|
|
| (3 intermediate revisions by the same user not shown) |
| Line 1: |
Line 1: |
| __NOTOC__
| | {{Drugbox |
| {{CMG}} | | | verifiedrevid = 459444186 |
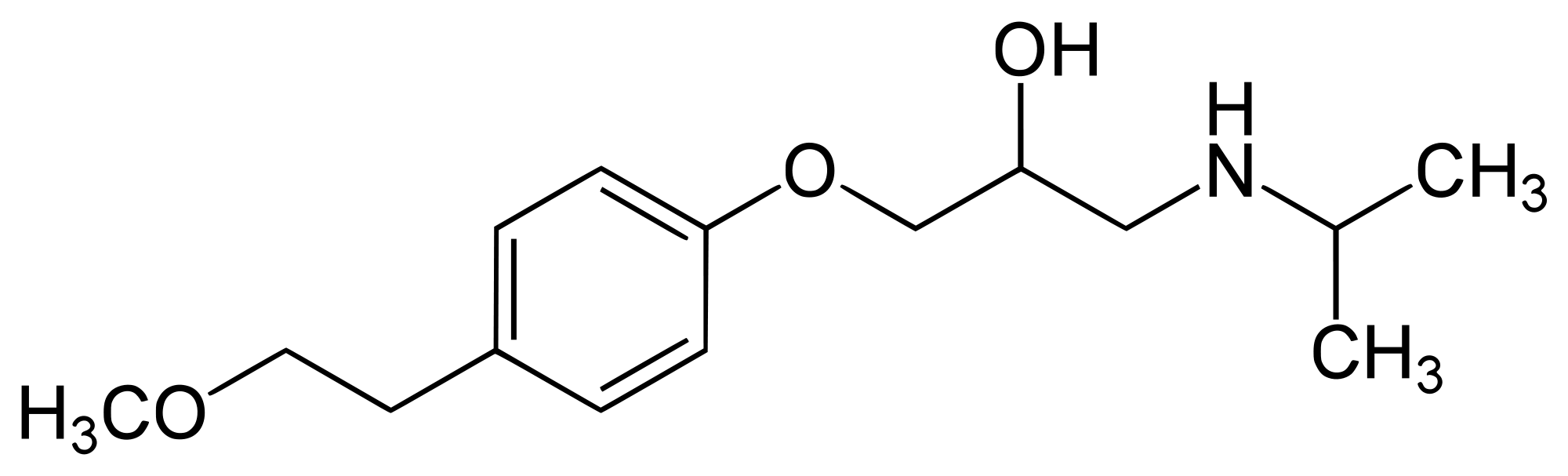
| | | IUPAC_name = (''RS'')-1-(Isopropylamino)-3-[4-(2-methoxyethyl)phenoxy]propan-2-ol |
| | | image = 2000px-Metoprolol structure.svg.png |
| | | drug_name = Metoprolol |
|
| |
|
| ==Definition==
| | <!--Clinical data--> |
| * Exacerbation of COPD is an acute event characterized by a worsening of the patient’s respiratory symptoms that is beyond normal day-to-day variations and leads to a change in medication.<ref name="Burge-2003">{{Cite journal | last1 = Burge | first1 = S. | last2 = Wedzicha | first2 = JA. | title = COPD exacerbations: definitions and classifications.|journal = Eur Respir J Suppl | volume = 41 | issue = | pages = 46s-53s | month = Jun | year = 2003 | doi = | PMID = 12795331 }}</ref><ref name="Celli-2007">{{Cite journal |last1 = Celli | first1 = BR. | last2 = Barnes | first2 = PJ. | title = Exacerbations of chronic obstructive pulmonary disease. | journal = Eur Respir J | volume = 29 | issue = 6 |pages = 1224-38 | month = Jun | year = 2007 | doi = 10.1183/09031936.00109906 | PMID = 17540785 }}</ref><ref name="Rodriguez-Roisin-2000">{{Cite journal | last1 = Rodriguez-Roisin| first1 = R. | title = Toward a consensus definition for COPD exacerbations. | journal = Chest | volume = 117 | issue = 5 Suppl 2 | pages = 398S-401S | month = May | year = 2000 |doi = |PMID = 10843984 }}</ref>
| | | tradename = Lopressor, Toprol-xl |
| | | Drugs.com = {{drugs.com|monograph|metoprolol-succinate}} |
| | | MedlinePlus = a682864 |
| | | licence_US = Metoprolol |
| | | pregnancy_AU = C |
| | | pregnancy_US = C |
| | | legal_status = Rx-only |
| | | routes_of_administration = Oral, [[Intravenous|IV]] |
|
| |
|
| * The diagnosis of an exacerbation relies exclusively on the clinical presentation of the patient complaining of an acute change of symptoms ('''baseline dyspnea, cough, and/or sputum production''') that is beyond normal day-to-day variation.<ref name="Vestbo-2013">{{Cite journal | last1 = Vestbo | first1 = J. | last2 = Hurd | first2 = SS. | last3 = Agustí | first3 = AG. | last4 = Jones | first4 = PW. | last5 = Vogelmeier | first5 = C. | last6 = Anzueto | first6 = A. | last7 = Barnes | first7 = PJ. | last8 = Fabbri | first8 = LM. | last9 = Martinez | first9 = FJ. | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary.|journal = Am J Respir Crit Care Med | volume = 187 | issue = 4 | pages = 347-65 | month = Feb | year = 2013 | doi = 10.1164/rccm.201204-0596PP | PMID = 22878278 }}</ref>
| | <!--Pharmacokinetic data--> |
| | | bioavailability = 12% |
| | | metabolism = [[Liver|Hepatic]] via [[CYP2D6]], [[CYP3A4]] |
| | | elimination_half-life = 3-7 hours |
| | | excretion = [[Kidney|Renal]] |
|
| |
|
| ==Causes== | | <!--Identifiers--> |
| ===Life-Threatening Causes=== | | | CAS_number_Ref = {{cascite|correct|??}} |
| <SMALL>''Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.''</SMALL>
| | | CAS_number = 51384-51-1 |
| * [[Arrhythmia]]
| | | ATC_prefix = C07 |
| * [[Congestive heart failure]]
| | | ATC_suffix = AB02 |
| * [[Pleural effusion]]
| | | PubChem = 4171 |
| * [[Pneumonia]]
| | | IUPHAR_ligand = 553 |
| * [[Pneumothorax]]
| | | DrugBank_Ref = {{drugbankcite|correct|drugbank}} |
| * [[Pulmonary embolism]]
| | | DrugBank = DB00264 |
| | | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} |
| | | ChemSpiderID = 4027 |
| | | UNII_Ref = {{fdacite|correct|FDA}} |
| | | UNII = GEB06NHM23 |
| | | KEGG_Ref = {{keggcite|correct|kegg}} |
| | | KEGG = D02358 |
| | | ChEBI_Ref = {{ebicite|correct|EBI}} |
| | | ChEBI = 6904 |
| | | ChEMBL_Ref = {{ebicite|correct|EBI}} |
| | | ChEMBL = 13 |
|
| |
|
| ===Common Causes===
| | <!--Chemical data--> |
| * [[Respiratory tract infections]] (~½)
| | | C=15 | H=25 | N=1 | O=3 |
| * Unknown (~⅓)
| | | molecular_weight = 267.364 [[gram|g]]/[[Mole (unit)|mol]] |
| * Air pollutants
| | | smiles = O(c1ccc(cc1)CCOC)CC(O)CNC(C)C |
| | | | InChI = 1/C15H25NO3/c1-12(2)16-10-14(17)11-19-15-6-4-13(5-7-15)8-9-18-3/h4-7,12,14,16-17H,8-11H2,1-3H3 |
| ==Treatment Setting==
| | | InChIKey = IUBSYMUCCVWXPE-UHFFFAOYAN |
| {{Family tree/start}}
| | | StdInChI_Ref = {{stdinchicite|correct|chemspider}} |
| {{Family tree |border=2|boxstyle=background: WhiteSmoke;|A1|A1=<div style="float: left; text-align: left; height: 5.5em; width: 9.7em; padding: 1em;">'''''COPD Exacerbation'''''<BR>❑ Cough ↑ <BR> ❑ Dyspnea ↑ <BR> ❑ Sputum ↑ </div>}}
| | | StdInChI = 1S/C15H25NO3/c1-12(2)16-10-14(17)11-19-15-6-4-13(5-7-15)8-9-18-3/h4-7,12,14,16-17H,8-11H2,1-3H3 |
| {{Family tree |!|}}
| | | StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} |
| {{Family tree |border=2|boxstyle=background:WhiteSmoke;|)|B1|B1=<div style="float: left; text-align: left; height: 4.8em; width: 41em; padding: 1em">
| | | StdInChIKey = IUBSYMUCCVWXPE-UHFFFAOYSA-N |
| '''1. Oxygen Supplement''' <BR> ❑ Pulse oximetry (maintain Sa<sub>O<sub>2</sub></sub> ≥88—92%)<ref name="Austin-2010">{{Cite journal | last1 = Austin | first1 = MA. | last2 = Wills | first2 = KE. | last3 = Blizzard | first3 = L. | last4 = Walters | first4 = EH. | last5 = Wood-Baker | first5 = R. | title = Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. | journal = BMJ | volume = 341 | issue = | pages = c5462 | month = | year = 2010 | doi = | PMID = 20959284 }}</ref> <BR> ❑ Arterial blood gas (if acute or acute-on-chronic respiratory failure is suspected)</div>}}
| | | melting_point = 120 |
| {{Family tree |!|}}
| | }} |
| {{Family tree |border=2|boxstyle=background:WhiteSmoke;|)|C1|C1=<div style="float: left; text-align: left; height: 7em; width: 39em; padding: 1em">
| |
| '''2. Indications for ICU Admission'''<BR> ❑ Hemodynamic instability <BR> ❑ Changes in mental status (confusion, lethargy, coma) <BR> ❑ Severe dyspnea that responds inadequately to initial emergency therapy <BR> ❑ Worsening hypoxemia (Pa<sub>O<sub>2</sub></sub> <40 mm Hg) and/or respiratory acidosis (pH <7.25)</div>}}
| |
| {{Family tree |!| | |!|}}
| |
| {{Family tree |border=2|boxstyle=background:WhiteSmoke;|!| |D1|D1=<div style="float: left; text-align: left; height: 23em; width: 40em; padding: 1em">'''2a. Indications for Noninvasive Mechanical Ventilation''' <BR> ❑ Respiratory acidosis (arterial pH < 7.35 or Pa<sub>CO<sub>2</sub></sub> >45 mm Hg) <BR> ❑ Severe dyspnea with sings of respiratory muscle fatigue <BR> ❑ Increased work of breathing
| |
| ----
| |
| '''2b. Indications for Invasive Mechanical Ventilation''' <BR> ❑ Diminished consciousness, psychomotor agitation inadequately controlled by sedation <BR> ❑ Severe hemodynamic instability without response to fluids and vasoactive drugs <BR> ❑ Respiratory pauses with loss of consciousness or gasping for air <BR> ❑ Life-threatening hypoxemia in patients unable to tolerate NIV <BR> ❑ Persistent inability to remove respiratory secretions <BR> ❑ Heart rate <50/min with loss of alertness <BR> ❑ Severe ventricular arrhythmias <BR> ❑ Respiratory or cardiac arrest <BR> ❑ Failure of initial trial of NIV <BR> ❑ Massive aspiration</div>}}
| |
| {{Family tree |!|}}
| |
| {{Family tree |border=2|boxstyle=background:WhiteSmoke;|`|E1|E1=<div style="float: left; text-align: left; height: 23em; width: 41em; padding: 1em">
| |
| '''3. Indications for Hospitalization''' <BR> ❑ Marked increase in intensity of symptoms (eg, sudden development of resting dyspnea) <BR> ❑ Presence of serious comorbidities (eg, heart failure or newly occurring arrhythmias) <BR> ❑ Failure of an exacerbation to respond to initial medical management <BR> ❑ Onset of new physical signs (eg, cyanosis, peripheral edema) <BR> ❑ Severe underlying COPD (GOLD 3—4 categories) <BR> ❑ Frequent exacerbations (≥2 events per year) <BR> ❑ Insufficient home support <BR> ❑ Older age (>65 years)
| |
| ----
| |
| '''4. Assessment of Exacerbation''' <BR> ❑ Cardinal symptoms (↑ dyspnea, ↑ sputum volume, and ↑ sputum purulence) <BR> ❑ ECG (identify coexisting cardiac problems) <BR> ❑ Chest radiograph (exclude alternative diagnoses)<BR> ❑ Whole-blood count (identify polycythemia, anemia, or leukocytosis) <BR> ❑ Electrolytes and glucose (identify electrolyte disturbances or hyperglycemia)</div>}}
| |
| {{Family tree | | | |!|}}
| |
| {{Family tree |border=2|boxstyle=background:WhiteSmoke;| | | |F1|F1=<div style="float: left; text-align: left; height: 30em; width: 30em; padding: 1em">
| |
| '''''Severe Exacerbation''''' (⊕ 3 cardinal symptoms) <BR> ❑ Consider inpatient management <BR> ❑ Assess symptoms, ABG, and CXR <BR> ❑ Monitor fluid balance and nutrition <BR> ❑ Identify and treat associated conditions <BR> ❑ Consider subcutaneous heparin or LMWH <BR> ❑ Controlled oxygen therapy (consider NIV if indicated) <BR> ❑ Antibiotics (if ↑ sputum purulence or ⊕ bacterial infection) <BR> ❑ Corticosteroids <BR> ❑ Bronchodilators <BR> ▸ Increase doses/frequency of short-acting bronchodilators <BR> ▸ Combine short-acting β2-agonists and anticholinergics <BR> ▸ Use spacers or air-driven nebulizers
| |
| ----
| |
| '''''Moderate Exacerbation''''' (⊕ 2 cardinal symptoms) <BR> ❑ Consider outpatient management <BR> ❑ Require a short course of antibiotics and/or oral corticosteroids
| |
| ----
| |
| '''''Mild Exacerbation''''' (⊕ 1 cardinal symptom) <BR> ❑ Consider outpatient management <BR> ❑ Require change of inhaled treatment by the patient</div>}}
| |
| {{Family tree/end}}
| |
| | |
| ==Pharmacologic Treatment==
| |
| {{Family tree/start}}
| |
| {{Family tree |border=2|boxstyle=background: WhiteSmoke;|A1|A1=<div style="float: left; text-align: left; height: 43em; width: 45em; padding: 1em;">'''Indications for Antibiotics'''<BR> ❑ Mechanical ventilation required <BR> ❑ Severe exacerbation (⊕ 3 cardinal symptoms) <BR> ❑ Moderate exacerbation with ↑ sputum purulence
| |
| ----
| |
| '''''Complicated COPD''''' (⊕ Risk Factors) <BR> ❑ Age ≥65 years <BR> ❑ FEV<sub>1</sub> ≤50% predicted <BR> ❑ ≥3 exacerbations per year <BR> ❑ Cardiac disease <BR> ▸'''''[[Moxifloxacin]] 400 mg PO q24h''''' <BR> ▸ '''''[[Gemifloxacin]] 320 mg PO q24h''''' <BR> ▸ '''''[[Levofloxacin]] 500 mg PO q24h''''' <BR> ▸'''''[[Amoxicillin/Clavulanate|Amoxicillin-Clavulanate]] 875/125 mg PO bid or 2000/125 mg PO bid or 500/125 mg PO q8h''''' <BR> ▸ '''''[[Ciprofloxacin]] 750 mg PO q12h with sputum culture''''' (if at risk for ''Pseudomonas'')
| |
| ----
| |
| '''''Uncomplicated COPD''''' (⌀ Risk Factors) <BR> ▸ '''''[[Azithromycin]] 500 mg PO q24h or 500 mg PO x1 dose followed by 250 mg PO q24h''''' <BR> ▸ '''''[[Clarithromycin]]extended-release 1000 mg PO q24h'''''<BR> ▸ '''''[[Cefuroxime axetil]] 250 or 500 mg PO q12h''''' <BR> ▸ '''''[[Cefpodoxime]] 200 mg PO q12h''''' <BR> ▸ '''''[[Cefdinir]] 300 mg PO q12h or 600 mg PO q24h''''' <BR> ▸ '''''[[Doxycycline]] 100 mg PO bid''''' <BR> ▸ '''''[[Trimethoprim-Sulfamethoxazole]] 160/800 mg PO bid'''''
| |
| ----
| |
| '''Treatment Notes'''<ref name="Sethi-2008">{{Cite journal | last1 = Sethi | first1 = S. | last2 = Murphy | first2 = TF. | title = Infection in the pathogenesis and course of chronic obstructive pulmonary disease. | journal = N Engl J Med | volume = 359 | issue = 22 | pages = 2355-65 | month = Nov | year = 2008 | doi = 10.1056/NEJMra0800353 | PMID = 19038881 }}</ref><ref name="isbn1-9308-0874-7">{{cite book | author = | authorlink = | editor = |others = | title = The Sanford Guide to Antimicrobial Therapy | edition = | language = |publisher = | location = | year = |origyear = | pages = |quote = | isbn = 1-9308-0874-7 | oclc = |doi = |url = | accessdate = }}</ref> <BR> ❑ Antibiotic choice should reflect local resistance pattern <BR> ❑ Use alternative class if antibiotic exposure within 3 months <BR> ❑ Re-evaluate and consider sputum culture if failed to respond in 72 hours <BR> ❑ The recommended length of antibiotic therapy is usually 5—10 days </div>}}
| |
| {{Family tree/end}}
| |
| | |
| | |
| {{Family tree/start}}
| |
| {{Family tree |border=2|boxstyle=background: WhiteSmoke;|A1|A1=<div style="float: left; text-align: left; height: 9em; width: 45em; padding:1em;">'''Corticosteroids''' <BR> ▸'''''[[Prednisolone]] 30—40 mg PO q24h for 10—14 days''''' (for mild/moderate exacerbation) <BR> ▸ '''''[[Methylprednisolone]] 125 mg IV q6h for 3 days''''' (for severe exacerbation)
| |
| ----
| |
| '''Treatment Notes'''<ref name="Vestbo-2013">{{Cite journal | last1 = Vestbo | first1 = J. | last2 = Hurd | first2 = SS. | last3 = Agustí | first3 = AG. | last4 = Jones | first4 = PW. | last5 = Vogelmeier | first5 = C. | last6 = Anzueto | first6 = A. | last7 = Barnes | first7 = PJ. | last8 = Fabbri | first8 = LM. | last9 = Martinez | first9 = FJ. | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. | journal = Am J Respir Crit Care Med | volume = 187| issue = 4 | pages = 347-65 | month = Feb | year = 2013 | doi = 10.1164/rccm.201204-0596PP | PMID = 22878278 }}</ref><ref name="Maltais-2002">{{Cite journal | last1 = Maltais |first1 = F. | last2 = Ostinelli | first2 = J. | last3 = Bourbeau | first3 = J. | last4 = Tonnel | first4 = AB. | last5 = Jacquemet | first5 = N. | last6 = Haddon | first6 = J. |last7 = Rouleau | first7 = M. | last8 = Boukhana | first8 = M. | last9 = Martinot | first9 = JB. | title = Comparison of nebulized budesonide and oral prednisolone with placebo in the treatment of acute exacerbations of chronic obstructive pulmonary disease: a randomized controlled trial. | journal = Am J Respir Crit Care Med | volume = 165 | issue = 5 |pages = 698-703 | month = Mar | year = 2002 | doi = 10.1164/ajrccm.165.5.2109093 | PMID = 11874817 }}</ref><ref name="Gunen-2007">{{Cite journal | last1 = Gunen | first1 = H. |last2 = Hacievliyagil | first2 = SS. | last3 = Yetkin | first3 = O. | last4 = Gulbas | first4 = G. | last5 = Mutlu | first5 = LC. | last6 = In | first6 = E. | title = The role of nebulised budesonide in the treatment of exacerbations of COPD. | journal = Eur Respir J | volume = 29 | issue = 4 | pages = 660-7 | month = Apr | year = 2007 | doi = 10.1183/09031936.00073506 | PMID = 17251232 }}</ref><ref name="Ställberg-2009">{{Cite journal | last1 = Ställberg | first1 = B. | last2 = Selroos | first2 = O. | last3 = Vogelmeier| first3 = C. | last4 = Andersson | first4 = E. | last5 = Ekström | first5 = T. | last6 = Larsson | first6 = K. | title = Budesonide/formoterol as effective as prednisolone plus formoterol in acute exacerbations of COPD. A double-blind, randomised, non-inferiority, parallel-group, multicentre study. |journal = Respir Res | volume = 10 | issue = | pages = 11 | month = | year = 2009 | doi = 10.1186/1465-9921-10-11 | PMID = 19228428 }}</ref> <BR> ❑ '''''[[Budesonide]] 400 mcg IH bid''''' may be an alternative to oral corticosteroids<BR> ❑ Corticosteroids should be tapered over 2 weeks</div>}}
| |
| {{Family tree/end}}
| |
| | |
| | |
| {{Family tree/start}}
| |
| {{Family tree |border=2|boxstyle=background: WhiteSmoke;|A1|A1=<div style="float: left; text-align: left; height: 17em; width: 45em; padding:1em;">'''Anticholinergics''' <BR> ▸'''''[[Ipratropium]] MDI 4—8 puffs IH q1—2h OR Nebulizer 0.5 mg IH q1—2h'''''
| |
| ----
| |
| '''β2-adrenergic agonists''' <BR> ▸ '''''[[Albuterol]] MDI 4—8 puffs IH q1—2h OR Nebulizer 2.5—5 mg IH q1—2h'''''
| |
| ----
| |
| '''Methylxanthines''' <BR> ▸ '''''[[Aminophylline]] 0.9 mg/kg/hr IV''''' <BR> ▸ '''''[[Theophylline]] 150—450 mg PO bid'''''
| |
| ----
| |
| '''Treatment Notes'''<ref name="Stoller-2002">{{Cite journal | last1 = Stoller | first1 = JK. | title = Clinical practice. Acute exacerbations of chronic obstructive pulmonary disease. | journal = N Engl J Med | volume = 346 | issue = 13 | pages = 988-94 | month = Mar | year = 2002 | doi = 10.1056/NEJMcp012477 | PMID = 11919309 }}</ref><ref name="Celli-2004">{{Cite journal | last1 = Celli | first1 = BR. | last2 = MacNee | first2 = W. | title = Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. | journal = Eur Respir J | volume = 23 | issue = 6 | pages = 932-46 | month = Jun | year = 2004 | doi = | PMID = 15219010 }}</ref><ref name="Barberá-1992">{{Cite journal | last1 = Barberá | first1 = JA. | last2 = Reyes | first2 = A. | last3 = Roca | first3 = J. | last4 = Montserrat | first4 = JM. | last5 = Wagner | first5 = PD. |last6 = Rodríguez-Roisin | first6 = R. | title = Effect of intravenously administered aminophylline on ventilation/perfusion inequality during recovery from exacerbations of chronic obstructive pulmonary disease. | journal = Am Rev Respir Dis | volume = 145 | issue = 6 | pages = 1328-33 | month = Jun | year = 1992 |doi = 10.1164/ajrccm/145.6.1328 | PMID = 1595998 }}</ref><ref name="Emerman-1990">{{Cite journal | last1 = Emerman | first1 = CL. | last2 = Connors | first2 = AF. | last3 = Lukens| first3 = TW. | last4 = May | first4 = ME. | last5 = Effron | first5 = D. | title = Theophylline concentrations in patients with acute exacerbation of COPD. | journal = Am J Emerg Med |volume = 8 | issue = 4 | pages = 289-92 | month = Jul | year = 1990 | doi = | PMID = 2363749 }}</ref><ref name="Lloberes-1988">{{Cite journal | last1 = Lloberes | first1 = P. |last2 = Ramis | first2 = L. | last3 = Montserrat | first3 = JM. | last4 = Serra | first4 = J. | last5 = Campistol | first5 = J. | last6 = Picado | first6 = C. | last7 = Agusti-Vidal |first7 = A. | title = Effect of three different bronchodilators during an exacerbation of chronic obstructive pulmonary disease. | journal = Eur Respir J | volume = 1 |issue = 6 |pages = 536-9 | month = Jun | year = 1988 | doi = | PMID = 2971565 }}</ref><ref name="Mahon-1999">{{Cite journal | last1 = Mahon | first1 = JL. | last2 = Laupacis |first2 = A. |last3 = Hodder | first3 = RV. | last4 = McKim | first4 = DA. | last5 = Paterson | first5 = NA. | last6 = Wood | first6 = TE. | last7 = Donner | first7 = A. | title = Theophylline for irreversible chronic airflow limitation: a randomized study comparing n of 1 trials to standard practice. | journal = Chest | volume = 115 | issue = 1 | pages = 38-48 | month = Jan |year = 1999 | doi = | PMID = 9925061 }}</ref><ref name="Murciano-1984">{{Cite journal | last1 = Murciano | first1 = D. | last2 = Aubier | first2 = M. | last3 = Lecocguic | first3 = Y. | last4 = Pariente |first4 = R. | title = Effects of theophylline on diaphragmatic strength and fatigue in patients with chronic obstructive pulmonary disease. | journal = N Engl J Med | volume = 311 |issue = 6 | pages = 349-53 | month = Aug | year = 1984 | doi = 10.1056/NEJM198408093110601 | PMID = 6738652 }}</ref><ref>{{Cite web | last = | first = |title =http://www.nice.org.uk/nicemedia/live/13029/49397/49397.pdf | url = http://www.nice.org.uk/nicemedia/live/13029/49397/49397.pdf | publisher = | date = | accessdate = 18 December 2013 }}</ref> <BR> ❑ Short-acting β2-agonists with or without short-acting anticholinergics are generally preferred <BR> ❑ Consider methylxanthine as an adjunct if inadequate response to bronchodilators</div>}}
| |
| {{Family tree/end}}
| |
| | |
| ==Checklist at Time of Discharge From Hospital==
| |
| {{Family tree/start}}
| |
| {{Family tree |border=2|boxstyle=background: WhiteSmoke;|A1|A1=<div style="float: left; text-align: left; height: 13em; width: 41em; padding: 1em;">'''Action Items at Discharge'''<BR> ❑ Reinforce smoking cessation measures <BR> ❑ Assure effective home maintenance of pharmacotherapy regimen <BR> ❑ Reassess inhaler technique <BR> ❑ Educate about maintenance regimen <BR> ❑ Give instruction regarding completion of steroid therapy and antibiotics <BR> ❑ Assess need for long-term oxygen therapy <BR> ❑ Assure follow-up visit in 4—6 weeks<BR> ❑ Provide a management plan for comorbidities and their follow-up</div>}}
| |
| {{Family tree/end}}
| |
| | |
| ==Checklist at Follow-Up Visit 4—6 Weeks After Discharge==
| |
| {{Family tree/start}}
| |
| {{Family tree |border=2|boxstyle=background: WhiteSmoke;|A1|A1=<div style="float: left; text-align: left; height: 18em; width: 41em; padding: 1em;">'''Action Items at Follow-Up Visit''' <BR> ❑ Smoking cessation measures <BR> ❑ Ability to cope in usual environment <BR> ❑ Reassess inhaler technique <BR> ❑ Measurement of FEV<sub>1</sub> <BR> ❑ Inhaler technique <BR> ❑ Understanding of recommended treatment regimen <BR> ❑ Need for long-term oxygen therapy and/or home nebulizer <BR> ❑ Capacity to do physical activity and activities of daily living <BR> ❑ Chronic Obstructive Pulmonary Disease Assessment Test (CAT) <BR> ❑ Modified British Medical Research Council questionnaire on breathlessness (mMRC) <BR> ❑ Status of comorbidities</div>}}
| |
| {{Family tree/end}}
| |
| | |
| ==Do's==
| |
| ===Assessment===
| |
| * The presence of purulent [[sputum]] during an exacerbation can be sufficient indication for starting empirical antibiotic treatment.<ref name="Stockley-2000">{{Cite journal |last1 = Stockley | first1 = RA. | last2 = O'Brien | first2 = C. | last3 = Pye | first3 = A. | last4 = Hill | first4 = SL. | title = Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. | journal = Chest | volume = 117 | issue = 6 | pages = 1638-45 | month = Jun | year = 2000 | doi = | PMID = 10858396 }}</ref>
| |
| | |
| ===Treatment===
| |
| ======Treatment Setting======
| |
| * When a patient comes to the [[ED]], the first actions are to provide controlled [[oxygen therapy]] and to determine whether the exacerbation is life-threatening. If so, the patient should be admitted to the [[ICU]] immediately.<ref name="Vestbo-2013">{{Cite journal | last1 = Vestbo | first1 = J. | last2 = Hurd|first2 = SS. | last3 = Agustí |first3 = AG. | last4 = Jones | first4 = PW. | last5 = Vogelmeier | first5 = C. | last6 = Anzueto | first6 = A. | last7 = Barnes | first7 = PJ. | last8 = Fabbri | first8 = LM. | last9 = Martinez | first9 = FJ. | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. | journal = Am J Respir Crit Care Med | volume = 187 | issue = 4 | pages = 347-65 | month = Feb | year = 2013 | doi = 10.1164/rccm.201204-0596PP | PMID = 22878278}}</ref>
| |
| | |
| ======Short-Acting Bronchodilators======
| |
| * Short-acting inhaled [[Beta2-adrenergic receptor agonist|β2-agonists]] with or without short-acting [[anticholinergic]]s are usually the preferred [[bronchodilator]]s for treatment of an exacerbation.<ref name="Celli-2004">{{Cite journal | last1 = Celli | first1 = BR. | last2 = MacNee | first2 = W. | title = Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. | journal = Eur Respir J | volume = 23 | issue = 6 | pages = 932-46 | month = Jun | year = 2004 | doi = | PMID = 15219010 }}</ref>
| |
| | |
| * A systematic review found no significant differences in [[FEV1|FEV<sub>1</sub>]] between [[Metered-dose inhaler|MDI]] and [[Nebulizer|nebulizers]],<ref name="Turner-">{{Cite journal | last1 = Turner | first1 = MO. | last2 = Patel | first2 = A. | last3 = Ginsburg | first3 = S. | last4 = FitzGerald | first4 = JM. | title = Bronchodilator delivery in acute airflow obstruction. A meta-analysis. | journal = Arch Intern Med | volume = 157 | issue = 15 | pages = 1736-44 | month = | year = | doi = | PMID = 9250235 }}</ref>although the latter can be more convenient for sicker or frail patients.
| |
| | |
| * Intravenous [[methylxanthine]]s ([[theophylline]] or [[aminophylline]]) are only to be used in selected cases when there is insufficient response to [[SABA|short-acting bronchodilators]].<ref name="Barberá-1992">{{Cite journal | last1 = Barberá | first1 = JA. | last2 = Reyes | first2 = A. | last3 = Roca | first3 = J. | last4 = Montserrat | first4 = JM. | last5 = Wagner | first5 = PD. | last6 = Rodríguez-Roisin | first6 = R. | title = Effect of intravenously administered aminophylline on ventilation/perfusion inequality during recovery from exacerbations of chronic obstructive pulmonary disease. | journal = Am Rev Respir Dis | volume = 145 | issue = 6 | pages = 1328-33 | month = Jun | year = 1992|doi = 10.1164/ajrccm/145.6.1328 | PMID = 1595998 }}</ref><ref name="Emerman-1990">{{Cite journal | last1 = Emerman | first1 = CL. | last2 = Connors | first2 = AF. | last3 = Lukens| first3 = TW. | last4 = May | first4 = ME. | last5 = Effron | first5 = D. | title = Theophylline concentrations in patients with acute exacerbation of COPD. | journal = Am J Emerg Med | volume = 8 | issue = 4 | pages = 289-92 | month = Jul | year = 1990 | doi = | PMID = 2363749 }}</ref><ref name="Lloberes-1988">{{Cite journal | last1 = Lloberes |first1 = P. | last2 = Ramis | first2 = L. | last3 = Montserrat | first3 = JM. | last4 = Serra | first4 = J. | last5 = Campistol | first5 = J. | last6 = Picado | first6 = C. | last7 = Agusti-Vidal | first7 = A. | title = Effect of three different bronchodilators during an exacerbation of chronic obstructive pulmonary disease. | journal = Eur Respir J | volume = 1 |issue = 6 | pages = 536-9 | month = Jun | year = 1988 | doi = | PMID = 2971565 }}</ref><ref name="Mahon-1999">{{Cite journal | last1 = Mahon | first1 = JL. | last2 = Laupacis|first2 = A. | last3 = Hodder | first3 = RV. | last4 = McKim | first4 = DA. | last5 = Paterson | first5 = NA. | last6 = Wood | first6 = TE. | last7 = Donner | first7 = A. | title = Theophylline for irreversible chronic airflow limitation: a randomized study comparing n of 1 trials to standard practice. | journal = Chest | volume = 115 | issue = 1 | pages = 38-48 | month = Jan | year = 1999 | doi = | PMID = 9925061 }}</ref><ref name="Murciano-1984">{{Cite journal | last1 = Murciano | first1 = D. | last2 = Aubier | first2 = M. | last3 = Lecocguic | first3 = Y. | last4 = Pariente | first4 = R. | title = Effects of theophylline on diaphragmatic strength and fatigue in patients with chronic obstructive pulmonary disease. | journal = N Engl J Med | volume = 311 | issue = 6 | pages = 349-53 | month = Aug | year = 1984 | doi = 10.1056/NEJM198408093110601 | PMID = 6738652 }}</ref><ref>{{Cite web | last = | first = | title = http://www.nice.org.uk/nicemedia/live/13029/49397/49397.pdf | url = http://www.nice.org.uk/nicemedia/live/13029/49397/49397.pdf | publisher = |date = | accessdate = 18 December 2013 }}</ref>
| |
| | |
| ======Corticosteroids======
| |
| * Systemic [[corticosteroids]] in COPD exacerbations shorten recovery time, improve [[FEV1|FEV<sub>1</sub>]] and [[PaO2|Pa<sub>O<sub>2</sub></sub>]],<ref name="Davies-1999">{{Cite journal | last1 = Davies | first1 = L. | last2 = Angus | first2 = RM. | last3 = Calverley | first3 = PM. | title = Oral corticosteroids in patients admitted to hospital with exacerbations of chronic obstructive pulmonary disease: a prospective randomised controlled trial. | journal = Lancet | volume = 354 | issue = 9177 | pages = 456-60 | month = Aug|year = 1999 | doi = | PMID = 10465169 }}</ref><ref name="Maltais-2002">{{Cite journal | last1 = Maltais | first1 = F. | last2 = Ostinelli | first2 = J. | last3 = Bourbeau |first3 = J. | last4 = Tonnel | first4 = AB. | last5 = Jacquemet | first5 = N. | last6 = Haddon | first6 = J. | last7 = Rouleau | first7 = M. | last8 = Boukhana | first8 = M. | last9 = Martinot | first9 = JB. | title = Comparison of nebulized budesonide and oral prednisolone with placebo in the treatment of acute exacerbations of chronic obstructive pulmonary disease: a randomized controlled trial. | journal = Am J Respir Crit Care Med | volume = 165 | issue = 5 | pages = 698-703 | month = Mar | year = 2002 | doi = 10.1164/ajrccm.165.5.2109093 | PMID = 11874817 }}</ref><ref name="Niewoehner-1999">{{Cite journal | last1 = Niewoehner | first1 = DE. | last2 = Erbland | first2 = ML. | last3 = Deupree | first3 = RH. | last4 = Collins | first4 = D. |last5 = Gross | first5 = NJ. | last6 = Light | first6 = RW. | last7 = Anderson | first7 = P. | last8 = Morgan | first8 = NA.|title = Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. Department of Veterans Affairs Cooperative Study Group. | journal = N Engl J Med | volume = 340 | issue = 25 | pages = 1941-7| month = Jun | year = 1999 | doi = 10.1056/NEJM199906243402502 | PMID = 10379017 }}</ref><ref name="Thompson-1996">{{Cite journal |last1 = Thompson | first1 = WH. | last2 = Nielson | first2 = CP. | last3 = Carvalho | first3 = P. | last4 = Charan | first4 = NB. | last5 = Crowley | first5 = JJ. | title = Controlled trial of oral prednisone in outpatients with acute COPD exacerbation. | journal = Am J Respir Crit Care Med | volume = 154 | issue = 2 Pt 1 | pages = 407-12 | month = Aug| year = 1996 | doi = 10.1164/ajrccm.154.2.8756814 | PMID = 8756814 }}</ref> and reduce the risk of early relapse, treatment failure, and length of hospital stay.<ref name="Davies-1999">{{Cite journal | last1 = Davies | first1 = L. | last2 = Angus | first2 = RM. | last3 = Calverley | first3 = PM. | title = Oral corticosteroids in patients admitted to hospital with exacerbations of chronic obstructive pulmonary disease: a prospective randomised controlled trial. | journal = Lancet | volume = 354 | issue = 9177 | pages = 456-60 |month = Aug | year = 1999 | doi = | PMID = 10465169 }}</ref><ref name="Niewoehner-1999">{{Cite journal | last1 = Niewoehner | first1 = DE. | last2 = Erbland | first2 = ML. | last3 = Deupree | first3 = RH. | last4 = Collins | first4 = D. | last5 = Gross | first5 = NJ. | last6 = Light | first6 = RW. | last7 = Anderson | first7 = P. | last8 = Morgan|first8 = NA. | title = Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. Department of Veterans Affairs Cooperative Study Group. |journal = N Engl J Med | volume = 340 | issue = 25 | pages = 1941-7 | month = Jun | year = 1999 | doi = 10.1056/NEJM199906243402502 | PMID = 10379017 }}</ref><ref name="Aaron-2003">{{Cite journal |last1 = Aaron | first1 = SD. | last2 = Vandemheen | first2 = KL. | last3 = Hebert | first3 = P. | last4 = Dales | first4 = R. | last5 = Stiell | first5 = IG. |last6 = Ahuja | first6 = J. | last7 = Dickinson | first7 = G. | last8 = Brison | first8 = R. | last9 = Rowe | first9 = BH. | title = Outpatient oral prednisone after emergency treatment of chronic obstructive pulmonary disease. | journal = N Engl J Med | volume = 348 | issue = 26 | pages = 2618-25 | month = Jun | year = 2003 | doi = 10.1056/NEJMoa023161 |PMID = 12826636 }}</ref>
| |
| | |
| * Consensus on optimal [[corticosteroids]] dose and duration for COPD exacerbations has not been reached.<ref name="Walters-2009">{{Cite journal | last1 = Walters | first1 = JA.|last2 = Gibson | first2 = PG. | last3 = Wood-Baker | first3 = R. | last4 = Hannay | first4 = M. | last5 = Walters | first5 = EH. | title = Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. | journal = Cochrane Database Syst Rev | volume = | issue = 1 | pages = CD001288 | month = | year = 2009 | doi = 10.1002/14651858.CD001288.pub3 | PMID = 19160195 }}</ref>
| |
| | |
| ======Antibiotics======
| |
| * ''[[Haemophilus influenzae]]'', ''[[Streptococcus pneumoniae]]'', and ''[[Moraxella catarrhalis]]'' are the most common bacterial pathogens involved in an exacerbation.<ref name="Sethi-2008">{{Cite journal | last1 = Sethi | first1 = S. | last2 = Murphy | first2 = TF. | title = Infection in the pathogenesis and course of chronic obstructive pulmonary disease. | journal = N Engl J Med | volume = 359 | issue = 22 | pages = 2355-65 | month = Nov | year = 2008 | doi = 10.1056/NEJMra0800353 | PMID = 19038881 }}</ref> However, the choice of the antibiotic should be based on the local bacterial resistance pattern.
| |
| | |
| * Empirical coverage of ''[[Pseudomonas aeruginosa]]'' in GOLD 3 and GOLD 4 patients is important.<ref name="Vestbo-2013">{{Cite journal | last1 = Vestbo | first1 = J. | last2 = Hurd |first2 = SS. | last3 = Agustí |first3 = AG. | last4 = Jones | first4 = PW. | last5 = Vogelmeier | first5 = C. | last6 = Anzueto | first6 = A. | last7 = Barnes | first7 = PJ.|last8 = Fabbri | first8 = LM. | last9 = Martinez | first9 = FJ. | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. | journal = Am J Respir Crit Care Med | volume = 187 | issue = 4 | pages = 347-65 | month = Feb | year = 2013 | doi = 10.1164/rccm.201204-0596PP | PMID = 22878278}}</ref>
| |
| | |
| * [[Procalcitonin]] may be of value in the decision to use antibiotics.<ref name="Christ-Crain-2004">{{Cite journal | last1 = Christ-Crain | first1 = M. | last2 = Jaccard-Stolz|first2 = D. | last3 = Bingisser | first3 = R. | last4 = Gencay | first4 = MM. | last5 = Huber | first5 = PR. | last6 = Tamm | first6 = M. | last7 = Müller | first7 = B. | title = Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. | journal = Lancet | volume = 363 | issue = 9409 | pages = 600-7 | month = Feb | year = 2004 | doi = 10.1016/S0140-6736(04)15591-8 | PMID = 14987884 }}</ref>
| |
| | |
| ======Adjunct Therapies======
| |
| * An appropriate fluid balance with special attention to the administration of [[diuretic]]s, [[anticoagulant]]s, treatment of [[comorbidities]], and nutritional aspects should be considered.<ref name="Vestbo-2013">{{Cite journal | last1 = Vestbo | first1 = J. | last2 = Hurd | first2 = SS. | last3 = Agustí| first3 = AG. | last4 = Jones | first4 = PW. | last5 = Vogelmeier | first5 = C. | last6 = Anzueto | first6 = A. | last7 = Barnes | first7 = PJ. | last8 = Fabbri | first8 = LM. |last9 = Martinez | first9 = FJ. | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. | journal = Am J Respir Crit Care Med | volume = 187 | issue = 4|pages = 347-65 | month = Feb | year = 2013 | doi = 10.1164/rccm.201204-0596PP | PMID = 22878278 }}</ref>
| |
| | |
| * Healthcare providers should strongly enforce stringent measures against active [[cigarette]] smoking.<ref name="Vestbo-2013">{{Cite journal | last1 = Vestbo | first1 = J. | last2 = Hurd | first2 = SS. | last3 = Agustí| first3 = AG. | last4 = Jones | first4 = PW. | last5 = Vogelmeier | first5 = C. | last6 = Anzueto | first6 = A. | last7 = Barnes | first7 = PJ. | last8 = Fabbri | first8 = LM. |last9 = Martinez | first9 = FJ. | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. | journal = Am J Respir Crit Care Med | volume = 187 | issue = 4 | pages = 347-65 | month = Feb | year = 2013 | doi = 10.1164/rccm.201204-0596PP|PMID = 22878278 }}</ref>
| |
| | |
| ======Respiratory Support======
| |
| * Once oxygen is started, [[arterial blood gases]] should be checked 30 to 60 minutes later to ensure satisfactory [[oxygenation]] without [[carbon dioxide]] retention or[[acidosis]].<ref name="Vestbo-2013">{{Cite journal | last1 = Vestbo | first1 = J. | last2 = Hurd | first2 = SS. | last3 = Agustí| first3 = AG. | last4 = Jones | first4 = PW.|last5 = Vogelmeier | first5 = C. | last6 = Anzueto | first6 = A. | last7 = Barnes | first7 = PJ. | last8 = Fabbri | first8 = LM. |last9 = Martinez | first9 = FJ. | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. | journal = Am J Respir Crit Care Med | volume = 187 | issue = 4 | pages = 347-65 | month = Feb | year = 2013 | doi = 10.1164/rccm.201204-0596PP |PMID = 22878278 }}</ref>
| |
| | |
| * [[Venturi mask]]s offer more accurate and controlled delivery of [[oxygen]] than do [[Nasal cannula|nasal prongs]] but are less likely to be tolerated by the patient.<ref name="Celli-2004">{{Cite journal | last1 = Celli | first1 = BR. | last2 = MacNee | first2 = W. | title = Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. | journal = Eur Respir J | volume = 23 | issue = 6 | pages = 932-46 | month = Jun | year = 2004 | doi = | PMID = 15219010 }}</ref>
| |
| | |
| * Noninvasive [[mechanical ventilation]] improves [[respiratory acidosis]] and decreases [[respiratory rate]], severity of breathlessness, complications such as [[ventilator-associated pneumonia]], length of hospital stay, [[mortality]], and [[intubation]] rates.<ref name="Brochard-1995">{{Cite journal | last1 = Brochard | first1 = L. | last2 = Mancebo| first2 = J. | last3 = Wysocki | first3 = M. | last4 = Lofaso | first4 = F. | last5 = Conti | first5 = G. | last6 = Rauss | first6 = A. | last7 = Simonneau | first7 = G. |last8 = Benito | first8 = S. | last9 = Gasparetto | first9 = A. | title = Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. | journal = N Engl J Med| volume = 333 | issue = 13 | pages = 817-22 | month = Sep | year = 1995 | doi = 10.1056/NEJM199509283331301 | PMID = 7651472 }}</ref><ref name="Bott-1993">{{Cite journal | last1 = Bott | first1 = J. | last2 = Carroll | first2 = MP. | last3 = Conway | first3 = JH. | last4 = Keilty | first4 = SE. | last5 = Ward | first5 = EM. | last6 = Brown | first6 = AM. |last7 = Paul | first7 = EA. | last8 = Elliott | first8 = MW. | last9 = Godfrey | first9 = RC. | title = Randomised controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease. | journal = Lancet | volume = 341 | issue = 8860 | pages = 1555-7 | month = Jun | year = 1993 | doi = | PMID = 8099639 }}</ref><ref name="Kramer-1995">{{Cite journal | last1 = Kramer | first1 = N. | last2 = Meyer | first2 = TJ. | last3 = Meharg | first3 = J. | last4 = Cece | first4 = RD. | last5 = Hill |first5 = NS. | title = Randomized, prospective trial of noninvasive positive pressure ventilation in acute respiratory failure. | journal = Am J Respir Crit Care Med | volume = 151| issue = 6 | pages = 1799-806 | month = Jun | year = 1995 | doi = 10.1164/ajrccm.151.6.7767523 | PMID = 7767523 }}</ref><ref name="Plant-2000">{{Cite journal | last1 = Plant |first1 = PK. | last2 = Owen | first2 = JL. | last3 = Elliott | first3 = MW. | title = Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. | journal = Lancet | volume = 355 | issue = 9219 | pages = 1931-5 | month = Jun | year = 2000 | doi = |PMID = 10859037 }}</ref>
| |
| | |
| ===Hospital Discharge and Follow-up===
| |
| * In the hospital prior to discharge, patients should start [[LABA|long-acting bronchodilators]], either [[anticholinergics]] and/or [[Beta2-adrenergic receptor agonist|β2-agonists]] with or without inhaled [[corticosteroids]].<ref name="Vestbo-2013">{{Cite journal | last1 = Vestbo | first1 = J. | last2 = Hurd|first2 = SS. | last3 = Agustí |first3 = AG. | last4 = Jones | first4 = PW. | last5 = Vogelmeier | first5 = C. | last6 = Anzueto | first6 = A. | last7 = Barnes | first7 = PJ. | last8 = Fabbri | first8 = LM. | last9 = Martinez | first9 = FJ. | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. | journal = Am J Respir Crit Care Med | volume = 187 | issue = 4 | pages = 347-65 | month = Feb | year = 2013 | doi = 10.1164/rccm.201204-0596PP | PMID = 22878278}}</ref>
| |
| | |
| * For patients who are [[hypoxia|hypoxemic]] during an exacerbation, [[arterial blood gases]] and/or [[pulse oximetry]] should be evaluated prior to hospital discharge and in the following 3 months. If the patient remains hypoxemic, long-term supplemental [[oxygen therapy]] may be required.<ref name="Vestbo-2013">{{Cite journal | last1 = Vestbo | first1 = J. | last2 = Hurd|first2 = SS. | last3 = Agustí |first3 = AG. | last4 = Jones | first4 = PW. | last5 = Vogelmeier | first5 = C. | last6 = Anzueto | first6 = A. | last7 = Barnes|first7 = PJ. | last8 = Fabbri | first8 = LM. | last9 = Martinez | first9 = FJ. | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. | journal = Am J Respir Crit Care Med | volume = 187 | issue = 4 | pages = 347-65 | month = Feb | year = 2013 | doi = 10.1164/rccm.201204-0596PP | PMID = 22878278}}</ref>
| |
| | |
| ===Prevention of COPD Exacerbations===
| |
| * [[Smoking cessation]], [[influenza vaccine|influenza]] and [[pneumococcal vaccine]]s, knowledge of current therapy including inhaler technique, and treatment with [[LABA|long-acting inhaled bronchodilators]], with or without inhaled [[corticosteroids]], and [[Phosphodiesterase inhibitors#PDE4-selective inhibitors|phosphodiesterase-4 inhibitors]] are all therapies that reduce the number of exacerbations and hospitalizations.<ref name="Calverley-2007">{{Cite journal | last1 = Calverley | first1 = PM. | last2 = Anderson | first2 = JA. | last3 = Celli | first3 = B. | last4 = Ferguson | first4 = GT. | last5 = Jenkins | first5 = C. | last6 = Jones | first6 = PW. | last7 = Yates | first7 = JC. | last8 = Vestbo|first8 = J. | title = Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. | journal = N Engl J Med | volume = 356 | issue = 8 | pages = 775-89 | month = Feb | year = 2007 | doi = 10.1056/NEJMoa063070 | PMID = 17314337 }}</ref><ref name="Tashkin-2008">{{Cite journal | last1 = Tashkin | first1 = DP. | last2 = Celli|first2 = B. | last3 = Senn | first3 = S. | last4 = Burkhart | first4 = D. | last5 = Kesten | first5 = S. | last6 = Menjoge | first6 = S. | last7 = Decramer | first7 = M. | last8 = Schiavi | first8 = E. | last9 = Figueroa Casas | first9 = JC. | title = A 4-year trial of tiotropium in chronic obstructive pulmonary disease. | journal = N Engl J Med | volume = 359 | issue = 15 | pages = 1543-54 | month = Oct | year = 2008 | doi = 10.1056/NEJMoa0805800 | PMID = 18836213 }}</ref><ref name="Calverley-2009">{{Cite journal | last1 = Calverley| first1 = PM. | last2 = Rabe | first2 = KF. | last3 = Goehring | first3 = UM. | last4 = Kristiansen | first4 = S. | last5 = Fabbri | first5 = LM. | last6 = Martinez |first6 = FJ.| last7 = Abdool-Gaffar | first7 = MS. | last8 = Abdullah | first8 = IA. | last9 = Abdullah | first9 = I. | title = Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. | journal = Lancet | volume = 374 | issue = 9691 | pages = 685-94 | month = Aug | year = 2009 | doi = 10.1016/S0140-6736(09)61255-1 | PMID = 19716960}}</ref><ref name="Fabbri-2009">{{Cite journal | last1 = Fabbri | first1 = LM. | last2 = Calverley | first2 = PM. | last3 = Izquierdo-Alonso | first3 = JL. |last4 = Bundschuh |first4 = DS. | last5 = Brose | first5 = M. | last6 = Martinez | first6 = FJ. | last7 = Rabe | first7 = KF. | last8 = Abdulla | first8 = R. | last9 = Abdullah |first9 = I. | title = Roflumilast in moderate-to-severe chronic obstructive pulmonary disease treated with longacting bronchodilators: two randomised clinical trials. | journal = Lancet | volume = 374 |issue = 9691 | pages = 695-703 | month = Aug | year = 2009 | doi = 10.1016/S0140-6736(09)61252-6 | PMID = 19716961 }}</ref><ref name="Decramer-2009">{{Cite journal | last1 = Decramer | first1 = M. | last2 = Celli | first2 = B. | last3 = Kesten | first3 = S. | last4 = Lystig | first4 = T. | last5 = Mehra | first5 = S. | last6 = Tashkin| first6 = DP. |last7 = Schiavi | first7 = E. | last8 = Casas | first8 = JC. | last9 = Rhodius | first9 = E. | title = Effect of tiotropium on outcomes in patients with moderate chronic obstructive pulmonary disease (UPLIFT): a prespecified subgroup analysis of a randomised controlled trial. | journal = Lancet | volume = 374 | issue = 9696 | pages = 1171-8| month = Oct | year = 2009 | doi = 10.1016/S0140-6736(09)61298-8 | PMID = 19716598 }}</ref><ref name="Jenkins-2009">{{Cite journal | last1 = Jenkins | first1 = CR. | last2 = Jones| first2 = PW. |last3 = Calverley | first3 = PM. | last4 = Celli | first4 = B. | last5 = Anderson | first5 = JA. | last6 = Ferguson | first6 = GT. | last7 = Yates | first7 = JC. |last8 = Willits |first8 = LR. | last9 = Vestbo | first9 = J. | title = Efficacy of salmeterol/fluticasone propionate by GOLD stage of chronic obstructive pulmonary disease: analysis from the randomised, placebo-controlled TORCH study. | journal = Respir Res | volume = 10 | issue = | pages = 59 | month = | year = 2009 | doi = 10.1186/1465-9921-10-59 | PMID = 19566934}}</ref>
| |
| | |
| * Early outpatient [[pulmonary rehabilitation]] after hospitalization for an exacerbation is safe and results in clinically significant improvements in exercise capacity and health status at 3 months.<ref name="Man-2004">{{Cite journal | last1 = Man | first1 = WD. | last2 = Polkey | first2 = MI. | last3 = Donaldson | first3 = N. | last4 = Gray | first4 = BJ.|last5 = Moxham | first5 = J. | title = Community pulmonary rehabilitation after hospitalisation for acute exacerbations of chronic obstructive pulmonary disease: randomised controlled study. | journal = BMJ | volume = 329 | issue = 7476 | pages = 1209 | month = Nov | year = 2004 | doi = 10.1136/bmj.38258.662720.3A | PMID = 15504763 }}</ref>
| |
| | |
| ==Don'ts==
| |
| ===Assessment===
| |
| * [[Spirometry]] is '''not''' recommended during an exacerbation because it can be difficult to perform and measurements are not accurate enough.<ref name="Vestbo-2013">{{Cite journal | last1 = Vestbo | first1 = J. | last2 = Hurd|first2 = SS. | last3 = Agustí |first3 = AG. | last4 = Jones | first4 = PW. | last5 = Vogelmeier | first5 = C. | last6 = Anzueto | first6 = A. | last7 = Barnes | first7 = PJ. | last8 = Fabbri | first8 = LM. | last9 = Martinez | first9 = FJ. | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. | journal = Am J Respir Crit Care Med | volume = 187 | issue = 4 | pages = 347-65 | month = Feb | year = 2013 | doi = 10.1164/rccm.201204-0596PP | PMID = 22878278}}</ref>
| |
| | |
| ===Treatment===
| |
| ======Adjunct Therapies======
| |
| * The use of [[Mucolytic agent|mucolytics]] is '''not''' well-supported by evidence.<ref name="McCrory-2001">{{Cite journal | last1 = McCrory | first1 = DC. | last2 = Brown |first2 = C. | last3 = Gelfand | first3 = SE. | last4 = Bach | first4 = PB. | title = Management of acute exacerbations of COPD: a summary and appraisal of published evidence. |journal = Chest | volume = 119 | issue = 4 | pages = 1190-209 | month = Apr | year = 2001 | doi = | PMID = 11296189 }}</ref>
| |
| | |
| ======Respiratory Support======
| |
| * NIPPV is '''not''' considered in the following conditions:
| |
| | |
| {{Family tree/start}}
| |
| {{Family tree |border=2|boxstyle=background: WhiteSmoke;|A1|A1=<div style="float: left; text-align: left; height: 16em; width: 27em; padding: 1em;">'''Contraindications for NIPPV'''<ref name="-2001">{{Cite journal | title = International Consensus Conferences in Intensive Care Medicine: noninvasive positive pressure ventilation in acute Respiratory failure. | journal = Am J Respir Crit Care Med | volume = 163 | issue = 1 | pages = 283-91 | month = Jan | year = 2001 | doi = 10.1164/ajrccm.163.1.ats1000 | PMID = 11208659 }}</ref> <BR> ❑ Inability to cooperate/protect the airway <BR> ❑ Inability to clear respiratory secretions <BR> ❑ Facial surgery, trauma, or deformity <BR> ❑ Upper airway obstruction <BR> ❑ High risk for aspiration <BR> ❑ Cardiac or respiratory arrest <BR> ❑ Nonrespiratory organ failure <BR> ▸ Severe encephalopathy (e.g., GCS <10) <BR> ▸ Severe upper gastrointestinal bleeding <BR> ▸ Hemodynamic instability or unstable cardiac arrhythmia</div>}}
| |
| {{Family tree/end}}
| |
| | |
| ==References==
| |
| {{Reflist|2}}
| |