Sandbox:Cherry: Difference between revisions
No edit summary |
|||
| Line 10: | Line 10: | ||
{{CMG}} {{AE}} | {{CMG}} {{AE}} | ||
== Indications of Liver transplanatation== | == Indications of Liver transplanatation== | ||
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4486032/ | |||
Indications | Indications | ||
The most common indications for liver transplantation in the United States are: | The most common indications for liver transplantation in the United States are: | ||
| Line 39: | Line 41: | ||
Biologic Model for End-stage Liver Disease (MELD) score is ≥15 | Biologic Model for End-stage Liver Disease (MELD) score is ≥15 | ||
Cases of Child B cirrhosis with portal hypertension but a low MELD score | Cases of Child B cirrhosis with portal hypertension but a low MELD score | ||
| Line 131: | Line 132: | ||
Portal hypertensive gastropathy leading to chronic blood loss | Portal hypertensive gastropathy leading to chronic blood loss | ||
Recurrent cholangitis in patients with PSC | Recurrent cholangitis in patients with PSC | ||
| Line 455: | Line 454: | ||
===Image and text to the right=== | ===Image and text to the right=== | ||
<figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>[[File:Global distribution of leptospirosis.jpg|577x577px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017. | <figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>[[File:Global distribution of leptospirosis.jpg|577x577px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017. | ||
===Gallery=== | ===Gallery=== | ||
Revision as of 15:45, 11 January 2018
Pathophysiology prev
| https://https://www.youtube.com/watch?v=5szNmKtyBW4%7C350}} |
|
Cirrhosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case studies |
|
Sandbox:Cherry On the Web |
|
American Roentgen Ray Society Images of Sandbox:Cherry |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief:
Indications of Liver transplanatation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4486032/
Indications The most common indications for liver transplantation in the United States are:
Hepatitis C virus (30%) Alcoholic liver disease (18%) Idiopathic/autoimmune liver disease (12%) Primary biliary cirrhosis (10%) Primary sclerosing cholangitis (8%)
Acute liver failure : Severe acute liver injury with impaired synthetic function of the liver(INR ≥1.5) and encephalopathy in the absence of pre existing liver disease or cirrhosis Common causes: viral, drug-induced Highest priority for liver transplantation, immediate referral to transplantation centre, May recover or die
Cirrhosis: Only in cases of complications such as portal hypertension, or compromised hepatic function( marker for impaired survival) Signs of decompensated cirrhosis include: Ascites Encephalopathy Variceal haemorrhage Hepatorenal syndrome Transplanatation evaluation is commenced in patients with MELD score >10: Gives the patient time for pre transplanatation evaluation Education before the development of symptoms of hepatic encephalopathy
Patients with cirrhosis are candidates for liver transplantation in the following scenarios: Biologic Model for End-stage Liver Disease (MELD) score is ≥15 Cases of Child B cirrhosis with portal hypertension but a low MELD score
Hepatitis B virus Metabolic liver disease (eg, inborn errors of metabolism) Cancer
Biliary atresia
INDICATIONS MELD exception points are given to patients with pathologies that may impair survival without impacting the MELD score such as: Cancer: HCC, Hilar cholangiocarcinoma Complications of cirrhosis: Hepatopulmonary syndrome, Portopulmonary hypertension Vascular pathologies: Hepatic artery thrombosis Cystic fibrosis Primary hyperoxaluria Familial amyloid polyneuropathy Other conditions that may also be indications for transplantation that do not qualify for MELD or MELD exception points include: Intractable pruritus in case of primary biliary cirrhosis Refractory variceal haemorrhage Refractory ascites Refractory hepatic encephalopathy Portal hypertensive gastropathy leading to chronic blood loss Recurrent cholangitis in patients with PSC Liver neoplasms — HCC: a single lesion ≤5 cm or up to three separate lesions all <3 cm, no evidence of gross vascular invasion, and no regional nodal or distant metastases). In addition, there may be a role for liver transplantation in patients with neuroendocrine tumors that have metastasized to the liver, but experience in this setting is limited. Some of the liver neoplasms that have been treated with liver transplantation include : HCC (including fibrolamellar HCC) Epithelioid hemangioendothelioma Large hepatic adenomas Metabolic disorders — Several liver-based metabolic conditions with systemic manifestations may be treated with liver transplantation. In some cases (eg, alpha-1 antitrypsin deficiency and Wilson disease), patients are cured of the underlying disease with liver transplantation, though some clinical manifestations may not be reversible. Liver-based metabolic conditions that have been treated with liver transplantation include: Alpha-1 antitrypsin deficiency Some forms of glycogen storage disease (type I and type IV) Tyrosinemia Hemochromatosis Wilson disease Acute intermittent porphyria
Overview
Indications The most common indications for liver transplantation in the United States are:
Hepatitis C virus (30%) Alcoholic liver disease (18%) Idiopathic/autoimmune liver disease (12%) Primary biliary cirrhosis (10%) Primary sclerosing cholangitis (8%)
Acute liver failure : Severe acute liver injury with impaired synthetic function of the liver(INR ≥1.5) and encephalopathy in the absence of pre existing liver disease or cirrhosis Common causes: viral, drug-induced Highest priority for liver transplantation, immediate referral to transplantation centre, May recover or die
Cirrhosis: Only in cases of complications such as portal hypertension, or compromised hepatic function( marker for impaired survival) Signs of decompensated cirrhosis include: Ascites Encephalopathy Variceal haemorrhage Hepatorenal syndrome Transplanatation evaluation is commenced in patients with MELD score >10: Gives the patient time for pre transplanatation evaluation Education before the development of symptoms of hepatic encephalopathy
Patients with cirrhosis are candidates for liver transplantation in the following scenarios: Biologic Model for End-stage Liver Disease (MELD) score is ≥15 Cases of Child B cirrhosis with portal hypertension but a low MELD score
Hepatitis B virus Metabolic liver disease (eg, inborn errors of metabolism) Cancer Biliary atresia
INDICATIONS MELD exception points are given to patients with pathologies that may impair survival without impacting the MELD score such as: Cancer: HCC, Hilar cholangiocarcinoma Complications of cirrhosis: Hepatopulmonary syndrome, Portopulmonary hypertension Vascular pathologies: Hepatic artery thrombosis Cystic fibrosis Primary hyperoxaluria Familial amyloid polyneuropathy Other conditions that may also be indications for transplantation that do not qualify for MELD or MELD exception points include: Intractable pruritus in case of primary biliary cirrhosis Refractory variceal haemorrhage Refractory ascites Refractory hepatic encephalopathy Portal hypertensive gastropathy leading to chronic blood loss Recurrent cholangitis in patients with PSC
Liver neoplasms —
HCC: a single lesion ≤5 cm or up to three separate lesions all <3 cm, no evidence of gross vascular invasion, and no regional nodal or distant metastases). In addition, there may be a role for liver transplantation in patients with neuroendocrine tumors that have metastasized to the liver, but experience in this setting is limited. Some of the liver neoplasms that have been treated with liver transplantation include :
HCC (including fibrolamellar HCC)
Epithelioid hemangioendothelioma
Large hepatic adenomas
Metabolic disorders — Several liver-based metabolic conditions with systemic manifestations may be treated with liver transplantation. In some cases (eg, alpha-1 antitrypsin deficiency and Wilson disease), patients are cured of the underlying disease with liver transplantation, though some clinical manifestations may not be reversible.
Liver-based metabolic conditions that have been treated with liver transplantation include:
Alpha-1 antitrypsin deficiency
Some forms of glycogen storage disease (type I and type IV)
Tyrosinemia
Hemochromatosis
Wilson disease
Acute intermittent porphyria
source
Liver transplantation is an important treatment option for patients with acute liver failure, end-stage liver disease, and primary hepatic malignancy, though it is not the initial or primary treatment modality for most liver diseases.
Transplantation infrequently cures the underlying disease; recurrent liver disease after transplantation occurs in 0 to 100 percent of patients, depending on the disease for which transplantation was performed. Thus, the decision to list a patient for transplantation is a risk-benefit analysis in which the inherent risks of surgery, recurrent disease, and long-term immunosuppression must be weighed against the potential benefits of transplantation. These benefits differ for each patient but include improvements in survival, prevention of long-term complications, and better health-related quality of life. In most cases, the risks associated with recurrent disease do not outweigh the benefits of liver transplantation.
This topic will review the selection of patients for liver transplantation and the pretransplantation evaluation. Other issues related to liver transplantation including donor selection, living donor liver transplantation, ethical issues in liver transplantation, immunosuppression following liver transplantation, and the medical management of patients who have undergone liver transplantation are discussed elsewhere. (See "Liver transplantation: Donor selection" and "Living donor liver transplantation" and "Ethical issues in liver transplantation" and "Liver transplantation in adults: Overview of immunosuppression" and "Liver transplantation in adults: Long-term management of transplant recipients".)
In 2013, the American Association for the Study of Liver Diseases and the American Society of Transplantation developed guidelines regarding the indications for liver transplantation and the evaluation of patients being considered for liver transplantation [1]. The discussion that follows is generally consistent with those guidelines.
FREQUENCY OF LIVER TRANSPLANTATION BY UNDERLYING LIVER DISEASE — According to the United Network for Organ Sharing/Organ Procurement and Transplantation Network registry, hepatocellular carcinoma and hepatitis C virus cirrhosis are the most common diseases leading to liver transplantation, although increasing numbers of patients with alcoholic cirrhosis and nonalcoholic steatohepatitis are receiving transplants [2]. For additional information, see optn.transplant.hrsa.gov/data/view-data-reports. INDICATIONS
Acute liver failure — Patients with acute liver failure are given the highest priority for liver transplantation (United Network for Organ Sharing [UNOS] status 1). In the absence of liver transplantation, patients with acute liver failure will either have a complete recovery of liver function or will die [3]. However, because it can be difficult to predict whether a given patient will recover, patients with acute liver failure should be referred to a liver transplantation center as soon as possible. (See "Acute liver failure in adults: Management and prognosis", section on 'Liver transplantation'.)
Acute liver failure is defined by the development of severe acute liver injury with encephalopathy and impaired synthetic function (international normalized ratio [INR] of ≥1.5) in a patient without cirrhosis or preexisting liver disease. While the time course that differentiates acute liver failure from chronic liver failure varies between reports, a commonly used cutoff is an illness duration of <26 weeks. While there are numerous causes of acute liver failure (table 1), viral and drug-induced hepatitis are the most common causes of acute liver failure in adults. (See "Acute liver failure in adults: Etiology, clinical manifestations, and diagnosis".)
Cirrhosis — The presence of cirrhosis alone is not sufficient to warrant transplantation. Transplantation is generally considered when a patient has suffered either a complication of portal hypertension or a manifestation of compromised hepatic function [1]. Variceal hemorrhage, ascites, and encephalopathy are the primary manifestations of end-stage liver disease and are designated as markers of decompensation. The onset of decompensation is associated with significantly impaired survival. Another complication of cirrhosis is the development of hepatorenal syndrome, which is an ominous marker and signals the need for immediate transplantation evaluation. (See "Cirrhosis in adults: Overview of complications, general management, and prognosis".)
Patients with cirrhosis are typically candidates for liver transplantation once their biologic Model for End-stage Liver Disease (MELD) score is ≥15 (calculator 1 and calculator 2). However, some patients with Child B cirrhosis (table 2) with portal hypertension but a low MELD score may be candidates for liver transplantation. The transplantation evaluation is typically started once a patient has a MELD score >10. This permits the patient to meet the transplantation team prior to the development of end-stage liver disease and ensures adequate time for the patient to complete the pretransplantation evaluation. If patients are referred for evaluation once end-stage liver disease has developed, there may not be adequate time for education, and the patient may have impaired mental status from underlying encephalopathy. (See "Model for End-stage Liver Disease (MELD)", section on 'Prioritization for liver transplantation based on MELD score'.)
Patients may also qualify for liver transplantation if they have a complication or condition that qualifies for standard MELD exception points. Exception points are awarded because there are some conditions associated with chronic liver disease that may result in impaired survival but are not directly accounted for in the MELD scoring system. Conditions that qualify for MELD exception points include. (See "Model for End-stage Liver Disease (MELD)", section on 'Standard MELD exceptions in liver transplantation'.):
●Hepatocellular carcinoma.
●Hepatopulmonary syndrome.
●Portopulmonary hypertension (provided the mean arterial pressure can be maintained at <35 mmHg with treatment).
●Familial amyloid polyneuropathy.
●Primary hyperoxaluria.
●Cystic fibrosis.
●Hilar cholangiocarcinoma (provided the liver transplantation center has a UNOS-approved protocol detailing the work-up and management of patients with cholangiocarcinoma undergoing transplantation).
●Hepatic artery thrombosis (occurring within 14 days of liver transplantation but not meeting criteria for status 1A).
Finally, patients may have complicating medical conditions that are related to their liver disease but that do not qualify for standard MELD exception points. Such patients can be considered for liver transplantation if their medical providers believe that the biologic MELD score does not adequately reflect a patient's true liver-related morbidity and mortality or if the complications are severely impairing the patient's quality of life. Some of these complications include (see "Model for End-stage Liver Disease (MELD)", section on 'Petitioning for additional MELD points'):
●Recurrent cholangitis in patients with primary sclerosing cholangitis who are on antibiotic suppressive therapy or require repeated biliary interventions
●Refractory ascites
●Refractory hepatic encephalopathy
●Refractory variceal hemorrhage
●Portal hypertensive gastropathy leading to chronic blood loss
●Intractable pruritus in a patient with primary biliary cirrhosis
Liver neoplasms — Patients with some primary liver neoplasms may be candidates for liver transplantation, provided the neoplasms meet specific criteria (eg, for patients with hepatocellular carcinoma [HCC], a single lesion ≤5 cm or up to three separate lesions all <3 cm, no evidence of gross vascular invasion, and no regional nodal or distant metastases). In addition, there may be a role for liver transplantation in patients with neuroendocrine tumors that have metastasized to the liver, but experience in this setting is limited [4]. (See "Metastatic gastroenteropancreatic neuroendocrine tumors: Local options to control tumor growth and symptoms of hormone hypersecretion", section on 'Liver transplantation'.)
Some of the liver neoplasms that have been treated with liver transplantation include [4]:
●HCC (including fibrolamellar HCC) (see "Liver transplantation for hepatocellular carcinoma" and "Epidemiology, clinical manifestations, diagnosis, and treatment of fibrolamellar carcinoma", section on 'Liver transplantation')
●Epithelioid hemangioendothelioma [5-7]
●Large hepatic adenomas (see "Hepatic adenoma", section on 'Symptomatic patients and those with large adenomas')
Metabolic disorders — Several liver-based metabolic conditions with systemic manifestations may be treated with liver transplantation. In some cases (eg, alpha-1 antitrypsin deficiency and Wilson disease), patients are cured of the underlying disease with liver transplantation, though some clinical manifestations may not be reversible.
Liver-based metabolic conditions that have been treated with liver transplantation include:
●Familial amyloid polyneuropathy (qualifies for standard MELD exception points) [8-10].
●Primary hyperoxaluria (qualifies for standard MELD exception points) (see "Primary hyperoxaluria", section on 'Transplantation').
●Cystic fibrosis (qualifies for standard MELD exception points) (see "Cystic fibrosis: Hepatobiliary disease", section on 'Management').
●Alpha-1 antitrypsin deficiency [11,12].
●Some forms of glycogen storage disease (type I and type IV) (see "Glucose-6-phosphatase deficiency (glycogen storage disease I, von Gierke disease)", section on 'Liver transplantation' and "Glycogen branching enzyme deficiency (glycogen storage disease IV, Andersen disease)", section on 'Treatment').
●Tyrosinemia (see "Disorders of tyrosine metabolism", section on 'Liver transplantation').
●Hemochromatosis [13,14].
●Wilson disease (see "Wilson disease: Treatment and prognosis", section on 'Liver transplantation').
●Acute intermittent porphyria (see "Management and prognosis of acute intermittent porphyria", section on 'Liver transplantation').
In the case of alpha-1 antitrypsin deficiency, cystic fibrosis, tyrosinemia, hemochromatosis, and Wilson disease, liver transplantation is usually reserved for patients who have developed end-stage liver disease or HCC.
CONTRAINDICATIONS — Although organ allocation is centralized, criteria and contraindications to listing for liver transplantation are often transplantation center-specific. General contraindications adopted by most centers include [1]:
●Cardiopulmonary disease that cannot be corrected and is a prohibitive risk for surgery
●Acquired immunodeficiency syndrome (AIDS)
●Malignancy outside of the liver not meeting oncologic criteria for cure
●Hepatocellular carcinoma with metastatic spread
●Intrahepatic cholangiocarcinoma
●Hemangiosarcoma
●Anatomic abnormalities that preclude liver transplantation
●Uncontrolled sepsis
●Acute liver failure with a sustained intracranial pressure >50 mmHg or a cerebral perfusion pressure <40 mmHg
●Persistent nonadherence with medical care
●Lack of adequate social support
For patients with alcoholic liver disease, most programs require a minimum period of abstinence of at least six months, participation in a structured rehabilitation and abstinence program, and adequate social support to help maintain sobriety. Experimental programs in Europe have transplanted selected patients with acute alcoholic hepatitis who are unlikely to survive for six months, but this is not commonly done [15]. (See "Management and prognosis of alcoholic hepatitis", section on 'Liver transplantation' and "Liver transplantation for alcoholic liver disease", section on 'Pre-transplant abstinence and monitoring'.)
Advanced age and human immunodeficiency virus (HIV) (but not AIDS) are examples of relative contraindications that are site-specific and are often decided on a case-by-case basis. Liver transplantation can be performed in those older than 65 years of age, provided that there has been a comprehensive evaluation for comorbidities [16].
Several transplantation centers in the United States and Europe are now performing liver transplantations in patients with HIV [17-24], and studies suggest good outcomes in patients who are not coinfected with hepatitis C virus (HCV) [25-27]. Our approach is to list patients with HIV for transplantation if they meet other criteria. We do not exclude patients with HCV since new treatments for HCV improve outcomes following transplantation. (See "Recurrence of hepatitis C virus infection following liver transplantation".)
Patients with class 3 obesity (body mass index [BMI] ≥40) have worse outcomes following liver transplantation, and some centers consider it a relative contraindication to transplantation [1]. Patients who are obese should be encouraged to lose weight prior to liver transplantation. Whether patients with high BMI should be excluded from transplantation and what cutoff should be used (BMI >40, >50) remains controversial, and some centers will perform a gastric sleeve before or at the time of transplantation.
PRETRANSPLANTATION EVALUATION — The goal of the pretransplantation evaluation is to assess the patient's ability to tolerate the stress of surgery, immunosuppression, and the demands of post-transplantation care. Thus, each patient undergoes an extensive cardiopulmonary evaluation, screening for occult infection or cancer, and psychosocial evaluation (table 3). Specific testing varies depending on the patient's age, medical history, and transplantation center practice. In addition, while a certain battery of tests may initiate the work-up, more testing may be indicated if the initial test results are abnormal or if the patient has signs or symptoms of a significant comorbid illness that is not evaluated as part of the initial evaluation.
Laboratory testing — Laboratory tests that should be obtained in patients being evaluated for liver transplantation include:
●ABO-Rh blood typing.
●Liver biochemical and function tests (alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, bilirubin, international normalized ratio [INR]).
●Complete blood count with differential.
●Creatinine clearance.
●Serum sodium.
●Serum alpha-fetoprotein.
●Calcium and vitamin D levels.
●Serologies for cytomegalovirus, Epstein-Barr virus, varicella, human immunodeficiency virus, hepatitis A, hepatitis B, hepatitis C, rapid plasma reagin.
●Urinalysis.
●Urine drug screen.
Cardiopulmonary evaluation — The cardiopulmonary evaluation is designed to evaluate for significant coronary artery disease, valvular heart disease, cardiomyopathy, obstructive or restrictive lung disease, hepatopulmonary syndrome, and pulmonary hypertension [1,28-30]. There are some nuances in cardiac evaluation (reduced afterload, hyperdynamic circulation, etc.) that need to be taken into account in patients with cirrhosis to ensure that the work-up is appropriately vigorous. Some findings discovered during initial testing may permanently preclude transplantation, whereas others may need to be treated or corrected prior to surgery.
We obtain noninvasive cardiac testing for all patients over 40 years of age and for those younger than forty if there are multiple risk factors for coronary artery disease. We obtain pulse oximetry and an arterial blood gas in all patients. We also perform pulmonary function testing in all patients who are able to undergo the testing. In patients who are unable to undergo testing, pulmonary function is assessed based on the patient's history, physical exam, arterial blood gas, and chest imaging.
Morbidity and mortality from liver transplantation are increased in patients with coronary artery disease [31] or those with severe hypoxemia and elevated mean pulmonary artery pressure measurements [32,33]. However, the risk of poor outcomes does not appear to be increased in patients with mild to moderate pulmonary hypertension (pulmonary artery systolic pressure between 40 and 59 mmHg) [34]. (See "Liver transplantation in adults: Long-term management of transplant recipients", section on 'Cardiovascular risk' and "Management of cardiac risk for noncardiac surgery".)
Electrocardiogram — We obtain an electrocardiogram to look for signs of cardiac arrhythmias, conduction defects, signs of prior cardiac ischemia, or chamber enlargement/hypertrophy. (See "ECG tutorial: Basic principles of ECG analysis".)
Cardiac stress testing — To screen for coronary artery disease, we obtain noninvasive cardiac testing for all patients over 40 years of age and for those younger than 40 years if there are multiple risk factors for coronary artery disease. (See "Stress testing for the diagnosis of obstructive coronary heart disease".)
However, the ideal evaluation of coronary artery disease prior to liver transplantation is unclear:
●In 2012, the American Heart Association and the American College of Cardiology Foundation suggested noninvasive stress testing in liver transplantation candidates with no active cardiac conditions if there are multiple (three or more) risk factors for coronary artery disease present (eg, diabetes, prior cardiovascular disease, left ventricular hypertrophy, age greater than 60 years, smoking, hypertension, or dyslipidemia) [35]. (See "Overview of established risk factors for cardiovascular disease", section on 'Established risk factors for atherosclerotic CVD'.)
●In 2013 practice guidelines, the American Association for the Study of Liver Diseases and the American Society of Transplantation recommend noninvasive cardiac testing (either exercise stress testing or pharmacologic stress testing) for all adults being evaluated for liver transplantation [1].
●Some cardiologists recommend that patients with known coronary artery disease, diabetes mellitus, or more than two cardiovascular risk factors undergo coronary angiography to assess the extent and severity of coronary artery disease [36].
Another method that is being studied for pretransplant evaluation is submaximal cardiopulmonary exercise testing. One study found that the calculated anaerobic threshold (which corresponds with cardiorespiratory reserve) predicted post-transplantation mortality [37]. Survivors of liver transplantation had higher mean anaerobic thresholds than patients who did not survive (12.0 versus 8.4 mL/min/kg). This method of pretransplantation evaluation is not currently in widespread use. (See "Functional exercise testing: Ventilatory gas analysis", section on 'Ventilatory anaerobic threshold determination'.)
If initial noninvasive testing is abnormal, cardiac catheterization is indicated. If clinically significant coronary artery stenoses are present, patients should be evaluated for revascularization prior to transplantation. (See "Use of intracoronary stents for specific coronary lesions" and "Management of left main coronary artery disease" and "Management of significant proximal left anterior descending coronary artery disease".)
Echocardiography — We obtain transthoracic contrast-enhanced echocardiography to look for evidence of valvular heart disease or portopulmonary hypertension. Contrast-enhanced echocardiography is also part of the evaluation of patients with suspected hepatopulmonary syndrome. (See 'Pulse oximetry' below and "Echocardiographic evaluation of the aortic valve" and "Echocardiographic evaluation of the mitral valve" and "Echocardiographic evaluation of the tricuspid valve" and "Echocardiographic evaluation of the pulmonic valve and pulmonary artery" and "Portopulmonary hypertension", section on 'Diagnostic evaluation'.)
Portopulmonary hypertension refers to pulmonary arterial hypertension that is associated with portal hypertension. Symptoms and signs of pulmonary hypertension (PH) may be difficult to recognize because they are nonspecific. Initially, patients present with fatigue, exertional dyspnea and a loud pulmonic component of the second heart sound. If the echocardiography suggests PH, additional testing is required to confirm the diagnosis and to rule out other causes of PH. (See "Portopulmonary hypertension", section on 'Diagnostic evaluation'.)
Pulse oximetry — Patients should undergo pulse oximetry to screen for hepatopulmonary syndrome. Hepatopulmonary syndrome is considered present when the following triad exists:
●Liver disease
●Impaired oxygenation
●Intrapulmonary vascular abnormalities, referred to as intrapulmonary vascular dilatations
The presence of hepatopulmonary syndrome worsens the prognosis of patients with cirrhosis. As a result, patients with hepatopulmonary syndrome receive standard Model for End-stage Liver Disease (MELD) exception points. If the oxygen saturation on pulse oximetry is low (<96 percent [38]), patients should have a blood gas obtained while breathing room air and undergo transthoracic contrast-enhanced echocardiography. Testing should also be obtained to rule out alternative causes for a low oxygen saturation. Testing to rule out other causes includes a chest radiograph, pulmonary function tests, and chest computed tomography (CT). (See "Hepatopulmonary syndrome in adults: Prevalence, causes, clinical manifestations, and diagnosis", section on 'Diagnostic evaluation' and "Model for End-stage Liver Disease (MELD)", section on 'Standard MELD exceptions in liver transplantation'.)
We also perform an arterial blood gas in patients with normal pulse oximetry to calculate their age-adjusted alveolar-arterial gradient (calculator 3).
Additional testing for pulmonary disease — We obtain pulmonary function testing with diffusing capacity of the lungs for carbon monoxide to look for evidence of restrictive or obstructive lung disease in patients who are able to undergo testing. We also obtain a chest radiograph and chest CT scan to look for signs of pulmonary disease. (See "Overview of pulmonary function testing in adults", section on 'Pulmonary function tests'.)
Cancer screening — Cancer screening should include abdominal CT scanning or magnetic resonance imaging (MRI) to look for hepatocellular carcinoma (HCC) and a skin examination to look for evidence of skin cancer. Patients over the age of 50 years (younger if there is a history of colon cancer in a first-degree relative) or who have primary sclerosing cholangitis should undergo colonoscopy. Screening for cervical cancer, breast cancer, and prostate cancer should be obtained when indicated based on the patient's sex and age. (See "Screening for colorectal cancer in patients with a family history of colorectal cancer" and "Screening for cervical cancer" and "Screening for breast cancer: Strategies and recommendations" and "Screening for prostate cancer".)
Infectious disease evaluation and vaccinations — In addition to obtaining serologies for several viral infections, the infectious disease evaluation should include skin testing or interferon-gamma release assay for tuberculosis. If positive, treatment may be initiated prior to transplantation or deferred until after transplantation, depending on the clinical assessment of the patient (eg, treatment should be initiated prior to transplantation if the patient has any signs or symptoms of tuberculosis). Similarly, any required dental extractions should be carried out prior to transplantation. Patients from endemic areas should be screened for coccidiomycosis or strongyloides. (See "Treatment of latent tuberculosis infection in HIV-uninfected adults" and "Primary coccidioidal infection", section on 'Epidemiology' and "Strongyloidiasis", section on 'Epidemiology'.)
Several vaccinations are recommended prior to liver transplantation including hepatitis A, hepatitis B, pneumococcus, influenza, diphtheria, pertussis, and tetanus. Immunizations in solid organ transplantation candidates are discussed in detail elsewhere. (See "Immunizations in solid organ transplant candidates and recipients".)
Hepatic imaging and HCC staging — Hepatic imaging should be obtained to assess the vasculature (to ensure there are no anatomic barriers to transplantation) and, in the case of HCC, for tumor staging. This is typically done with multiphase contrast-enhanced CT scanning or contrast-enhanced MRI. If cross-sectional imaging cannot be obtained, the hepatic vasculature can be assessed with transabdominal ultrasonography with Doppler imaging or contrast-enhanced ultrasonography (where available). (See "Staging and prognostic factors in hepatocellular carcinoma", section on 'Staging and prognostic scoring systems' and "Contrast-enhanced ultrasound for the evaluation of liver lesions", section on 'Liver transplantation'.)
Upper endoscopy — Upper endoscopy should be performed in patients with cirrhosis or portal hypertension to evaluate for varices. (See "Primary and pre-primary prophylaxis against variceal hemorrhage in patients with cirrhosis", section on 'Screening for varices'.)
Bone density testing — Patients should be screened for osteoporosis with bone density testing. If osteoporosis is present, treatment should be initiated prior to transplantation. Oral bisphosphonates should be used with caution in patients with esophageal varices, and patients should be aware of the importance of taking the drugs as instructed (eg, sitting upright for at least 30 minutes after taking the drug). Patients who are osteopenic should receive calcium and vitamin D supplementation. (See "Overview of the management of osteoporosis in postmenopausal women", section on 'Choice of drug' and "Overview of the management of osteoporosis in postmenopausal women", section on 'Calcium/vitamin D'.)
Psychosocial evaluation and education — In addition to a standard medical evaluation, initial assessment should include an educational session discussing the risks and benefits of transplantation, including the potential for poor outcomes. A psychological evaluation and assessment of the patient's social supports is another key part of the evaluation.
The purpose of this assessment is to identify issues that may impair a successful outcome after transplantation. These potential problems include a lack of insight into the nature of the transplantation procedure, post-transplantation care, and substance use disorders. The assessment includes education of the family and/or the patient's support network. The ability to comply with complex medical and behavioral regimens is crucial after any organ transplantation procedure. Recipients must be able to incorporate complicated medication regimens, follow-up appointments, and frequent laboratory visits into their lives. Making spouses, friends, and family aware of these requirements encourages patient compliance and may improve long-term success. (See "Screening for unhealthy use of alcohol and other drugs in primary care".)
In patients with a history of a substance use disorder (drugs or alcohol), treatment should be provided prior to transplantation in an effort to increase the likelihood of success after transplantation. The treatment requirements vary among different transplantation centers but often include participation in a structured rehabilitation and abstinence program, adequate social support to help maintain sobriety, and a minimum period of sobriety prior to listing for transplantation (eg, six months). (See "Liver transplantation for alcoholic liver disease".)
ADULT LIVING DONOR LIVER TRANSPLANTATION — Adult living donor liver transplantation (LDLT) was initiated in 1998 in response to the growing shortage of organs from deceased donors [39]. Recipients considered for LDLT should fulfill the same minimal listing criteria established for deceased donor liver transplantation. The goal is to avoid premature transplantation. The optimal Model for End-stage Liver Disease (MELD) score at which patients should undergo LDLT has yet to be determined. The optimal MELD score is one that identifies the recipient when the chance of liver disease-related mortality is greater than the chance of mortality from surgical complications. (See "Living donor liver transplantation".)
INFORMATION FOR PATIENTS — UpToDate offers two types of patient education materials, "The Basics" and "Beyond the Basics." The Basics patient education pieces are written in plain language, at the 5th to 6th grade reading level, and they answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10th to 12th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. (You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword(s) of interest.)
●Basics topic (see "Patient education: Liver transplant (The Basics)")
SUMMARY AND RECOMMENDATIONS
●Indications for liver transplantation include acute liver failure, cirrhosis with complications, some liver neoplasms, and liver-based metabolic conditions with systemic manifestations. (See 'Indications' above.)
•Patients with acute liver failure are given the highest priority for liver transplantation and should be referred to a liver transplantation center for evaluation as soon as possible. (See 'Acute liver failure' above.)
•Patients with cirrhosis are typically candidates for liver transplantation once their biologic Model for End-stage Liver Disease (MELD) score is ≥15 (calculator 1 and calculator 2). However, the transplantation evaluation is typically started once a patient has a MELD score >10. This permits the patient to meet the transplantation team prior to developing end-stage liver disease and ensures adequate time for the patient to complete the pretransplantation evaluation. (See 'Cirrhosis' above.)
Patients with cirrhosis may also qualify for liver transplantation if they have a complication that qualifies for standard MELD exception points including hepatocellular carcinoma (HCC), hepatopulmonary syndrome, and portopulmonary hypertension. (See "Model for End-stage Liver Disease (MELD)", section on 'Standard MELD exceptions in liver transplantation'.)
Finally, patients with cirrhosis may be considered for liver transplantation if they have other complications related to cirrhosis such as refractory ascites, though they do not receive standard MELD exception points. (See "Model for End-stage Liver Disease (MELD)", section on 'Petitioning for additional MELD points'.)
•Patients with some primary liver neoplasms (eg, HCC) may be candidates for liver transplantation, provided the neoplasms meet specific criteria. In addition, there may be a role for liver transplantation in patients with neuroendocrine tumors that have metastasized to the liver, but experience in this setting is limited. (See 'Liver neoplasms' above.)
•Liver-based metabolic conditions with systemic manifestations that may be treated with liver transplantation include familial amyloid polyneuropathy, primary hyperoxaluria, and cystic fibrosis. (See 'Metabolic disorders' above.)
●Contraindications to liver transplantation include cardiopulmonary disease that cannot be corrected and is a prohibitive risk for surgery, malignancy outside of the liver not meeting oncologic criteria for cure, metastatic HCC, intrahepatic cholangiocarcinoma, persistent nonadherence with medical care, and lack of adequate social support. (See 'Contraindications' above.)
For patients with alcoholic liver disease, most programs require a minimum period of abstinence of at least six months, participation in a structured rehabilitation and abstinence program, and adequate social support to help maintain sobriety.
●The goal of the pretransplantation evaluation is to assess the patient's ability to tolerate the stress of surgery, immunosuppression, and the demands of post-transplantation care. Thus, each patient undergoes an extensive cardiopulmonary evaluation, screening for occult infection or cancer, and psychosocial evaluation
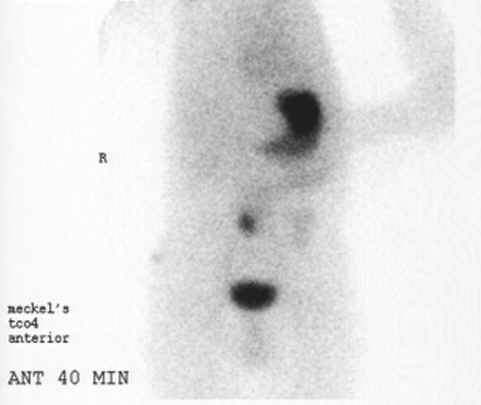
Meckel
References
Video codes
Normal video
{{#ev:youtube|x6e9Pk6inYI}} {{#ev:youtube|4uSSvD1BAHg}} {{#ev:youtube|PQXb5D-5UZw}}
Video in table
Floating video
| Title |
| https://https://www.youtube.com/watch?v=ypYI_lmLD7g%7C350}} |
Redirect
- REDIRECTEsophageal web
synonym website
https://mq.b2i.sg/snow-owl/#!terminology/snomed/10743008
Image
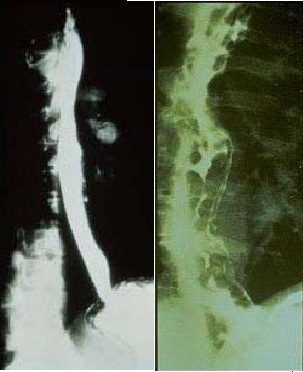
Image to the right
 |
Image and text to the right
<figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>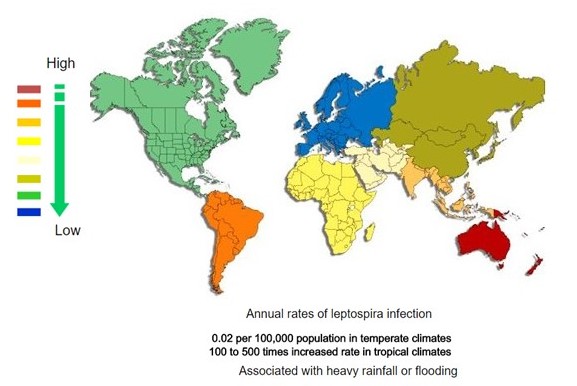 </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
Gallery
-
Histopathology of a pancreatic endocrine tumor (insulinoma). Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]
-
Histopathology of a pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]
-
Histopathology of a pancreatic endocrine tumor (insulinoma). Insulin immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]
References
- ↑ 1.0 1.1 1.2 Neuroendocrine tumor of the pancreas. Libre Pathology. http://librepathology.org/wiki/index.php/Neuroendocrine_tumour_of_the_pancreas
REFERENCES




![Histopathology of a pancreatic endocrine tumor (insulinoma). Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/2/2f/Pancreatic_insulinoma_histology_2.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/a/a3/Pancreatic_insulinoma_histopathology_3.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Insulin immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/d/d5/Pancreatic_insulinoma_histology_4.JPG)