Nephrologic Disorders and COVID-19: Difference between revisions
Jump to navigation
Jump to search
| Line 24: | Line 24: | ||
====Clinical Features of AKI by SARS-CoV-2==== | ====Clinical Features of AKI by SARS-CoV-2==== | ||
====Treatment==== | ====Treatment==== | ||
*Management of [[AKI]] following [[COVID-19]] includes treatment of infection, identifying electrolyte disorders, and [[intravenous fluid]] administration. | |||
*Treatment of [[AKI]] following [[COVID-19]] includes<ref name="pmid32416769">{{cite journal| author=Ronco C, Reis T, Husain-Syed F| title=Management of acute kidney injury in patients with COVID-19. | journal=Lancet Respir Med | year= 2020 | volume= | issue= | pages= | pmid=32416769 | doi=10.1016/S2213-2600(20)30229-0 | pmc=7255232 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32416769 }} </ref>: | |||
**Correction of hypovolemia and hypotension by the administration of adequate [[intravenous fluid]] | |||
**Correction of electrolyte disturbances | |||
**[[Renal Replacement Therapy]] | |||
***If AKI is unresponsive to conservative therapy | |||
***In volume overload conditions | |||
***Modality of choice in unstable hemodynamic status | |||
**Anticoagulants in hypercoagulable conditions | |||
**Sequential extracorporeal therapy | |||
Revision as of 02:54, 22 June 2020
To go to the COVID-19 project topics list, click here.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sogand Goudarzi, MD [2] Nasrin Nikravangolsefid, MD-MPH [3]
Overview
Nephrologic_Disorders of COVID-19
Nephrologic_Disorders risk factors of COVID-19
Complications
AKI
Pathophysiology
- Angiotensin-converting enzyme 2 (ACE2), which is a primary receptor for SARS-CoV-2 entry into cells, mostly presents in renal tubular epithelial cells as well as lungs and heart.[1]
- Despite kidney injury following COVID-19 infection is less frequent than severe lung injury, ACE2: ACE ratio is higher in the kidneys compared to the respiratory system. (1:1 in the kidneys VS 1:20 in the respiratory system)[1]
- After SARS-CoV-2 enters through the nasal cavity, it may travel to the kidneys and enters the bloodstream leading to severe inflammatory response activation and cytokine storm.
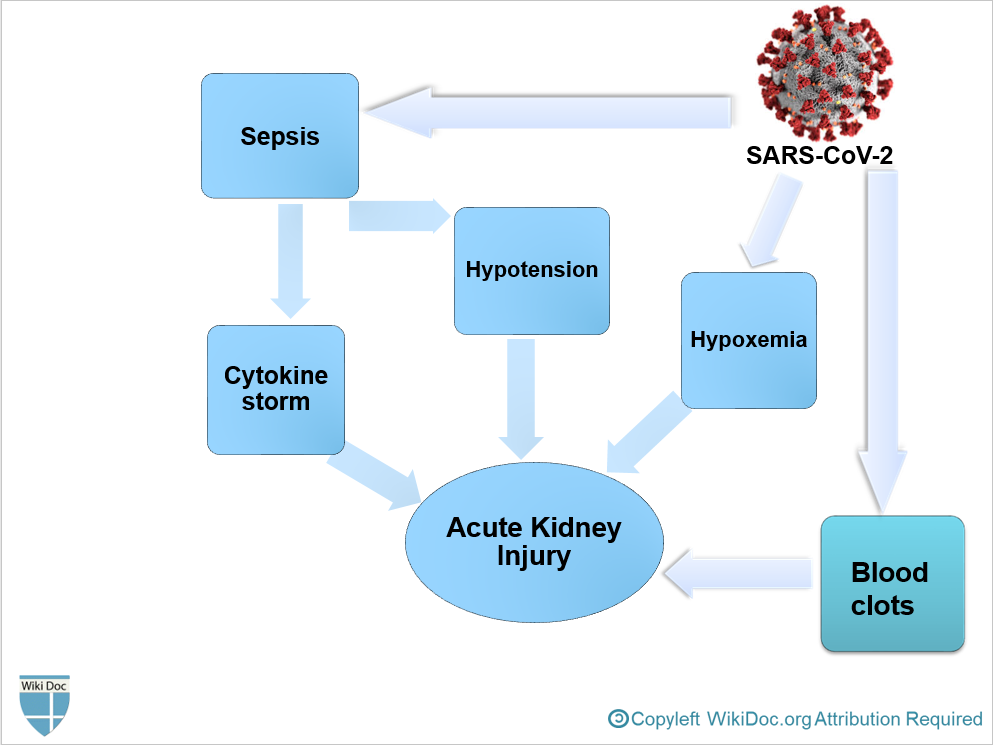
- It is thought that AKI following COVID-19 is the result of[1]
- Sepsis
- Hypovolemia and Hypotension
- Hypoxemia
- Blood clots formation, leading to impaired blood flow in the renal arterioles.
- AKI often occurs at later stages in critically ill patients with COVID-19 following multiple organ failure.
Clinical Features of AKI by SARS-CoV-2
Treatment
- Management of AKI following COVID-19 includes treatment of infection, identifying electrolyte disorders, and intravenous fluid administration.
- Treatment of AKI following COVID-19 includes[2]:
- Correction of hypovolemia and hypotension by the administration of adequate intravenous fluid
- Correction of electrolyte disturbances
- Renal Replacement Therapy
- If AKI is unresponsive to conservative therapy
- In volume overload conditions
- Modality of choice in unstable hemodynamic status
- Anticoagulants in hypercoagulable conditions
- Sequential extracorporeal therapy
- ↑ 1.0 1.1 1.2 Malha, Line; Mueller, Franco B.; Pecker, Mark S.; Mann, Samuel J.; August, Phyllis; Feig, Peter U. (2020). "COVID-19 and the Renin-Angiotensin System". Kidney International Reports. 5 (5): 563–565. doi:10.1016/j.ekir.2020.03.024. ISSN 2468-0249.
- ↑ Ronco C, Reis T, Husain-Syed F (2020). "Management of acute kidney injury in patients with COVID-19". Lancet Respir Med. doi:10.1016/S2213-2600(20)30229-0. PMC 7255232 Check
|pmc=value (help). PMID 32416769 Check|pmid=value (help).