Androgen insensitivity syndrome pathophysiology: Difference between revisions
No edit summary |
|||
| Line 7: | Line 7: | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Pathogenesis=== | |||
*The exact pathogenesis of [disease name] is not fully understood. | |||
OR | |||
*It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3]. | |||
=== | *[Pathogen name] is usually transmitted via the [transmission route] route to the human host. | ||
* | *Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell. | ||
* | *[Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells]. | ||
*The progression to [disease name] usually involves the [molecular pathway]. | |||
*The pathophysiology of [disease/malignancy] depends on the histological subtype. | |||
* | |||
* | |||
* | |||
* | |||
* | |||
===Genetics=== | ===Genetics=== | ||
Revision as of 15:24, 23 August 2017
|
Androgen insensitivity syndrome Microchapters |
|
Differentiating Androgen insensitivity syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Androgen insensitivity syndrome pathophysiology On the Web |
|
American Roentgen Ray Society Images of Androgen insensitivity syndrome pathophysiology |
|
Directions to Hospitals Treating Androgen insensitivity syndrome |
|
Risk calculators and risk factors for Androgen insensitivity syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
Overview
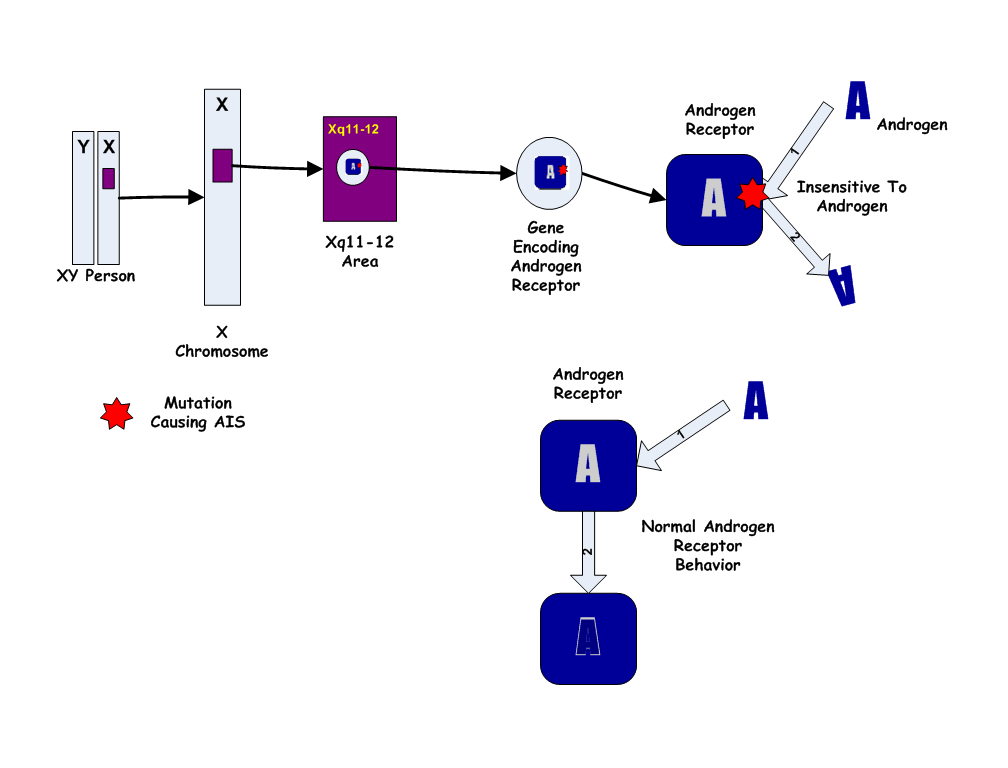
Androgen insensitivity syndrome results from mutations of the gene encoding the androgen receptor. AIS involves variable degree of undervirilization and/or infertility in genetically male person. Family history of other affected individuals related to each other in a pattern consistent with X linked inheritance. Androgen insensitivity syndrome is associated with conditions such as primary amenorrhea, infertility, and dyspareunia.
Pathophysiology
Pathogenesis
- The exact pathogenesis of [disease name] is not fully understood.
OR
- It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
- [Pathogen name] is usually transmitted via the [transmission route] route to the human host.
- Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
- [Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
- The progression to [disease name] usually involves the [molecular pathway].
- The pathophysiology of [disease/malignancy] depends on the histological subtype.
Genetics
- Family history of other affected individuals related to each other in a pattern consistent with X linked inheritance. “Other affected family members” refers to: [1]
- Affected 46,XY individuals
- Manifesting heterozygous females (46,XX).
- About 10% of heterozygous females have asymmetric distribution and sparse or delayed growth of pubic and/or axillary hair.
- Absence of a family history of AIS or suggestive features of AIS does not preclude the diagnosis.
- Because the Androgen Insensitivity Syndrome gives rise to ambiguity between the genetic and the phenotypic gender, we will use the convention 46,XY to designate a genotypic male, and 46,XX to designate a genotypic female. By this convention, a person with Androgen Insensitivity Syndrome is a 46,XY but a phenotypic female.
- The Androgen Insensitivity Syndrome has been linked to mutations in Androgen receptor (AR), the gene for the human Androgen receptor (AR), located at Xq11-12 (i.e. on the X chromosome). Thus, it is an X-linked recessive trait, causing minimal or no effects in 46,XX people.
- However, 46,XX women with a single mutated copy of the AR gene can be "carriers" of AIS, and their 46,XY children (male) will have a 50% chance of having the syndrome. As in some other X-linked recessive conditions, carrier mothers may display some minor traits of the condition: AIS carriers often have reduced axillary and pubic hair, and reduced normal adolescent acne.

Associated Conditions
Gross Pathology
- Complete androgen insensitivity syndrome in a 30 years old woman who presented primary amenorrhea.[2]. [3]
-
Front and side view of the patient
-
Normal female morphotype but absence of pubic and axillary hair
-
Clinical aspect of the vagina
-
Intra- abdominal testes - Laparoscopic aspect
-
The excised testis - Macroscopic aspect
Microscopic Pathology
- Histopathology shows two testes with atrophic seminiferous tubules containing only Sertoli cells, associated to a Leydig cells hyperplasia.[3]
- On histological examination, the well-limited nodule circumscribed by a thin capsule consists of atrophic Servolian tubes with a very small interstitial tissue with rare Leydig cells. This nodule corresponds to a well differentiated tumor with Sertoli-Leydig cells. [2]
-
Testes - Atrophy of the seminiferous tubules - Histopathological aspect, HE staining.[2]
-
testicular parenchyma of lobulated architecture, made of seminiferous tubes of atrophic appearance; these tubes are lined with Sertolia cells, with no obvious signs of spermatogenesis the interstitium is fibrous with rare clusters of Leydig cells.[3]
References
- ↑ Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean L, Bird TD, Ledbetter N, Mefford HC, Smith R, Stephens K, Gottlieb B, Trifiro MA. PMID 20301602. Vancouver style error: initials (help); Missing or empty
|title=(help) - ↑ 2.0 2.1 2.2 Souhail R, Amine S, Nadia A, Tarik K, Khalid EK, Abdellatif K, Ahmed A (2016). "Complete androgen insensitivity syndrome or testicular feminization: review of literature based on a case report". Pan Afr Med J. 25: 199. doi:10.11604/pamj.2016.25.199.10758. PMC 5326263. PMID 28270903.
- ↑ 3.0 3.1 3.2 Lachiri B, Hakimi I, Boudhas A, Guelzim K, Kouach J, Oukabli M, Rahali DM, Dehayni M (2015). "[Complete androgen insensitivity syndrome: report of two cases and review of literature]". Pan Afr Med J (in French). 20: 400. doi:10.11604/pamj.2015.20.400.6760. PMC 4524922. PMID 26301004.





![Testes - Atrophy of the seminiferous tubules - Histopathological aspect, HE staining.[2]](/images/b/b5/AIS_-_Testes_-_atrophy_of_the_seminiferous_tubules_-_Histopathological_aspect%2C_HE_staining.jpg)
![testicular parenchyma of lobulated architecture, made of seminiferous tubes of atrophic appearance; these tubes are lined with Sertolia cells, with no obvious signs of spermatogenesis the interstitium is fibrous with rare clusters of Leydig cells.[3]](/images/8/8a/AIS_-_testicular_parenchyma.jpg)