Ovarian cancer pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{ | {{varian cancer}} | ||
{{CMG}} | {{CMG}} | ||
| Line 69: | Line 69: | ||
|- | |- | ||
|- | |- | ||
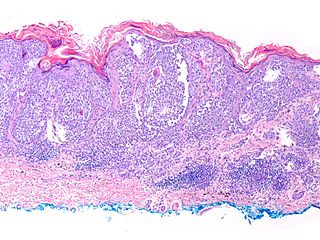
| | | Ovarian serous cystadenocarcinoma|| | ||
* | * Nuclear pleomorphism: | ||
* | :* Variation in size - often marked. | ||
* | :* Variation in staining. | ||
* | :* Variation in shape. | ||
* | * +/-Macronucleolus - key feature. | ||
* Eccentric nucleus. | |||
* Architecture: | |||
:* Solid. | |||
:* Papillary - classic. | |||
* Glandular - uncommon. | |||
* +/-Psammoma bodies - uncommon. | |||
* +/-Necrosis - often extensive. | |||
| [[File: Serous_carcinoma_-_omentum_3_--_very_high_mag.jpg|thumb|none|300px|Micrograph showing serous carcinoma in the omentum, presumed to have arisen from the ovary (ovarian serous carcinoma)]] | | [[File: Serous_carcinoma_-_omentum_3_--_very_high_mag.jpg|thumb|none|300px|Micrograph showing serous carcinoma in the omentum, presumed to have arisen from the ovary (ovarian serous carcinoma)]] | ||
Revision as of 21:01, 9 December 2015
Template:Varian cancer Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Ovarian cancer is often diagnosed late resulting in a poor overall outcome for the patient. Pathological findings, therefore, often only occur in advanced symptomatic onset and tend to present more as severe pathologic outcomes.
Pathophysiology
-
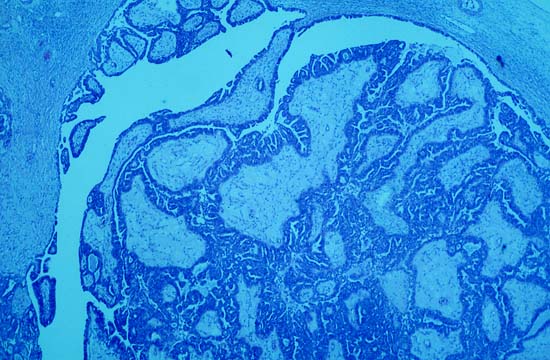
Photomicrograph is from the solid / papillary right ovarian tumor. As shown in this photo, much of the tumor had a papillary pattern with exuberant epithelial proliferation but no obvious stromal invasion. Other areas, such as the one depicted in the second photo, show extensive stromal invasion, the criterion upon which rests the diagnosis of frank malignancy.
-
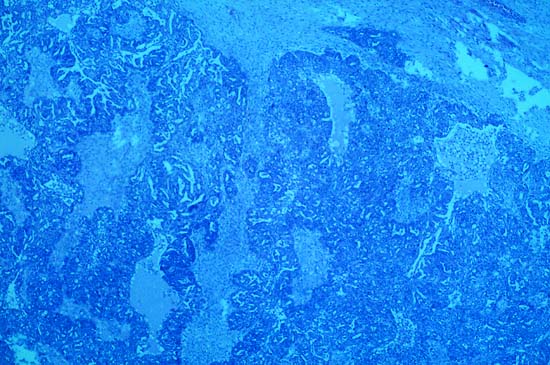
Extensive stromal invasion, the criterion upon which rests the diagnosis of frank malignancy
-
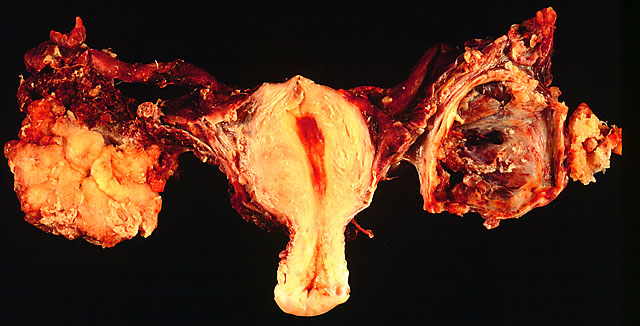
In this TAH-BSO specimen, the right ovary (on the left of the image) has been replaced by a solid serous carcinoma. The contralateral ovarian tumor is grossly cystic and could be termed a "cystadenocarcinoma." The patient had omental metastases and positive peritoneal fluid cytology. This cancer, which was discovered at exploratory laparotomy, apparently developed very rapidly; the patient had a normal pelvic ultrasound exam only 2 months before. (Courtesy of Ed Uthman, MD)
-
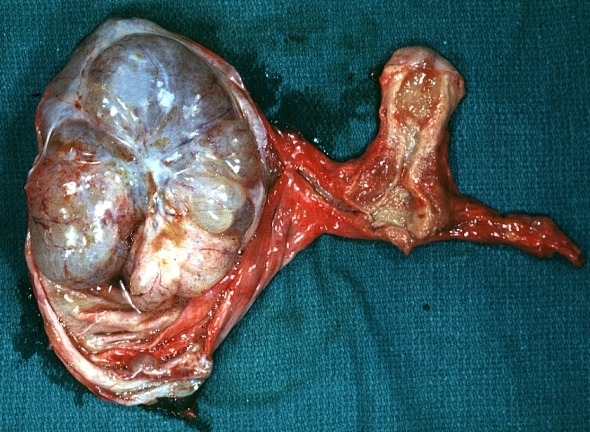
Ovary: Mucinous cystadenocarcinoma: Gross, an excellent image of uterus is in picture and thus illustrates the very large size of the ovarian tumor.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
Gross Patholgy
| Vulvar Carcinomas Subtype | Features on Gross Pathology | ||
| ovarian serous cystadenocarcinoma |
Typically solid with multiple cystic areas. Often >10 cm.
| ||
| Basal cell carcinoma of vulva |
|
Vulvar melanoma |
|
Microscopic Pathology
Histologic subtypes of epithelial ovarian tumor
include:[1][2][3][4]
- Surface epithelial stromal ovarian tumor (60-70%)
- ovarian serous tumor
- ovarian serous cystadenoma: ~60% of serous tumor
- ovarian borderline serous cystadenoma: ~15% of serous tumor
- ovarian serous cystadenocarcinoma: ~25% of serous tumor; commonest malignant ovarian tumour
- ovarian mucinous tumor: ~20% of all ovarian tumor
- ovarian mucinous cystadenoma: ~80% of mucinous tumor
- ovarian bordeline mucinous cystadenoma: 10-15% of mucinous tumor
- ovarian mucinous cystadenocarcinoma: 5-10% of mucinous tumor
- ovarian endometrioid tumour: 8-15% of all ovarian tumor
- clear cell ovarian carcinoma: ~5% of ovarian cancer
- Brenner tumour: ~2.5% of ovarian epithelial neoplasms
- squamous cell carcinoma of the ovary
- ovarian cystadenofibroma / ovarian adenofibroma: can be serous, mucinous, endometrioid, clear cell or mixed
- ovarian cystadenocarcinofibroma: extremely rare
- undifferentiated carcinoma of the ovary: ~4% of all ovarian tumor
References
- ↑ Hoffman, Barbara (2012). Williams gynecology. New York: McGraw-Hill Medical. ISBN 9780071716727.
- ↑ Malignant melanoma. Libre pathology. http://librepathology.org/wiki/index.php/Malignant_melanoma. URL Accessed on September 30, 2015
- ↑ Basal cell carcinoma . Libre pathology. http://librepathology.org/wiki/index.php/Basal_cell_carcinoma. URL Accessed on September 30, 2015
- ↑ Squamous cell carcinoma. Libre pathology. http://librepathology.org/wiki/index.php/Squamous_cell_carcinoma. URL Accessed on September 30, 2015