system.
- First, 1mg IM B12 is given to saturate transcobalmin.
- Radiolabeled B12 is then given orally.
- If it can be absorbed, then >9% will be excreted in the urine in 24 hours and the rest is eliminated in the feces undetected.
- Renal insufficiency causes a falsely low level.
- It may be spuriously normal in patients without gastrectomy.
- Since, acid is required to free dietary B12 from binding factors.
- Radiolabeled b12 is not bound to these factors. Therefore, persons with impaired acid and pepsin production can absorb too little dietary B12, but will absorb free B12 normally.
- Part two of the Schilling test is administering radiolabeled b12 with OF to see if the problem corrects. This should differentiate PA from those with intestinal malabsorption. Remember, B12 deficiency affects the intestinal mucosal cells and causes malabsorption. Therefore, Part II should only be done 4 weeks after replacement, giving the mucosa time to regenerate in PA.
- If Part II is abnormal, Part III is basically a repeat of Part I after a course of antibiotics/vermicides.
- If this is abnormal, an malabsorptive cause is implicated.
Hematological findings
MCV is often >110. Hct can often be as low as 15. Elevated LDH and bilirubin are seen since dyserythopoesis leads to destruction of >90% of RBC precursors. Hypersegmentation of PMNs is quite sensitive (>5% with 5 or more lobes or >1% with 6 lobes). Reticulocyte, WBC and platelets are low to normal. In one series of patients with B12 deficiency, 64% had a MCV greater than 100, and only 29% had anemia. In general the blood film can point towards vitamin deficiency:
- Decreased red blood cell (RBC) count and hemoglobin levels
- Increased mean corpuscular volume (MCV >95 fl often >110) and mean corpuscular hemoglobin (MCH)
- The reticulocyte count is normal
- The platelet count may be reduced.
- Neutrophil granulocytes may show multisegmented nuclei ("senile neutrophil"). This is thought to be due to decreased production and a compensatory prolonged lifespan for circulating neutrophils.
- Anisocytosis (increased variation in RBC size) and poikilocytosis (abnormally shaped RBCs).
- Macrocytes (larger than normal RBCs) are present.
- Ovalocytes (oval shaped RBCs) are present.
- Bone marrow (not normally checked in a patient suspected of megaloblastic anemia) shows megaloblastic hyperplasia.
- Howell-Jolly bodies (chromosomal remnant) also present.
Blood chemistries will also show:
- Increased homocysteine and methylmalonic acid in B12 deficiency
- Increased homocysteine in folate defiency
References
gl:Anemia megaloblástica he:אנמיה מגלובלסטית it:Anemia megaloblastica sl:Megaloblastna anemija sr:Мегалобластна анемија