Papillary thyroid cancer pathophysiology: Difference between revisions
(Created page with "__NOTOC ==Overview== ==Pathogenesis== ==Genetics== ==Associated Conditions== ==Gross Pathology== ==Microscopic Pathology== ==References== {{Reflist|2}} {{WikiDoc Help M...") |
m (Bot: Removing from Primary care) |
||
| (68 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Papillary thyroid cancer}} | |||
{{CMG}}; {{AE}} {{Sahar}} {{Ammu}} | |||
==Overview== | ==Overview== | ||
The exact [[pathogenesis]] of papillary thyroid cancer is not fully understood. Papillary thyroid cancer has been associated with [[somatic]] [[rearrangement]] of [[RET proto-oncogene|RET protooncogene]]. On gross [[pathology]], an ill-defined [[tumor]], irregular [[borders]], and firm consistency are characteristic findings of papillary thyroid cancer. There is no unique consensus on the definition of [[histological]] [[subtypes]] of papillary thyroid cancer. | |||
==Physiology== | |||
* The [[mitogen-activated protein kinase]] ([[MAPK]]) pathway is involved in signal transduction of [[receptor tyrosine kinase]] such as [[RET proto-oncogene|RET]] and [[NTRK1]].<ref name="pmid16434896">{{cite journal |vauthors=Adeniran AJ, Zhu Z, Gandhi M, Steward DL, Fidler JP, Giordano TJ, Biddinger PW, Nikiforov YE |title=Correlation between genetic alterations and microscopic features, clinical manifestations, and prognostic characteristics of thyroid papillary carcinomas |journal=Am. J. Surg. Pathol. |volume=30 |issue=2 |pages=216–22 |date=February 2006 |pmid=16434896 |doi= |url=}}</ref> | |||
*[[Tyrosine kinase]] [[receptor]] activation leads to [[RAS]] activation which subsequently result in [[GTP]] substitution of GDP. The [[GTP-binding protein|GTP]]-bound form of [[RAS]] makes [[BRAF]] active which in turn activates [[MAP kinase kinase kinase|MEK]] and [[ERK]]. | |||
*[[ERK]] is engaged in the regulation of [[gene transcription]] including [[cell differentiation]], [[proliferation]], and survival. | |||
{{familytree/start |summary=Sample 1}} | |||
{{familytree | | | | | | | E04 | | | | | | |E04=Growth factor binds to [[Receptor]] [[tyrosine kinase]] ([[RET]], [[NTRK1]])}} | |||
{{familytree | | | | | | | |!| | | | | | | |}} | |||
{{familytree | | | | | | | E05 | | | | | | |E05=GDP substitution by [[GTP]]}} | |||
{{familytree | | | | | | | |!| | | | | | | |}} | |||
{{familytree | | | | | | | C05 | | | | | | |C05=[[RAS]] activation}} | |||
{{familytree | | | | | | | |!| | | | | | | |}} | |||
{{familytree | | | | | | | C04 | | | | | | |C04=[[BRAF]] activation}} | |||
{{familytree | | | | | | | |!| | | | | | | |}} | |||
{{familytree | | | | | | | D05 | | | | | | |D05=[[MEK]] ativation}} | |||
{{familytree | | | | | | | |!| | | | | | | |}} | |||
{{familytree | | | | | | | G05 | | | | | | |G05=[[ERK]] activation}} | |||
{{familytree | | | | | | | |!| | | | | | | |}} | |||
{{familytree | | |,|-|-|-|-|+|-|-|-|-|.| | |}} | |||
{{familytree | | B01 | | | B02 | | | B03 | |B01=[[cell differentiation]]|B02=cell [[proliferation]]|B03=cell survival}} | |||
{| | |||
! colspan="2" style="background:#DCDCDC;" align="center" + |The above algorithm is adopted from Endocrine patology book<ref name="Lloyd2010">{{cite journal|last1=Lloyd|first1=Ricardo V.|year=2010|doi=10.1007/978-1-4419-1069-1}}</ref> | |||
|- | |||
|} | |||
==Pathogenesis== | ==Pathogenesis== | ||
* The exact [[pathogenesis]] of papillary thyroid cancer (PTC) is not fully understood.<ref>{{cite journal |vauthors=Nikiforov YE |title=RET/PTC rearrangement in thyroid tumors |journal=Endocr. Pathol. |volume=13 |issue=1 |pages=3–16 |date=2002 |pmid=12114746 |doi= |url=}}</ref><ref>{{cite journal |vauthors=Tallini G, Asa SL |title=RET oncogene activation in papillary thyroid carcinoma |journal=Adv Anat Pathol |volume=8 |issue=6 |pages=345–54 |date=November 2001 |pmid=11707626 |doi= |url=}}</ref><ref>{{cite journal |vauthors=Nikiforov YE, Koshoffer A, Nikiforova M, Stringer J, Fagin JA |title=Chromosomal breakpoint positions suggest a direct role for radiation in inducing illegitimate recombination between the ELE1 and RET genes in radiation-induced thyroid carcinomas |journal=Oncogene |volume=18 |issue=46 |pages=6330–4 |date=November 1999 |pmid=10597232 |doi=10.1038/sj.onc.1203019 |url=}}</ref> | |||
* Papillary thyroid cancer has been [[Association (statistics)|associated]] with [[somatic]] rearrangement of [[RET proto-oncogene|RET protooncogene]] se well as point mutation in [[BRAF]] and [[RAS]] [[genes]]. | |||
* All of the aforementioned [[genetic]] alterations leads to [[mitogen-activated protein kinase]] ([[MAPK]]) pathway activation. | |||
* The [[RET gene|RET]] rearrangement encodes for a [[tyrosine kinase]] [[receptor]]. | |||
* This rearrangement has also been observed in mice with a history of [[ionizing radiation]] exposure. | |||
* [[Ionizing radiation]] has been well recognized for its role in papillary thyroid cancer [[etiology]]. | |||
* The rearranged form of this [[gene]] is well-known as [[RET gene|ret]]/PCT [[rearrangement]] and is believed to be related to PTC [[carcinogenesis]]. | |||
* Papillary thyroid cancer [[metastasize]] through [[lymphatics]]. | |||
==Genetics== | ==Genetics== | ||
*[[Genetic]] alteration [[Association (statistics)|associated]] with papillary thyroid cancer include:<ref name="LloydBuehler2011">{{cite journal|last1=Lloyd|first1=Ricardo V.|last2=Buehler|first2=Darya|last3=Khanafshar|first3=Elham|title=Papillary Thyroid Carcinoma Variants|journal=Head and Neck Pathology|volume=5|issue=1|year=2011|pages=51–56|issn=1936-055X|doi=10.1007/s12105-010-0236-9}}</ref> | |||
**[[Mutations]] in [[RET proto-oncogene]] | |||
**[[Mutations]] in the [[BRAF]] oncogene | |||
**[[RAS]] [[mutations]] | |||
**[[TRK]] rearrangements | |||
**[[HMGA2]] [[overexpression]] | |||
==Associated Conditions== | ==Associated Conditions== | ||
* Papillary thyroid cancer may be [[Association (statistics)|associated]] with:<ref name="LloydBuehler2011">{{cite journal|last1=Lloyd|first1=Ricardo V.|last2=Buehler|first2=Darya|last3=Khanafshar|first3=Elham|title=Papillary Thyroid Carcinoma Variants|journal=Head and Neck Pathology|volume=5|issue=1|year=2011|pages=51–56|issn=1936-055X|doi=10.1007/s12105-010-0236-9}}</ref><ref name="HallAbdollahian2013">{{cite journal|last1=Hall|first1=Joseph E.|last2=Abdollahian|first2=Davood J.|last3=Sinard|first3=Robert J.|last4=Eisele|first4=David W.|title=Thyroid disease associated with cowden syndrome: A meta-analysis|journal=Head & Neck|volume=35|issue=8|year=2013|pages=1189–1194|issn=10433074|doi=10.1002/hed.22971}}</ref> | |||
**[[Gardner syndrome]] (especially seen with cribriform-Morular Variant of PTC) | |||
** [[Cowden syndrome]] | |||
==Gross Pathology== | |||
{| align="right" | |||
|[[File:Papillary thyroid carcinoma.jpeg|thumb|right|200px|Papillary thyroid cancer gross pathology<ref name="radio"> Image courtesy of Dr David Cuete. [http://www.radiopaedia.org Radiopaedia] (original file [http://radiopaedia.org/articles/papillary-thyroid-cancer ‘’here’’].[http://radiopaedia.org/licence Creative Commons BY-SA-NC]</ref>]] | |||
|} | |||
* On gross pathology, an ill-defined [[tumor]], irregular borders, and firm consistency are characteristic findings of papillary thyroid cancer.<ref name="Lloyd2010">{{cite journal|last1=Lloyd|first1=Ricardo V.|year=2010|doi=10.1007/978-1-4419-1069-1}}</ref> | |||
*[[Calcification]] may also be present. | |||
* Other less common features include: | |||
**[[Cystic]] [[nodule]] with attached [[papillary]] [[growth]] | |||
** A well-circumscribed, encapsulated [[nodule]] with a [[fleshy]] appearance that may show some [[cystic]] change | |||
==Microscopic Pathology== | |||
* Papillary thyroid carcinoma has numerous [[histological]] subtypes. Each subtype has some specific characteristics.<ref name="Lloyd2010">{{cite journal|last1=Lloyd|first1=Ricardo V.|year=2010|doi=10.1007/978-1-4419-1069-1}}</ref><ref name="LloydBuehler2011">{{cite journal|last1=Lloyd|first1=Ricardo V.|last2=Buehler|first2=Darya|last3=Khanafshar|first3=Elham|title=Papillary Thyroid Carcinoma Variants|journal=Head and Neck Pathology|volume=5|issue=1|year=2011|pages=51–56|issn=1936-055X|doi=10.1007/s12105-010-0236-9}}</ref><ref name="KunjumonUpadhyaya2014">{{cite journal|last1=Kunjumon|first1=DeepaThomas|last2=Upadhyaya|first2=Krishnaraj|title=Histopathological features of Papillary Thyroid Carcinoma with special emphasis on the significance of nuclear features in their diagnosis|journal=Archives of Medicine and Health Sciences|volume=2|issue=1|year=2014|pages=16|issn=2321-4848|doi=10.4103/2321-4848.133786}}</ref> | |||
* There is no unique consensus on the definition of each subtype, so different [[pathologists]] may not agree with these definitions. | |||
* [[Cytologic]] features of papillary thyroid cancer are [[diagnostic]] for this [[tumor]]. These features include: | |||
** Enlarged, irregular, oval shape [[nuclei]] that are overlapped because of the [[nuclear]] enlargement | |||
** [[Nuclear]] clearing | |||
** [[Ground glass]] appearance with prominent [[nuclear]] grooves | |||
** Pink cytoplasmic invaginations | |||
{| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Papillary thyroid cancer subtype'''}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Histopathological Microscopic Analysis'''}} | |||
|- | |||
|- | |||
|'''Follicular''' | |||
| | |||
* Follicles with variable size | |||
* Dark, [[eosinophilic]] [[colloid]] with scalloping ‘‘bubble gum’’ appearance | |||
* [[Cytologic]] features including prominent [[nucleoli]] and increased [[mitotic]] activity are [[diagnostic]] | |||
|- | |||
|'''Conventional''' | |||
| | |||
* [[Papillae]] with [[fibrovascular]] cores | |||
* Enlarged [[nuclei]] with [[nuclear]] clearing | |||
* [[Squamous metaplasia]] may be present | |||
|- | |||
|'''Tall cell''' | |||
| | |||
* With a height 2 to 3 times greater than the width | |||
* [[Cytologic]] features are [[diagnostic]] | |||
|- | |||
|'''Columnar cell''' | |||
| | |||
* Pseudostratified cells | |||
* Overlapping enlarged [[nuclei ]] | |||
|- | |||
|'''Oncocytic''' | |||
| | |||
* Large [[cells]] with abundant [[eosinophilic]] [[cytoplasm]] | |||
* Enlarged [[nuclei]] with [[nuclear]] clearing | |||
|- | |||
|'''Solid''' | |||
| | |||
* Sheets of [[tumor]] [[cells]] with abundant [[cytoplasm]] | |||
* Enlarged [[nuclei]] with [[nuclear]] clearing | |||
|- | |||
|'''Diffuse sclerosing''' | |||
| | |||
* Abundant [[psammoma bodies]], and squamoid changes in the [[tumor]] [[cells]] | |||
* [[Lymphocytic]] infiltrates in the background | |||
|- | |||
|'''Papillary thyroid carcinoma with prominent hobnail features''' | |||
| | |||
* Hobnail [[cells]] with loss of polarity | |||
* High-grade [[cytologic]] features including | |||
* prominent [[nucleoli]] | |||
* increased [[mitotic]] activity | |||
|- | |||
|'''Clear cell''' | |||
| | |||
* Clear [[cells]] with a [[papillary]] architecture | |||
* [[Cytological]] features of papillary thyroid cancer | |||
|- | |||
|'''Cribriform-Morular''' | |||
| | |||
* Cribriform pattern with [[solid]] and [[spindle]] [[cell]] areas | |||
* [[Squamous]] morules | |||
* [[Nuclei]] with clearing and groove | |||
* Involving both thyroid lobes | |||
|- | |||
|'''Macrofollicular''' | |||
| | |||
* Composed of macrofollicles | |||
* [[Cytological]] features of papillary thyroid cancer | |||
|- | |||
|} | |||
== | {| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | ||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Papillary thyroid cancer'''}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Image'''}} | |||
|- | |||
| | |||
* Micrograph of papillary thyroid carcinoma, tall cell variant - high magnification | |||
* "Tall cells": the largest dimension is 3x the smaller dimension | |||
* Abundant [[eosinophilic]] [[cytoplasm]] | |||
* Lack of pseudostratification is a significant differentiator from columnar cell variant of papillary thyroid carcinoma | |||
|[[File:Papillary thyroid carcinoma tall cell var high mag.jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | |||
|- | |||
| | |||
* Micrograph showing oncocytic variant of papillary thyroid carcinoma | |||
* Large cells with abundant eosinophilic cytoplasm | |||
|[[File:Papillary thyroid carcinoma oncocytic variant -- low mag.jpg|thumb|none|250px| H&E stain, Contributed in wikimedia.commons]] | |||
|- | |||
| | |||
* Micrograph showing cribriform-Morular variant of papillary thyroid carcinoma | |||
* Cribriform pattern with [[solid]] and [[spindle]] [[cell]] areas | |||
* [[Squamous]] morules | |||
|[[File:Thyroid PapillaryCarcinoma CribriformMorularVariant HP2 13BR (1).jpg|thumb|none|250px| H&E stain, Contributed in wikimedia.commons]] | |||
|- | |||
| | |||
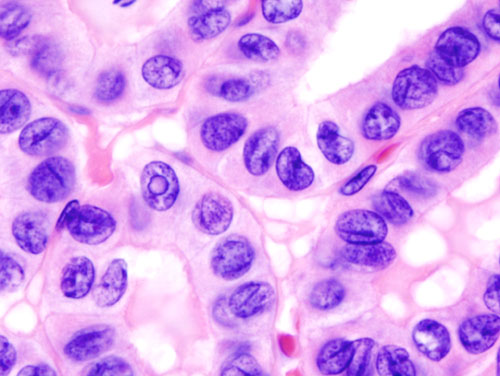
* Micrograph (high power view) showing nuclear changes in papillary thyroid carcinoma (PTC), which include: | |||
** Groove formation | |||
** Optical clearing | |||
** Eosinophilic inclusions and overlapping of nuclei | |||
|[[File:Thyroid papillary carcinoma histopathology (3).jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | |||
|- | |||
| | |||
* Micrograph (high power view) of PTC demonstrating [[nuclear]] clearing and overlapping [[nuclei]] | |||
|[[File:Thyroid papillary carcinoma histopathology (2).jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | |||
|- | |||
| | |||
* Micrograph of papillary thyroid carcinoma demonstrating prominent [[papillae]] with fibrovascular cores | |||
|[[File:Thyroid papillary carcinoma histopatholgy (1).jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | |||
|- | |||
| | |||
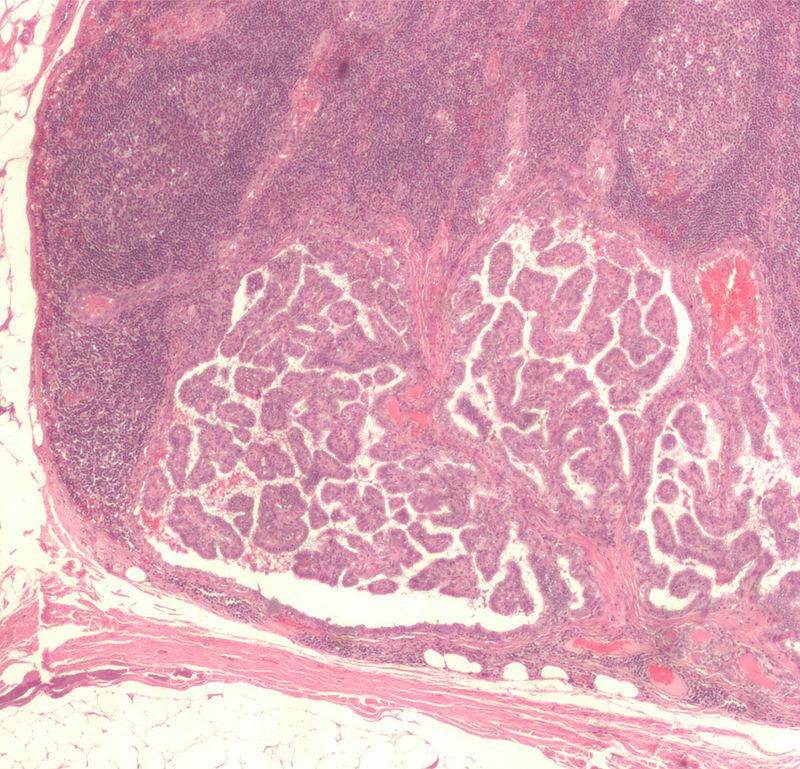
* Micrograph of [[metastatic]] papillary thyroid carcinoma to a [[lymph node]] | |||
* [[Papillary]] architecture -- papillae with fibrovascular cores are present | |||
* [[Lymph node]] with several [[germinal centers]] (left, top/right of image) | |||
* [[Adipose tissue]] (fat) is seen at the edge of the image (bottom and left) | |||
|[[File:-Lymph node with papillary thyroid carcinoma.jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | |||
|- | |||
| | |||
* Micrograph of [[psammoma body]] in papillary thyroid cancer | |||
* A single [[necrotic]] [[tumor cell]] in the center of this structure acts as the nidus for its formation | |||
|[[File:WBR0863.jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | |||
|} | |||
== | ==Immunohistochemistry== | ||
* Papillary thyroid cancer may be positive for following markers:<ref name="Lloyd2010">{{cite journal|last1=Lloyd|first1=Ricardo V.|year=2010|doi=10.1007/978-1-4419-1069-1}}</ref> | |||
**[[TTF-1]] | |||
**[[Thyroglobulin]] | |||
**[[Thyroid peroxidase]] | |||
**[[CD56]] (NCAM) | |||
**[[PAX8]] | |||
** HBME-1 | |||
**[[CITED1]] | |||
**[[Cytokeratin]] 19 | |||
**[[Galectin-3|Galectin 3]] | |||
* These markers are helpful in the confirmation of [[thyroid]] origin of the [[tumor]] particularly when the [[tumor]] is outside of the [[thyroid gland]]. | |||
==Histopathological Video== | |||
===Video=== | |||
{{#ev:youtube|JwymE_Lfs44}} | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Endocrine system]] | |||
[[Category:Endocrinology]] | |||
[[Category:Otolaryngology]] | |||
[[Category:Disease]] | |||
[[Category:Genetic disorders]] | |||
[[Category:Types of cancer]] | |||
[[Category:Hereditary cancers]] | |||
[[Category:Thyroid disease]] | |||
Latest revision as of 23:34, 29 July 2020
|
Papillary thyroid cancer Microchapters |
|
Differentiating Papillary thyroid cancer from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Papillary thyroid cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Papillary thyroid cancer pathophysiology |
|
Risk calculators and risk factors for Papillary thyroid cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sahar Memar Montazerin, M.D.[2] Ammu Susheela, M.D. [3]
Overview
The exact pathogenesis of papillary thyroid cancer is not fully understood. Papillary thyroid cancer has been associated with somatic rearrangement of RET protooncogene. On gross pathology, an ill-defined tumor, irregular borders, and firm consistency are characteristic findings of papillary thyroid cancer. There is no unique consensus on the definition of histological subtypes of papillary thyroid cancer.
Physiology
- The mitogen-activated protein kinase (MAPK) pathway is involved in signal transduction of receptor tyrosine kinase such as RET and NTRK1.[1]
- Tyrosine kinase receptor activation leads to RAS activation which subsequently result in GTP substitution of GDP. The GTP-bound form of RAS makes BRAF active which in turn activates MEK and ERK.
- ERK is engaged in the regulation of gene transcription including cell differentiation, proliferation, and survival.
| Growth factor binds to Receptor tyrosine kinase (RET, NTRK1) | |||||||||||||||||||||||||||||||
| GDP substitution by GTP | |||||||||||||||||||||||||||||||
| RAS activation | |||||||||||||||||||||||||||||||
| BRAF activation | |||||||||||||||||||||||||||||||
| MEK ativation | |||||||||||||||||||||||||||||||
| ERK activation | |||||||||||||||||||||||||||||||
| cell differentiation | cell proliferation | cell survival | |||||||||||||||||||||||||||||
| The above algorithm is adopted from Endocrine patology book[2] |
|---|
Pathogenesis
- The exact pathogenesis of papillary thyroid cancer (PTC) is not fully understood.[3][4][5]
- Papillary thyroid cancer has been associated with somatic rearrangement of RET protooncogene se well as point mutation in BRAF and RAS genes.
- All of the aforementioned genetic alterations leads to mitogen-activated protein kinase (MAPK) pathway activation.
- The RET rearrangement encodes for a tyrosine kinase receptor.
- This rearrangement has also been observed in mice with a history of ionizing radiation exposure.
- Ionizing radiation has been well recognized for its role in papillary thyroid cancer etiology.
- The rearranged form of this gene is well-known as ret/PCT rearrangement and is believed to be related to PTC carcinogenesis.
- Papillary thyroid cancer metastasize through lymphatics.
Genetics
- Genetic alteration associated with papillary thyroid cancer include:[6]
- Mutations in RET proto-oncogene
- Mutations in the BRAF oncogene
- RAS mutations
- TRK rearrangements
- HMGA2 overexpression
Associated Conditions
- Papillary thyroid cancer may be associated with:[6][7]
- Gardner syndrome (especially seen with cribriform-Morular Variant of PTC)
- Cowden syndrome
Gross Pathology
 |
- On gross pathology, an ill-defined tumor, irregular borders, and firm consistency are characteristic findings of papillary thyroid cancer.[2]
- Calcification may also be present.
- Other less common features include:
Microscopic Pathology
- Papillary thyroid carcinoma has numerous histological subtypes. Each subtype has some specific characteristics.[2][6][9]
- There is no unique consensus on the definition of each subtype, so different pathologists may not agree with these definitions.
- Cytologic features of papillary thyroid cancer are diagnostic for this tumor. These features include:
- Enlarged, irregular, oval shape nuclei that are overlapped because of the nuclear enlargement
- Nuclear clearing
- Ground glass appearance with prominent nuclear grooves
- Pink cytoplasmic invaginations
| Papillary thyroid cancer subtype | Features on Histopathological Microscopic Analysis |
| Follicular |
|
| Conventional |
|
| Tall cell |
|
| Columnar cell |
|
| Oncocytic |
|
| Solid | |
| Diffuse sclerosing |
|
| Papillary thyroid carcinoma with prominent hobnail features | |
| Clear cell |
|
| Cribriform-Morular | |
| Macrofollicular |
|
| Papillary thyroid cancer | Image |
|
 |
|
 |
 | |
|
 |
 | |
|
 |
|
 |
|
 |
Immunohistochemistry
- Papillary thyroid cancer may be positive for following markers:[2]
- TTF-1
- Thyroglobulin
- Thyroid peroxidase
- CD56 (NCAM)
- PAX8
- HBME-1
- CITED1
- Cytokeratin 19
- Galectin 3
- These markers are helpful in the confirmation of thyroid origin of the tumor particularly when the tumor is outside of the thyroid gland.
Histopathological Video
Video
{{#ev:youtube|JwymE_Lfs44}}
References
- ↑ Adeniran AJ, Zhu Z, Gandhi M, Steward DL, Fidler JP, Giordano TJ, Biddinger PW, Nikiforov YE (February 2006). "Correlation between genetic alterations and microscopic features, clinical manifestations, and prognostic characteristics of thyroid papillary carcinomas". Am. J. Surg. Pathol. 30 (2): 216–22. PMID 16434896.
- ↑ 2.0 2.1 2.2 2.3 Lloyd, Ricardo V. (2010). doi:10.1007/978-1-4419-1069-1. Missing or empty
|title=(help) - ↑ Nikiforov YE (2002). "RET/PTC rearrangement in thyroid tumors". Endocr. Pathol. 13 (1): 3–16. PMID 12114746.
- ↑ Tallini G, Asa SL (November 2001). "RET oncogene activation in papillary thyroid carcinoma". Adv Anat Pathol. 8 (6): 345–54. PMID 11707626.
- ↑ Nikiforov YE, Koshoffer A, Nikiforova M, Stringer J, Fagin JA (November 1999). "Chromosomal breakpoint positions suggest a direct role for radiation in inducing illegitimate recombination between the ELE1 and RET genes in radiation-induced thyroid carcinomas". Oncogene. 18 (46): 6330–4. doi:10.1038/sj.onc.1203019. PMID 10597232.
- ↑ 6.0 6.1 6.2 Lloyd, Ricardo V.; Buehler, Darya; Khanafshar, Elham (2011). "Papillary Thyroid Carcinoma Variants". Head and Neck Pathology. 5 (1): 51–56. doi:10.1007/s12105-010-0236-9. ISSN 1936-055X.
- ↑ Hall, Joseph E.; Abdollahian, Davood J.; Sinard, Robert J.; Eisele, David W. (2013). "Thyroid disease associated with cowden syndrome: A meta-analysis". Head & Neck. 35 (8): 1189–1194. doi:10.1002/hed.22971. ISSN 1043-3074.
- ↑ Image courtesy of Dr David Cuete. Radiopaedia (original file ‘’here’’.Creative Commons BY-SA-NC
- ↑ Kunjumon, DeepaThomas; Upadhyaya, Krishnaraj (2014). "Histopathological features of Papillary Thyroid Carcinoma with special emphasis on the significance of nuclear features in their diagnosis". Archives of Medicine and Health Sciences. 2 (1): 16. doi:10.4103/2321-4848.133786. ISSN 2321-4848.