Acute myeloid leukemia laboratory tests: Difference between revisions
No edit summary |
Carlos Lopez (talk | contribs) No edit summary |
||
| Line 2: | Line 2: | ||
{{Acute myeloid leukemia}} | {{Acute myeloid leukemia}} | ||
{{CMG}}; {{AE}} {{RT}} | {{CMG}}; {{AE}} {{RT}} {{CLG}} | ||
==Overview== | ==Overview== | ||
| Line 25: | Line 25: | ||
* [[Bone marrow examination]] - is often performed to identify the type of abnormal blood cells; however, if there are many leukemic cells circulating in the peripheral blood, a bone marrow [[biopsy]] may not be necessary. | * [[Bone marrow examination]] - is often performed to identify the type of abnormal blood cells; however, if there are many leukemic cells circulating in the peripheral blood, a bone marrow [[biopsy]] may not be necessary. | ||
Marrow or blood is examined via [[light microscopy]] as well as [[flow cytometry]] to diagnose the presence of leukemia, to differentiate | Marrow or blood is examined via [[light microscopy]] as well as [[flow cytometry]] to diagnose the presence of leukemia, to differentiate acute myeloid leukemia from other types of leukemia (e.g. [[acute lymphoblastic leukemia]]), and to classify the subtype of disease. | ||
* A sample of marrow or blood is typically also tested for [[chromosomal translocation]]s by routine [[cytogenetics]] or [[fluorescent in situ hybridization]]. | * A sample of marrow or blood is typically also tested for [[chromosomal translocation]]s by routine [[cytogenetics]] or [[fluorescent in situ hybridization]]. | ||
The diagnosis and classification of | The diagnosis and classification of acute myeloid leukemia can be challenging, and should be performed by a qualified [[hematopathologist]] or [[hematologist]]. In straightforward cases, the presence of certain morphologic features (such as [[Auer rods]]) or specific flow cytometry results can distinguish acute myeloid leukemia from other leukemias; however, in the absence of such features, diagnosis may be more difficult.<ref>Abeloff, Martin et al. (2004), p. 2835.</ref> | ||
{| align="center" | {| align="center" | ||
Revision as of 15:35, 2 September 2015
|
Acute myeloid leukemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Acute myeloid leukemia laboratory tests On the Web |
|
American Roentgen Ray Society Images of Acute myeloid leukemia laboratory tests |
|
Risk calculators and risk factors for Acute myeloid leukemia laboratory tests |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2] Carlos A Lopez, M.D. [3]
Overview
Laboratory Findings
- Complete blood count and differential count - an abnormal result is typically the first clue to a diagnosis of AML. Findings include:
- Leukocytosis
- Leukemic blasts
- Thrombocytopenia
- Anemia - decreased red cell count
- Leucopenia (sometimes)
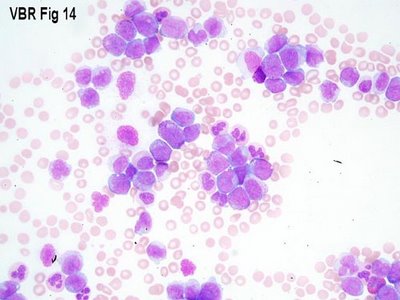
- Peripheral blood smear - immature blast cells can be identified
- Liver function tests
- Renal function tests
- Coagulation studies - prolonged bleeding and clotting time
- Bone marrow examination - is often performed to identify the type of abnormal blood cells; however, if there are many leukemic cells circulating in the peripheral blood, a bone marrow biopsy may not be necessary.
Marrow or blood is examined via light microscopy as well as flow cytometry to diagnose the presence of leukemia, to differentiate acute myeloid leukemia from other types of leukemia (e.g. acute lymphoblastic leukemia), and to classify the subtype of disease.
- A sample of marrow or blood is typically also tested for chromosomal translocations by routine cytogenetics or fluorescent in situ hybridization.
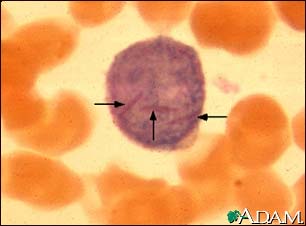
The diagnosis and classification of acute myeloid leukemia can be challenging, and should be performed by a qualified hematopathologist or hematologist. In straightforward cases, the presence of certain morphologic features (such as Auer rods) or specific flow cytometry results can distinguish acute myeloid leukemia from other leukemias; however, in the absence of such features, diagnosis may be more difficult.[1]
 |
 |
References
- ↑ Abeloff, Martin et al. (2004), p. 2835.