Bitemporal hemianopia: Difference between revisions
mNo edit summary |
|||
| (42 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
{{SI}} | {{SI}} | ||
{{CMG}} ; {{AOEIC}}{{ADI}} | {{CMG}} ; {{AOEIC}} {{ADI}} {{NihasRM}} | ||
'''''Synonyms and keywords: ''''' Bitemporal hemianopsia | '''''Synonyms and keywords: ''''' Bitemporal hemianopsia | ||
==Overview== | ==Overview== | ||
''' | Bitemporal hemianopia (''bi-'': both eyes, ''temporal'': temporal/peripheral, ''hemi-'': half, ''anopsia'': blindness) is defect in [[visual pathway]] causing loss of [[Visual perception|sight]] in the outer half of the [[visual field]]. A lesion compressing or disrupting [[optic chiasm]] would result in bitemporal hemianopia. Additional symptoms such as [[Headache]], [[Diplopia]], [[Endocrine disorders]] can be present. Most common causes are [[Pituitary tumor|Pituitary macroadenoma]], [[Craniopharyngioma]], [[Meningioma]] and [[Aneurysm of anterior communicating artery|Aneurysm of anterior communicating artery.]] [[Visual field defect|Visual field defects]] can be diagnosed using Standard Automated Perimetry (SAP). [[Computed tomography|CT Imaging]] and [[MRI]] usually reveal the underlying cause. While vision loss can be improved by treating the underlying cause, sometimes it can be permanent. | ||
==Historical Perspective== | |||
*First case of Bitemporal hemianopsia was reported by Clarence A. Veasey, in 1904 <ref name="pmid16692037">{{cite journal| author=Veasey CA| title=Observations of a case of bi-temporal hemianopsia with some unusual changes in the visual fields. | journal=Trans Am Ophthalmol Soc | year= 1904 | volume= 10 | issue= Pt 2 | pages= 383-7 | pmid=16692037 | doi= | pmc=1322445 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16692037 }}</ref>. | |||
*In 1929, L.S.Kubie and J.W.Beckmann documented [[Diplopia]] to be the most reported symptom in patients with bitemporal hemianopia in the absence of [[Extraocular muscle|extraocular muscle palsies]].<ref name="KubieBeckmann1929">{{cite journal|last1=Kubie|first1=L. S.|last2=Beckmann|first2=J. W.|title=DIPLOPIA WITHOUT EXTRA-OCULAR PALSIES, CAUSED BY HETERONYMOUS DEFECTS IN THE VISUAL FIELDS ASSOCIATED WITH DEFECTIVE MACULAR VISION|journal=Brain|volume=52|issue=3|year=1929|pages=317–333|issn=0006-8950|doi=10.1093/brain/52.3.317}}</ref> | |||
==Classification== | |||
*Bitemporal hemianopia may be classified according to the number of defective optic fibers into complete bitemporal hemianopia and partial bitemporal hemianopia. | |||
Bitemporal hemianopia may be classified according to the number of defective optic fibers into | |||
==Pathophysiology== | ==Pathophysiology== | ||
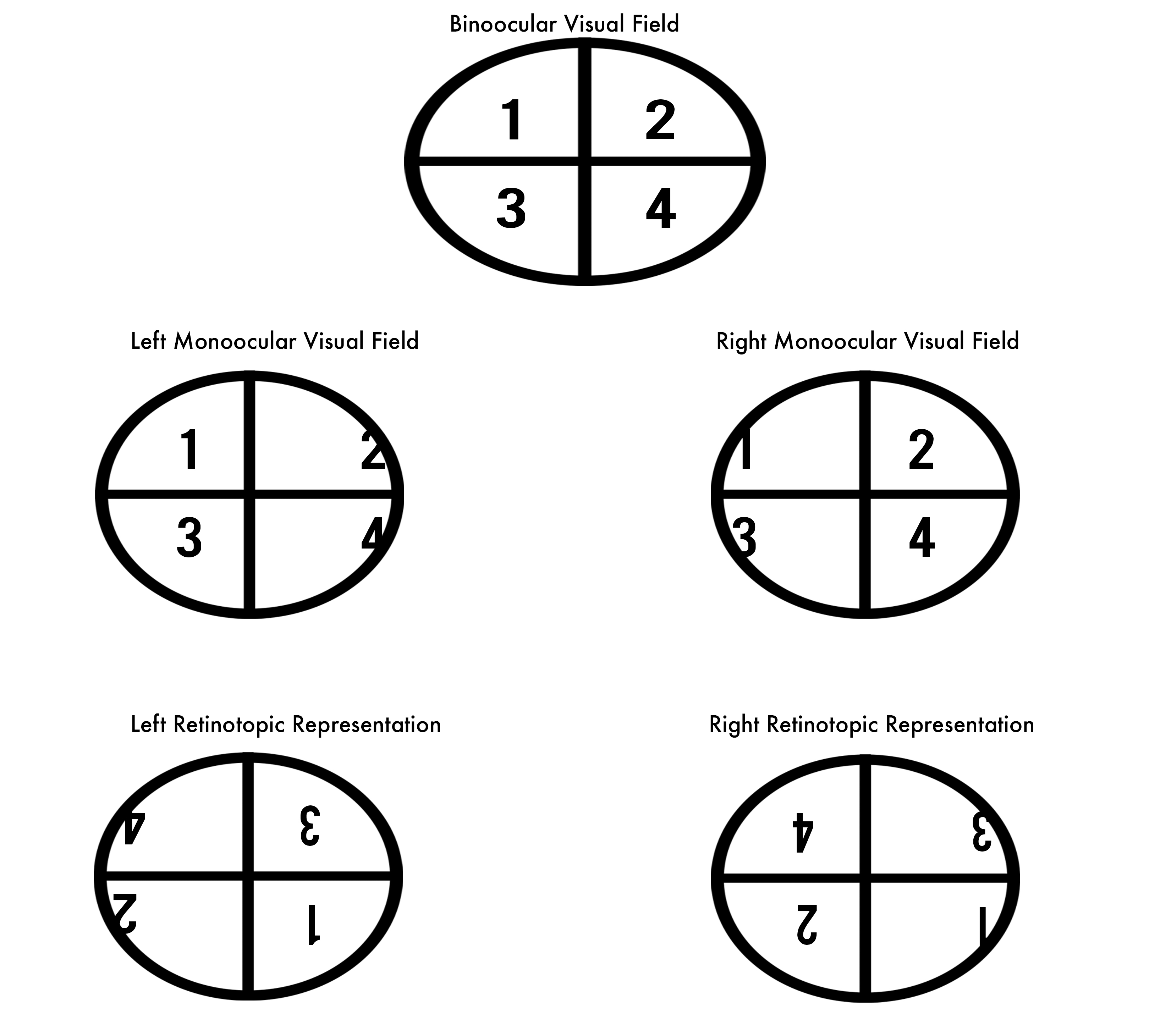
*Bitemporal hemianopia is a visual defect due to a lesion involving optic chiasm. | [[File:Retinoptic representation.jpg|alt=Comparison of visual field and retinoptic field. Picture courtesy Nihas R Mateti|thumb|Comparison of visual field and retinoptic field. Picture courtesy Nihas R Mateti|left|228x228px]] | ||
*While afferent sensory inputs from superior temporal quadrant of visual field are relayed through inferior nasal fibers of optic nerve, the inputs | <br /> | ||
*Optic chiasm is an anatomical structure in middle cranial fossa formed by decussation of nasal fibers of optic nerve travelling from retina to visual cortex. | |||
*A lesion involving optic chiasm either due to compression | *Bitemporal hemianopia is a visual defect due to a lesion involving [[optic chiasm]]. | ||
*A lesion compressing the chiasm from below (eg: | *While [[afferent]] [[sensory]] inputs from superior [[temporal]] quadrant of [[visual field]] are relayed through inferior [[nasal]] fibers of [[optic nerve]], the inputs from inferior [[temporal]] quadrant are relayed through superior [[nasal]] [[Fiber|fibers]]. Similarly the visual information from superior nasal quadrant and inferior nasal quadrant are relayed through inferior temporal fibers and superior temporal fibers respectively.<ref name="urlThe Retinotopic Representation of the Visual Field - Neuroscience - NCBI Bookshelf">{{cite web |url=https://www.ncbi.nlm.nih.gov/books/NBK10944/ |title=The Retinotopic Representation of the Visual Field - Neuroscience - NCBI Bookshelf |format= |work= |accessdate=}}</ref> | ||
*[[Optic chiasm]] is an anatomical structure in [[middle cranial fossa]] formed by [[decussation]] of nasal fibers of [[optic nerve]] travelling from [[retina]] to [[visual cortex]]. | |||
*A lesion involving [[optic chiasm]] either due to compression or vascular compromise, disrupts nasal fibers of [[optic nerve]] almost always resulting in [[bilateral]] defects in [[temporal]] half of [[visual field]].<ref name="pmid5381296">{{cite journal| author=Hedges TR| title=Preservation of the upper nasal field in the chiasmal syndrome: an anatomic explanation. | journal=Trans Am Ophthalmol Soc | year= 1969 | volume= 67 | issue= | pages= 131-41 | pmid=5381296 | doi= | pmc=1310336 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=5381296 }}</ref><ref name="pmid5811834">{{cite journal| author=Bergland R| title=The arterial supply of the human optic chiasm. | journal=J Neurosurg | year= 1969 | volume= 31 | issue= 3 | pages= 327-34 | pmid=5811834 | doi=10.3171/jns.1969.31.3.0327 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=5811834 }}</ref> | |||
*[[Nasal|Nasal fibers]] have predilection for greater pressure due to compression causing them to be easily disrupted(Mechanical theory).<ref name="pmid15756133">{{cite journal| author=McIlwaine GG, Carrim ZI, Lueck CJ, Chrisp TM| title=A mechanical theory to account for bitemporal hemianopia from chiasmal compression. | journal=J Neuroophthalmol | year= 2005 | volume= 25 | issue= 1 | pages= 40-3 | pmid=15756133 | doi=10.1097/00041327-200503000-00011 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15756133 }}</ref> | |||
*A lesion compressing the [[Optic chiasm|chiasm]] from below (eg: [[pituitary tumors]]) will have predominant defects in superior temporal quadrants along with partial defects in the inferior temporal quadrant and Vice-versa. | |||
==Causes== | ==Causes== | ||
===Common Causes=== | ===Common Causes=== | ||
Most of the common causes of bitemporal hemianopia are due to disorders of the pituitary gland and its surrounding structures. | |||
*[[Pituitary tumor|Pituitary macroadenoma]] | *[[Pituitary tumor|Pituitary macroadenoma]]<ref name="pmid24010395">{{cite journal| author=Lake MG, Krook LS, Cruz SV| title=Pituitary adenomas: an overview. | journal=Am Fam Physician | year= 2013 | volume= 88 | issue= 5 | pages= 319-27 | pmid=24010395 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24010395 }}</ref> | ||
*[[Craniopharyngioma]] | *[[Craniopharyngioma]]<ref name="pmid24467716">{{cite journal| author=Müller HL| title=Craniopharyngioma. | journal=Endocr Rev | year= 2014 | volume= 35 | issue= 3 | pages= 513-43 | pmid=24467716 | doi=10.1210/er.2013-1115 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24467716 }}</ref> | ||
*[[Meningioma]] | *[[Meningioma]]<ref name="pmid11950417">{{cite journal| author=Bejjani GK, Cockerham KP, Kennerdell JS, Maroon JC| title=Visual field deficit caused by vascular compression from a suprasellar meningioma: case report. | journal=Neurosurgery | year= 2002 | volume= 50 | issue= 5 | pages= 1129-31; discussion 1131-2 | pmid=11950417 | doi=10.1097/00006123-200205000-00033 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11950417 }}</ref> | ||
*[[Aneurysm]] | *[[Aneurysm of anterior communicating artery|Aneurysm of anterior communicating artery<ref name="pmid26539276">{{cite journal| author=Seung WB, Kim DY, Park YS| title=A Large Ruptured Anterior Communicating Artery Aneurysm Presenting with Bitemporal Hemianopsia. | journal=J Korean Neurosurg Soc | year= 2015 | volume= 58 | issue= 3 | pages= 291-3 | pmid=26539276 | doi=10.3340/jkns.2015.58.3.291 | pmc=4630364 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26539276 }}</ref>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]][[Bitemporal hemianopia#cite%20note-pmid26539276-10|<span class="mw-reflink-text">[10]</span>]] | ||
===Causes by Organ System=== | ===Causes by Organ System=== | ||
| Line 59: | Line 48: | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
|'''Dermatologic''' | |'''Dermatologic''' | ||
| bgcolor="Beige" |[[Dermatochalasis]] | | bgcolor="Beige" |[[Dermatochalasis]]<ref name="pmid12644764">{{cite journal| author=Fay A, Lee LC, Pasquale LR| title=Dermatochalasis causing apparent bitemporal hemianopsia. | journal=Ophthalmic Plast Reconstr Surg | year= 2003 | volume= 19 | issue= 2 | pages= 151-3 | pmid=12644764 | doi=10.1097/01.IOP.0000055827.78632.CA | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12644764 }}</ref> | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
|'''Drug Side Effect''' | |'''Drug Side Effect''' | ||
| bgcolor="Beige" |[[Chloroquine retinopathy]] | | bgcolor="Beige" |[[Chloroquine retinopathy]]<ref name="GoldhammerSmith1974">{{cite journal|last1=Goldhammer|first1=Y.|last2=Smith|first2=J. L.|title=Bitemporal hemianopia in chloroquine retinopathy|journal=Neurology|volume=24|issue=12|year=1974|pages=1135–1135|issn=0028-3878|doi=10.1212/WNL.24.12.1135}}</ref>, [[Ethambutol]] [[toxicity]]<ref name="pmid24094504">{{cite journal| author=Boulanger Scemama E, Touitou V, Le Hoang P| title=[Bitemporal hemianopia as presenting sign of severe ethambutol toxicity]. | journal=J Fr Ophtalmol | year= 2013 | volume= 36 | issue= 9 | pages= e163-7 | pmid=24094504 | doi=10.1016/j.jfo.2012.12.008 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24094504 }}</ref> | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| Line 103: | Line 92: | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
|'''Neurologic''' | |'''Neurologic''' | ||
| bgcolor="Beige" | | | bgcolor="Beige" |[[Craniopharyngioma]], [[Aneurysm of anterior communicating artery]], [[Intracranial vascular loop]], [[Meningioma]], [[Enlarged third ventricle]]<ref name="OsherCorbett1978">{{cite journal|last1=Osher|first1=R. H.|last2=Corbett|first2=J. J.|last3=Schatz|first3=N. J.|last4=Savino|first4=P. J.|last5=Orr|first5=L. S.|title=Neuro-ophthalmological complications of enlargement of the third ventricle.|journal=British Journal of Ophthalmology|volume=62|issue=8|year=1978|pages=536–542|issn=0007-1161|doi=10.1136/bjo.62.8.536}}</ref>, [[Glioma of third ventricle]]<ref name="pmid26668411">{{cite journal| author=Thavaratnam LK, Loy ST, Gupta A, Ng I, Cullen JF| title=Chordoid glioma. | journal=Singapore Med J | year= 2015 | volume= 56 | issue= 11 | pages= 641-3 | pmid=26668411 | doi=10.11622/smedj.2015175 | pmc=4656874 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26668411 }}</ref>, [[Chronic chiasmal arachnoiditis]]<ref name="pmid13618533">{{cite journal| author=GIBBS DC| title=Chiasmal arachnoiditis. | journal=Br J Ophthalmol | year= 1959 | volume= 43 | issue= 1 | pages= 52-6 | pmid=13618533 | doi=10.1136/bjo.43.1.52 | pmc=512211 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13618533 }}</ref>, [[Suprasellar tumors|Suprasellar tumors<ref name="pmid18170220">{{cite journal| author=Lodge WO| title=BITEMPORAL HEMIANOPIA. | journal=Br J Ophthalmol | year= 1946 | volume= 30 | issue= 5 | pages= 276-81 | pmid=18170220 | doi= | pmc=510604 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18170220 }}</ref>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-17|<span class="mw-reflink-text">[17]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-14|<span class="mw-reflink-text">[14]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid18170220-13|<span class="mw-reflink-text">[13]</span>]], [[Adamantinoma of sella turcica]]<ref name="pmid18170220" />, [[Optic neuropathy|Optic neuropathy<ref name="pmid24094504" />]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-13|<span class="mw-reflink-text">[13]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-8|<span class="mw-reflink-text">[8]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-7|<span class="mw-reflink-text">[7]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-7|<span class="mw-reflink-text">[7]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-7|<span class="mw-reflink-text">[7]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-7|<span class="mw-reflink-text">[7]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-7|<span class="mw-reflink-text">[7]</span>]][[Bitemporal hemianopia#cite%20note-pmid24094504-7|<span class="mw-reflink-text">[7]</span>]], [[Traumatic chiasmal syndrome]]<ref name="Yazici2015">{{cite journal|last1=Yazici|first1=Bulent|title=Isolated Bitemporal Hemianopsia Due to Traumatic Chiasmal Syndrome|journal=Turkish Journal of Trauma and Emergency Surgery|year=2015|issn=1306696X|doi=10.5505/tjtes.2015.90540}}</ref>, [[Dolichoectasia of internal carotid arteries]]<ref name="pmid2139057">{{cite journal| author=Slavin ML| title=Bitemporal hemianopia associated with dolichoectasia of the intracranial carotid arteries. | journal=J Clin Neuroophthalmol | year= 1990 | volume= 10 | issue= 1 | pages= 80-1 | pmid=2139057 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2139057 }}</ref> | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| Line 111: | Line 100: | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
|'''Obstetric/Gynecologic''' | |'''Obstetric/Gynecologic''' | ||
| bgcolor="Beige" |[[Hypophyseal hypertrophy in pregnancy]] | | bgcolor="Beige" |[[Hypophyseal hypertrophy in pregnancy]]<ref name="pmid14082282">{{cite journal| author=PEARCE HM| title=PHYSIOLOGIC BITEMPORAL HEMIANOPSIA IN PREGNANCY. | journal=Obstet Gynecol | year= 1963 | volume= 22 | issue= | pages= 612-4 | pmid=14082282 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14082282 }}</ref> | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| Line 119: | Line 108: | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
|'''Opthalmologic''' | |'''Opthalmologic''' | ||
| bgcolor="Beige" |[[Dermatochalasis]], [[Optic neuropathy]], [[Optic chiasmal syndrome]], [[Bilateral blepharoptosis]], [[Traumatic chiasmal syndrome]] | | bgcolor="Beige" |[[Dermatochalasis]], [[Optic neuropathy]], [[Optic chiasmal syndrome]], [[Bilateral blepharoptosis]]<ref name="pmid21158577">{{cite journal| author=Levine BM, Lelli GJ| title=Bitemporal hemianopia caused by bilateral blepharoptosis. | journal=Orbit | year= 2010 | volume= 29 | issue= 6 | pages= 351-3 | pmid=21158577 | doi=10.3109/01676830.2010.516467 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21158577 }}</ref>, [[Traumatic chiasmal syndrome]], [[Retinal disorders]]<ref>{{cite journal|title=Bitemporal Hemianopia Caused by Retinal Disease|journal=Archives of Ophthalmology|volume=127|issue=12|year=2009|pages=1686|issn=0003-9950|doi=10.1001/archophthalmol.2009.320}}</ref>, [[Nasal]] [[Staphylomata]] <ref name="GuptaSmith2015">{{cite journal|last1=Gupta|first1=Anjali|last2=Smith|first2=J. M. Alaric|title=Bitemporal Hemianopia Secondary to Nasal Staphylomata|journal=Journal of Neuro-Ophthalmology|volume=35|issue=1|year=2015|pages=99–101|issn=1070-8022|doi=10.1097/WNO.0000000000000202}}</ref>, Tilted disc syndrome<ref name="pmid10543654">{{cite journal| author=Manfrè L, Vero S, Focarelli-Barone C, Lagalla R| title=Bitemporal pseudohemianopia related to the "tilted disk" syndrome: CT, MR, and fundoscopic findings. | journal=AJNR Am J Neuroradiol | year= 1999 | volume= 20 | issue= 9 | pages= 1750-1 | pmid=10543654 | doi= | pmc=7056191 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10543654 }}</ref> | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
|'''Overdose / Toxicity''' | |'''Overdose / Toxicity''' | ||
| bgcolor="Beige" | | | bgcolor="Beige" |[[Ethambutol]] [[toxicity]] | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| Line 163: | Line 152: | ||
|} | |} | ||
== | ==Differentiating Bitemporal hemianopia from other Diseases== | ||
*Bitemporal hemiaopia must be differentiated from most common causes: [[pituitary adenoma]], [[suprasellar tumors|suprasellar tumors]] [[craniopharyngioma]], [[aneurysm of anterior communicating artery]] and [[meningioma|meningioma.]] | |||
====Differential diagnosis of Bitemporal hemianopia==== | |||
{| style="width:80%; height:100px" border="1" | |||
| style="width:25%" bgcolor="LightSteelBlue" ; border="1" |[[Pituitary adenoma|'''Pituitary adenoma''']] | |||
| style="width:75%" bgcolor="Beige" ; border="1" |Functional [[adenoma]] - [[Endocrine]] abnormalities, Non functional [[adenoma]] - exert pressure symptoms ([[Headache]]). Isointense on [[Magnetic resonance imaging|MRI]]. | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|[[Suprasellar tumors|'''Suprasellar tumors''']] '''[[Craniopharyngioma]]''' | |||
| bgcolor="Beige" |[[Headache]], [[Seizure]], Focal neurological deficit. Calcified mass with Motor oil like fluid within the [[tumor]] on [[Magnetic resonance imaging|MRI]]. | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|[[Aneurysm of anterior communicating artery|'''Aneurysm of anterior communicating artery''']] | |||
| bgcolor="Beige" |[[Aneurysm|Unruptured aneurysm]] can be [[asymptomatic]] or mild [[headache]]. [[Aneurysm|Ruptured aneurysms]] presents with 'Worst headache of life' ([[Subarachnoid hemorrhage]]), [[Seizure|Seizures]], Focal neurological deficit. | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''[[Meningioma|Meningioma]]''' | |||
| bgcolor="Beige" |[[Headache]], [[Seizure]], Focal neurological deficit. Well circumscribed, Extra-axial mass with [[Dura|Dural]] attachment on [[Magnetic resonance imaging|MRI]]. [[Psammoma body|Psammoma bodies]] on immunohistopathology. | |||
|} | |||
== | ==Epidemiology and Demographics== | ||
*[[ | *The prevalence of [[Adenoma|pituitary adenoma]] is approximately 16.7% worldwide. Pituitary adenomas are almost always associated with bitemporal hemianopia.<ref name="pmid15274075">{{cite journal| author=Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML | display-authors=etal| title=The prevalence of pituitary adenomas: a systematic review. | journal=Cancer | year= 2004 | volume= 101 | issue= 3 | pages= 613-9 | pmid=15274075 | doi=10.1002/cncr.20412 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15274075 }}</ref> | ||
* | *There is no racial predilection to bitemporal hemianopia. | ||
== | ==Risk Factors== | ||
*There are no established risk factors for bitemporal hemianopia. | |||
==Screening== | |||
*There is insufficient evidence to recommend routine [[Screening (medicine)|screening]] for bitemporal hemianopia in a normal population. | |||
*Patients with [[asymptomatic]] [[Pituitary adenoma|pituitary adenomas]] can be screened by [[Perimetry|automated perimetry]]. | |||
*Presence of Vertical step [SN-96% SP-100%] and Temporal depression[SN-100% and SP-98%] is the criteria for diagnosis of bitemporal hemianopia. <ref name="pmid12439668">{{cite journal| author=Fujimoto N, Saeki N, Miyauchi O, Adachi-Usami E| title=Criteria for early detection of temporal hemianopia in asymptomatic pituitary tumor. | journal=Eye (Lond) | year= 2002 | volume= 16 | issue= 6 | pages= 731-8 | pmid=12439668 | doi=10.1038/sj.eye.6700165 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12439668 }}</ref> | |||
==Natural History, Complications, and Prognosis== | |||
====Natural History==== | |||
*In most of the patients, central visual field of 110°–120° (using Goldmann perimetry) is preserved and is sufficient for day to day activities. A volume perimetry demonstrates a [[Binocular vision|binocular]] [[scotoma]] beyond the [[Fixational eye movement|point of fixation]].<ref name="pmid24588535">{{cite journal| author=Peli E, Satgunam P| title=Bitemporal hemianopia; its unique binocular complexities and a novel remedy. | journal=Ophthalmic Physiol Opt | year= 2014 | volume= 34 | issue= 2 | pages= 233-42 | pmid=24588535 | doi=10.1111/opo.12118 | pmc=3947624 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24588535 }}</ref> | |||
====Complications==== | |||
*Shearing of nasal fibers (as in [[traumatic chiasmal syndrome]]) most commonly resulted in permanent [[visual loss]] and rare improvement.<ref name="BansalKumar2006">{{cite journal|last1=Bansal|first1=Shveta|last2=Kumar|first2=Nishant|last3=Kyle|first3=Graham|title=Mechanism of Bitemporal Hemianopia|journal=Journal of Neuro-Ophthalmology|volume=26|issue=3|year=2006|pages=233|issn=1070-8022|doi=10.1097/01.wno.0000235584.87674.9d}}</ref><ref name="pmid29577103">{{cite journal| author=Vellayan Mookan L, Thomas PA, Harwani AA| title=Traumatic chiasmal syndrome: A meta-analysis. | journal=Am J Ophthalmol Case Rep | year= 2018 | volume= 9 | issue= | pages= 119-123 | pmid=29577103 | doi=10.1016/j.ajoc.2018.01.029 | pmc=5861742 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29577103 }}</ref> | |||
====Prognosis==== | |||
*In patients with underlying etiology of [[Pituitary adenoma|pituitary adenomas]], an improvement or complete recovery of [[visual acuity]] or [[visual field]] post-surgery has been seen in 70-75% of cases.<ref name="urlInternet Scientific Publications">{{cite web |url=https://ispub.com/IJOVS/4/2/7588#:~:text=The%20overall%20improvement%20in%20visual,65.5%25%20of%20the%20affected%20eyes. |title=Internet Scientific Publications |format= |work= |accessdate=}}</ref><ref name="BerkmannFandino2013">{{cite journal|last1=Berkmann|first1=S|last2=Fandino|first2=J|last3=Müller|first3=B|last4=Kothbauer|first4=KF|last5=Henzen|first5=C|last6=Landolt|first6=H|title=Reply to the letter to the Editor “Visual outcomes after pituitary surgery”|journal=Swiss Medical Weekly|year=2013|issn=1424-7860|doi=10.4414/smw.2013.13803}}</ref><ref name="pmid23933694">{{cite journal| author=Lampropoulos KI, Samonis G, Nomikos P| title=Factors influencing the outcome of microsurgical transsphenoidal surgery for pituitary adenomas: a study on 184 patients. | journal=Hormones (Athens) | year= 2013 | volume= 12 | issue= 2 | pages= 254-64 | pmid=23933694 | doi=10.14310/horm.2002.1409 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23933694 }}</ref><ref name="pmid15918938">{{cite journal| author=Mortini P, Losa M, Barzaghi R, Boari N, Giovanelli M| title=Results of transsphenoidal surgery in a large series of patients with pituitary adenoma. | journal=Neurosurgery | year= 2005 | volume= 56 | issue= 6 | pages= 1222-33; discussion 1233 | pmid=15918938 | doi=10.1227/01.neu.0000159647.64275.9d | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15918938 }}</ref><ref name="pmid30700957">{{cite journal| author=Tagoe NN, Essuman VA, Bankah P, Dakurah T, Hewlett VK, Akpalu J | display-authors=etal| title=Visual Outcome of Patients with Pituitary Adenomas Following Surgery and Its Contributory Factors at a Tertiary Hospital in Ghana. | journal=Ethiop J Health Sci | year= 2019 | volume= 29 | issue= 1 | pages= 895-902 | pmid=30700957 | doi=10.4314/ejhs.v29i1.11 | pmc=6341437 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30700957 }}</ref> | |||
==Diagnosis== | |||
===Diagnostic Study of Choice=== | |||
*The diagnosis study of choice for bitemporal hemianopia is [[visual field testing]]. | |||
*[[Visual field testing]] by Standard Automated Perimetry(SAP) with favorable [[Sensitivity (tests)|sensitivity]] and early detection is preferred over Goldmann perimetry and is most common method used.<ref name="pmid7831036">{{cite journal| author=Katz J, Tielsch JM, Quigley HA, Sommer A| title=Automated perimetry detects visual field loss before manual Goldmann perimetry. | journal=Ophthalmology | year= 1995 | volume= 102 | issue= 1 | pages= 21-6 | pmid=7831036 | doi=10.1016/s0161-6420(95)31060-3 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7831036 }}</ref> | |||
*Even though frequency doubling technolgy (FDT) perimetry has increased [[Sensitivity (tests)|sensitivity]] over SAP, it cannot categorize [[Visual field defect|visual field defects]].<ref name="MonteiroMoura2007">{{cite journal|last1=Monteiro|first1=Mário Luiz Ribeiro|last2=Moura|first2=Frederico Castelo|last3=Cunha|first3=Leonardo Provetti|title=Frequency doubling perimetry in patients with mild and moderate pituitary tumor-associated visual field defects detected by conventional perimetry|journal=Arquivos Brasileiros de Oftalmologia|volume=70|issue=2|year=2007|pages=323–329|issn=0004-2749|doi=10.1590/S0004-27492007000200024}}</ref> | |||
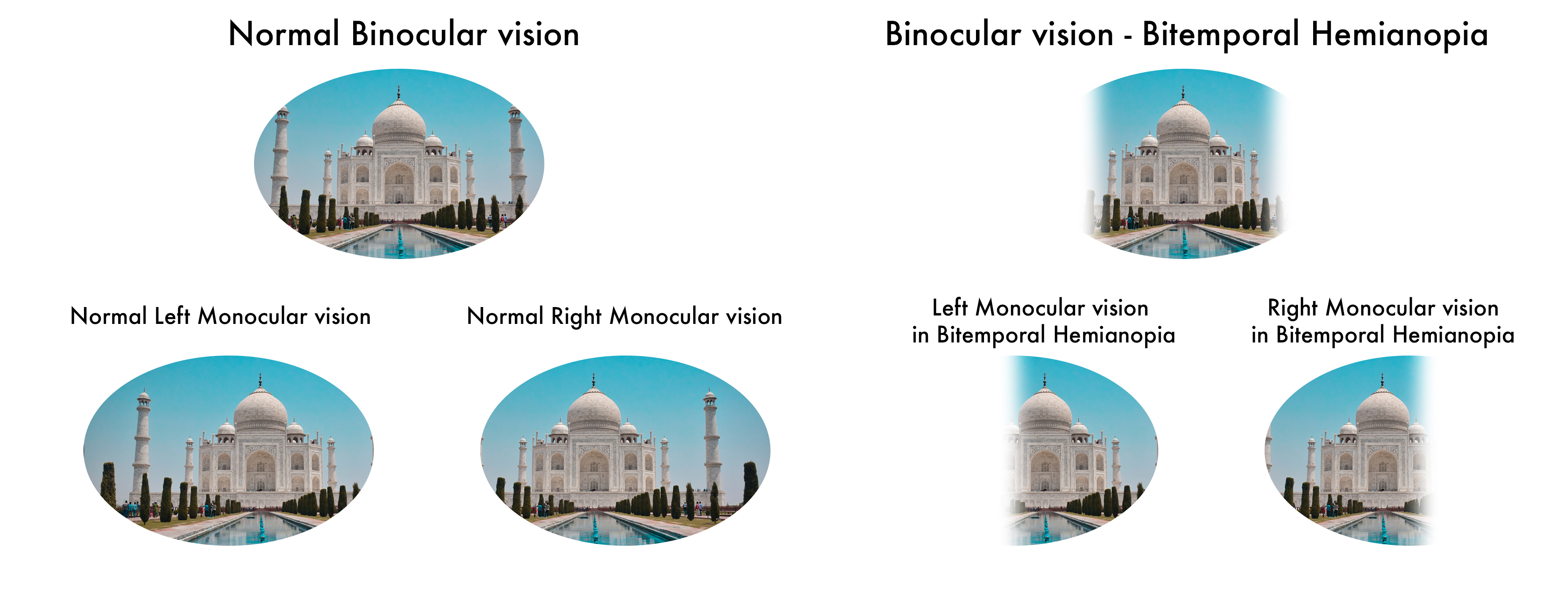
[[File:Bitemporal hemianopsia.jpg|alt=Bitemporal hemianopsia Nihas|center|thumb|700x700px|Bitemporal hemianopsia. Picture courtesy by Nihas R Mateti.]] | |||
<br /> | |||
===History and Symptoms=== | |||
*The hallmark of bitemporal hemianopia is the loss of peripheral [[vision]]. It is usually an incidental finding as there is no loss in central vision. | |||
*Presence of additional symptoms such as [[headache]], [[diplopia]], [[Endocrine diseases|endocrine disorders]] point towards underlying [[etiology]]. | |||
*History of [[chloroquine]] and [[ethambutol]] usage can be present. | |||
===Physical Examination=== | |||
*Physical examination of patients with bitemporal hemianopia is usually normal. | |||
===Laboratory Findings=== | |||
*There are no diagnostic laboratory findings associated with bitemporal hemianopia. | |||
===Electrocardiogram=== | |||
*There are no ECG findings associated with bitemporal hemianopia. | |||
===X-ray=== | |||
*There are no x-ray findings associated with bitemporal hemianopia. | |||
===Echocardiography or Ultrasound=== | |||
*There are no echocardiography/ultrasound findings associated with bitemporal hemianopia. | |||
*However, [[B-scan ultrasonography|B-scan]] [[ultrasonography]] may be helpful in the diagnosis of bitemporal hemianopia when etiology is Nasal staphylomata.<ref name="GuptaSmith2015" /> | |||
===CT scan=== | |||
*Brain CT scan showing a mass near optic chiasm may be helpful in the identifying underlying cause of bitemporal hemianopia. | |||
*Calcifications can be seen in craniopharyngiomas.<ref name="pmid9204320">{{cite journal| author=Tsuda M, Takahashi S, Higano S, Kurihara N, Ikeda H, Sakamoto K| title=CT and MR imaging of craniopharyngioma. | journal=Eur Radiol | year= 1997 | volume= 7 | issue= 4 | pages= 464-9 | pmid=9204320 | doi=10.1007/s003300050184 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9204320 }}</ref> | |||
*Menigiomas are moderately hyperdense before contrast enhancement and have no or minimal calcification.<ref name="pmid6805276">{{cite journal| author=New PF, Hesselink JR, O'Carroll CP, Kleinman GM| title=Malignant meningiomas: CT and histologic criteria, including a new CT sign. | journal=AJNR Am J Neuroradiol | year= 1982 | volume= 3 | issue= 3 | pages= 267-76 | pmid=6805276 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6805276 }}</ref> | |||
===MRI=== | |||
*Brain MRI showing a mass near optic chiasm may be helpful in the identifying underlying cause of bitemporal hemianopia. Compression of optic chiasm by tumor can be graded from 0-4.<ref name="pmid12439668" /> | |||
*Extent and the relation of [[craniopharyngioma]] to other structures can be clearly seen in MRI than CT scan.<ref name="pmid9204320" /> | |||
==Treatment== | |||
===Medical Therapy=== | |||
*Even though there is decrease in [[Vision|peripheral vision]] in bitemporal heminaopia, a central [[visual field]] of 110°–120° is preserved, which is even acceptable for driving licensing.<ref name="pmid16986090">{{cite journal| author=Krzizok T, Schwerdtfeger G| title=[Bitemporal hemianopia in road traffic]. | journal=Klin Monbl Augenheilkd | year= 2006 | volume= 223 | issue= 9 | pages= 775-9 | pmid=16986090 | doi=10.1055/s-2006-926999 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16986090 }}</ref><ref name="pmid24588535" /> | |||
*Hence, asymptomatic or mildly symptomatic patients and those who aren't suitable candidates for [[surgery]] can be treated medically [[cabergoline]] for [[prolactinoma]], [[somatostatin|somatostatin analogues]] for [[acromegaly]] and can be followed up regularly.<ref name="pmid25446388">{{cite journal| author=Oki Y| title=Medical management of functioning pituitary adenoma: an update. | journal=Neurol Med Chir (Tokyo) | year= 2014 | volume= 54 | issue= 12 | pages= 958-65 | pmid=25446388 | doi= | pmc=4533360 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25446388 }}</ref> | |||
===Radiation Therapy=== | |||
*[[Radiation therapy]] can be used as an adjuvant to medical therapy and surgical therapy to prevent remission. | |||
*Gamma-knife therapy has seen a recent success in normalizing hormonal hypersecretion in patients who are not suitable candidates for surgery. A 90.3% tumor control had been achieved in microdenomas.<ref name="pmid10207688">{{cite journal| author=Jackson IM, Norén G| title=Role of gamma knife therapy in the management of pituitary tumors. | journal=Endocrinol Metab Clin North Am | year= 1999 | volume= 28 | issue= 1 | pages= 133-42 | pmid=10207688 | doi=10.1016/s0889-8529(05)70060-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10207688 }}</ref><ref name="pmid20540596">{{cite journal| author=Sheehan JP, Pouratian N, Steiner L, Laws ER, Vance ML| title=Gamma Knife surgery for pituitary adenomas: factors related to radiological and endocrine outcomes. | journal=J Neurosurg | year= 2011 | volume= 114 | issue= 2 | pages= 303-9 | pmid=20540596 | doi=10.3171/2010.5.JNS091635 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20540596 }}</ref> | |||
*[[Stereotactic surgery|Stereotactic radiosurgery]] is being considered in the treatment of [[Parasellar and suprasellar disorders|parasellar]] [[Meningioma|meningiomas]].<ref name="pmid28338439">{{cite journal| author=Cohen-Inbar O, Tata A, Moosa S, Lee CC, Sheehan JP| title=Stereotactic radiosurgery in the treatment of parasellar meningiomas: long-term volumetric evaluation. | journal=J Neurosurg | year= 2018 | volume= 128 | issue= 2 | pages= 362-372 | pmid=28338439 | doi=10.3171/2016.11.JNS161402 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28338439 }}</ref> | |||
===Surgery=== | |||
*Surgery is the mainstay of treatment for bitemporal hemianopia. | |||
*'''Pituitary adenoma''': | |||
**Transsphenoidal pituitary surgery is the first line surgery for pituitary adenomas. Visual improvement occurs in 87% of those with preoperative visual loss. It has a mortality rate of 0.5%.<ref name="urlSurgical Treatment of Pituitary Adenomas - Endotext - NCBI Bookshelf">{{cite web |url=https://www.ncbi.nlm.nih.gov/books/NBK278983/ |title=Surgical Treatment of Pituitary Adenomas - Endotext - NCBI Bookshelf |format= |work= |accessdate=}}</ref> | |||
**A meta-analysis of [[Endoscopic surgery|endoscopic]] vs microscopic surgery hasn't been statistically significant but endoscopic route has been attributed to increased vascular complications.<ref name="pmid23243265">{{cite journal| author=Ammirati M, Wei L, Ciric I| title=Short-term outcome of endoscopic versus microscopic pituitary adenoma surgery: a systematic review and meta-analysis. | journal=J Neurol Neurosurg Psychiatry | year= 2013 | volume= 84 | issue= 8 | pages= 843-9 | pmid=23243265 | doi=10.1136/jnnp-2012-303194 | pmc=3717601 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23243265 }}</ref> | |||
*'''Meningioma:''' | |||
**A [[Frontal|fronto]]-[[Orbital cavity|orbital]] approach for tumor excision is preferred. Visual defect has been resolved post-operatively.<ref name="pmid11950417" /> | |||
===Primary Prevention=== | |||
*There are no established measures for the primary prevention of bitemporal hemianopia. | |||
===Secondary Prevention=== | |||
*There are no established measures for the secondary prevention of bitemporal hemianopia. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category: Ophthalmology]] | |||
[[Category: Neurology]] | |||
[[Category: Physical examination]] | |||
[[Category: Eye pathology]] | |||
[[Category: Needs review]] | |||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
Latest revision as of 18:23, 27 September 2021
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-In-Chief: Aditya Govindavarjhulla, M.B.B.S. [2] Nihas Raja Mateti, M.B.B.S.[3]
Synonyms and keywords: Bitemporal hemianopsia
Overview
Bitemporal hemianopia (bi-: both eyes, temporal: temporal/peripheral, hemi-: half, anopsia: blindness) is defect in visual pathway causing loss of sight in the outer half of the visual field. A lesion compressing or disrupting optic chiasm would result in bitemporal hemianopia. Additional symptoms such as Headache, Diplopia, Endocrine disorders can be present. Most common causes are Pituitary macroadenoma, Craniopharyngioma, Meningioma and Aneurysm of anterior communicating artery. Visual field defects can be diagnosed using Standard Automated Perimetry (SAP). CT Imaging and MRI usually reveal the underlying cause. While vision loss can be improved by treating the underlying cause, sometimes it can be permanent.
Historical Perspective
- First case of Bitemporal hemianopsia was reported by Clarence A. Veasey, in 1904 [1].
- In 1929, L.S.Kubie and J.W.Beckmann documented Diplopia to be the most reported symptom in patients with bitemporal hemianopia in the absence of extraocular muscle palsies.[2]
Classification
- Bitemporal hemianopia may be classified according to the number of defective optic fibers into complete bitemporal hemianopia and partial bitemporal hemianopia.
Pathophysiology
- Bitemporal hemianopia is a visual defect due to a lesion involving optic chiasm.
- While afferent sensory inputs from superior temporal quadrant of visual field are relayed through inferior nasal fibers of optic nerve, the inputs from inferior temporal quadrant are relayed through superior nasal fibers. Similarly the visual information from superior nasal quadrant and inferior nasal quadrant are relayed through inferior temporal fibers and superior temporal fibers respectively.[3]
- Optic chiasm is an anatomical structure in middle cranial fossa formed by decussation of nasal fibers of optic nerve travelling from retina to visual cortex.
- A lesion involving optic chiasm either due to compression or vascular compromise, disrupts nasal fibers of optic nerve almost always resulting in bilateral defects in temporal half of visual field.[4][5]
- Nasal fibers have predilection for greater pressure due to compression causing them to be easily disrupted(Mechanical theory).[6]
- A lesion compressing the chiasm from below (eg: pituitary tumors) will have predominant defects in superior temporal quadrants along with partial defects in the inferior temporal quadrant and Vice-versa.
Causes
Common Causes
Most of the common causes of bitemporal hemianopia are due to disorders of the pituitary gland and its surrounding structures.
- Pituitary macroadenoma[7]
- Craniopharyngioma[8]
- Meningioma[9]
- Aneurysm of anterior communicating artery[10][10][10][10][10][10][10][10][10][10][10][10][10][10][10][10][10]
Causes by Organ System
Differentiating Bitemporal hemianopia from other Diseases
- Bitemporal hemiaopia must be differentiated from most common causes: pituitary adenoma, suprasellar tumors craniopharyngioma, aneurysm of anterior communicating artery and meningioma.
Differential diagnosis of Bitemporal hemianopia
| Pituitary adenoma | Functional adenoma - Endocrine abnormalities, Non functional adenoma - exert pressure symptoms (Headache). Isointense on MRI. |
| Suprasellar tumors Craniopharyngioma | Headache, Seizure, Focal neurological deficit. Calcified mass with Motor oil like fluid within the tumor on MRI. |
| Aneurysm of anterior communicating artery | Unruptured aneurysm can be asymptomatic or mild headache. Ruptured aneurysms presents with 'Worst headache of life' (Subarachnoid hemorrhage), Seizures, Focal neurological deficit. |
| Meningioma | Headache, Seizure, Focal neurological deficit. Well circumscribed, Extra-axial mass with Dural attachment on MRI. Psammoma bodies on immunohistopathology. |
Epidemiology and Demographics
- The prevalence of pituitary adenoma is approximately 16.7% worldwide. Pituitary adenomas are almost always associated with bitemporal hemianopia.[25]
- There is no racial predilection to bitemporal hemianopia.
Risk Factors
- There are no established risk factors for bitemporal hemianopia.
Screening
- There is insufficient evidence to recommend routine screening for bitemporal hemianopia in a normal population.
- Patients with asymptomatic pituitary adenomas can be screened by automated perimetry.
- Presence of Vertical step [SN-96% SP-100%] and Temporal depression[SN-100% and SP-98%] is the criteria for diagnosis of bitemporal hemianopia. [26]
Natural History, Complications, and Prognosis
Natural History
- In most of the patients, central visual field of 110°–120° (using Goldmann perimetry) is preserved and is sufficient for day to day activities. A volume perimetry demonstrates a binocular scotoma beyond the point of fixation.[27]
Complications
- Shearing of nasal fibers (as in traumatic chiasmal syndrome) most commonly resulted in permanent visual loss and rare improvement.[28][29]
Prognosis
- In patients with underlying etiology of pituitary adenomas, an improvement or complete recovery of visual acuity or visual field post-surgery has been seen in 70-75% of cases.[30][31][32][33][34]
Diagnosis
Diagnostic Study of Choice
- The diagnosis study of choice for bitemporal hemianopia is visual field testing.
- Visual field testing by Standard Automated Perimetry(SAP) with favorable sensitivity and early detection is preferred over Goldmann perimetry and is most common method used.[35]
- Even though frequency doubling technolgy (FDT) perimetry has increased sensitivity over SAP, it cannot categorize visual field defects.[36]
History and Symptoms
- The hallmark of bitemporal hemianopia is the loss of peripheral vision. It is usually an incidental finding as there is no loss in central vision.
- Presence of additional symptoms such as headache, diplopia, endocrine disorders point towards underlying etiology.
- History of chloroquine and ethambutol usage can be present.
Physical Examination
- Physical examination of patients with bitemporal hemianopia is usually normal.
Laboratory Findings
- There are no diagnostic laboratory findings associated with bitemporal hemianopia.
Electrocardiogram
- There are no ECG findings associated with bitemporal hemianopia.
X-ray
- There are no x-ray findings associated with bitemporal hemianopia.
Echocardiography or Ultrasound
- There are no echocardiography/ultrasound findings associated with bitemporal hemianopia.
- However, B-scan ultrasonography may be helpful in the diagnosis of bitemporal hemianopia when etiology is Nasal staphylomata.[23]
CT scan
- Brain CT scan showing a mass near optic chiasm may be helpful in the identifying underlying cause of bitemporal hemianopia.
- Calcifications can be seen in craniopharyngiomas.[37]
- Menigiomas are moderately hyperdense before contrast enhancement and have no or minimal calcification.[38]
MRI
- Brain MRI showing a mass near optic chiasm may be helpful in the identifying underlying cause of bitemporal hemianopia. Compression of optic chiasm by tumor can be graded from 0-4.[26]
- Extent and the relation of craniopharyngioma to other structures can be clearly seen in MRI than CT scan.[37]
Treatment
Medical Therapy
- Even though there is decrease in peripheral vision in bitemporal heminaopia, a central visual field of 110°–120° is preserved, which is even acceptable for driving licensing.[39][27]
- Hence, asymptomatic or mildly symptomatic patients and those who aren't suitable candidates for surgery can be treated medically cabergoline for prolactinoma, somatostatin analogues for acromegaly and can be followed up regularly.[40]
Radiation Therapy
- Radiation therapy can be used as an adjuvant to medical therapy and surgical therapy to prevent remission.
- Gamma-knife therapy has seen a recent success in normalizing hormonal hypersecretion in patients who are not suitable candidates for surgery. A 90.3% tumor control had been achieved in microdenomas.[41][42]
- Stereotactic radiosurgery is being considered in the treatment of parasellar meningiomas.[43]
Surgery
- Surgery is the mainstay of treatment for bitemporal hemianopia.
- Pituitary adenoma:
- Transsphenoidal pituitary surgery is the first line surgery for pituitary adenomas. Visual improvement occurs in 87% of those with preoperative visual loss. It has a mortality rate of 0.5%.[44]
- A meta-analysis of endoscopic vs microscopic surgery hasn't been statistically significant but endoscopic route has been attributed to increased vascular complications.[45]
- Meningioma:
Primary Prevention
- There are no established measures for the primary prevention of bitemporal hemianopia.
Secondary Prevention
- There are no established measures for the secondary prevention of bitemporal hemianopia.
References
- ↑ Veasey CA (1904). "Observations of a case of bi-temporal hemianopsia with some unusual changes in the visual fields". Trans Am Ophthalmol Soc. 10 (Pt 2): 383–7. PMC 1322445. PMID 16692037.
- ↑ Kubie, L. S.; Beckmann, J. W. (1929). "DIPLOPIA WITHOUT EXTRA-OCULAR PALSIES, CAUSED BY HETERONYMOUS DEFECTS IN THE VISUAL FIELDS ASSOCIATED WITH DEFECTIVE MACULAR VISION". Brain. 52 (3): 317–333. doi:10.1093/brain/52.3.317. ISSN 0006-8950.
- ↑ "The Retinotopic Representation of the Visual Field - Neuroscience - NCBI Bookshelf".
- ↑ Hedges TR (1969). "Preservation of the upper nasal field in the chiasmal syndrome: an anatomic explanation". Trans Am Ophthalmol Soc. 67: 131–41. PMC 1310336. PMID 5381296.
- ↑ Bergland R (1969). "The arterial supply of the human optic chiasm". J Neurosurg. 31 (3): 327–34. doi:10.3171/jns.1969.31.3.0327. PMID 5811834.
- ↑ McIlwaine GG, Carrim ZI, Lueck CJ, Chrisp TM (2005). "A mechanical theory to account for bitemporal hemianopia from chiasmal compression". J Neuroophthalmol. 25 (1): 40–3. doi:10.1097/00041327-200503000-00011. PMID 15756133.
- ↑ Lake MG, Krook LS, Cruz SV (2013). "Pituitary adenomas: an overview". Am Fam Physician. 88 (5): 319–27. PMID 24010395.
- ↑ Müller HL (2014). "Craniopharyngioma". Endocr Rev. 35 (3): 513–43. doi:10.1210/er.2013-1115. PMID 24467716.
- ↑ 9.0 9.1 Bejjani GK, Cockerham KP, Kennerdell JS, Maroon JC (2002). "Visual field deficit caused by vascular compression from a suprasellar meningioma: case report". Neurosurgery. 50 (5): 1129–31, discussion 1131-2. doi:10.1097/00006123-200205000-00033. PMID 11950417.
- ↑ Seung WB, Kim DY, Park YS (2015). "A Large Ruptured Anterior Communicating Artery Aneurysm Presenting with Bitemporal Hemianopsia". J Korean Neurosurg Soc. 58 (3): 291–3. doi:10.3340/jkns.2015.58.3.291. PMC 4630364. PMID 26539276.
- ↑ Fay A, Lee LC, Pasquale LR (2003). "Dermatochalasis causing apparent bitemporal hemianopsia". Ophthalmic Plast Reconstr Surg. 19 (2): 151–3. doi:10.1097/01.IOP.0000055827.78632.CA. PMID 12644764.
- ↑ Goldhammer, Y.; Smith, J. L. (1974). "Bitemporal hemianopia in chloroquine retinopathy". Neurology. 24 (12): 1135–1135. doi:10.1212/WNL.24.12.1135. ISSN 0028-3878.
- ↑ 13.0 13.1 Boulanger Scemama E, Touitou V, Le Hoang P (2013). "[Bitemporal hemianopia as presenting sign of severe ethambutol toxicity]". J Fr Ophtalmol. 36 (9): e163–7. doi:10.1016/j.jfo.2012.12.008. PMID 24094504.
- ↑ Osher, R. H.; Corbett, J. J.; Schatz, N. J.; Savino, P. J.; Orr, L. S. (1978). "Neuro-ophthalmological complications of enlargement of the third ventricle". British Journal of Ophthalmology. 62 (8): 536–542. doi:10.1136/bjo.62.8.536. ISSN 0007-1161.
- ↑ Thavaratnam LK, Loy ST, Gupta A, Ng I, Cullen JF (2015). "Chordoid glioma". Singapore Med J. 56 (11): 641–3. doi:10.11622/smedj.2015175. PMC 4656874. PMID 26668411.
- ↑ GIBBS DC (1959). "Chiasmal arachnoiditis". Br J Ophthalmol. 43 (1): 52–6. doi:10.1136/bjo.43.1.52. PMC 512211. PMID 13618533.
- ↑ 17.0 17.1 Lodge WO (1946). "BITEMPORAL HEMIANOPIA". Br J Ophthalmol. 30 (5): 276–81. PMC 510604. PMID 18170220.
- ↑ Yazici, Bulent (2015). "Isolated Bitemporal Hemianopsia Due to Traumatic Chiasmal Syndrome". Turkish Journal of Trauma and Emergency Surgery. doi:10.5505/tjtes.2015.90540. ISSN 1306-696X.
- ↑ Slavin ML (1990). "Bitemporal hemianopia associated with dolichoectasia of the intracranial carotid arteries". J Clin Neuroophthalmol. 10 (1): 80–1. PMID 2139057.
- ↑ PEARCE HM (1963). "PHYSIOLOGIC BITEMPORAL HEMIANOPSIA IN PREGNANCY". Obstet Gynecol. 22: 612–4. PMID 14082282.
- ↑ Levine BM, Lelli GJ (2010). "Bitemporal hemianopia caused by bilateral blepharoptosis". Orbit. 29 (6): 351–3. doi:10.3109/01676830.2010.516467. PMID 21158577.
- ↑ "Bitemporal Hemianopia Caused by Retinal Disease". Archives of Ophthalmology. 127 (12): 1686. 2009. doi:10.1001/archophthalmol.2009.320. ISSN 0003-9950.
- ↑ 23.0 23.1 Gupta, Anjali; Smith, J. M. Alaric (2015). "Bitemporal Hemianopia Secondary to Nasal Staphylomata". Journal of Neuro-Ophthalmology. 35 (1): 99–101. doi:10.1097/WNO.0000000000000202. ISSN 1070-8022.
- ↑ Manfrè L, Vero S, Focarelli-Barone C, Lagalla R (1999). "Bitemporal pseudohemianopia related to the "tilted disk" syndrome: CT, MR, and fundoscopic findings". AJNR Am J Neuroradiol. 20 (9): 1750–1. PMC 7056191 Check
|pmc=value (help). PMID 10543654. - ↑ Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML; et al. (2004). "The prevalence of pituitary adenomas: a systematic review". Cancer. 101 (3): 613–9. doi:10.1002/cncr.20412. PMID 15274075.
- ↑ 26.0 26.1 Fujimoto N, Saeki N, Miyauchi O, Adachi-Usami E (2002). "Criteria for early detection of temporal hemianopia in asymptomatic pituitary tumor". Eye (Lond). 16 (6): 731–8. doi:10.1038/sj.eye.6700165. PMID 12439668.
- ↑ 27.0 27.1 Peli E, Satgunam P (2014). "Bitemporal hemianopia; its unique binocular complexities and a novel remedy". Ophthalmic Physiol Opt. 34 (2): 233–42. doi:10.1111/opo.12118. PMC 3947624. PMID 24588535.
- ↑ Bansal, Shveta; Kumar, Nishant; Kyle, Graham (2006). "Mechanism of Bitemporal Hemianopia". Journal of Neuro-Ophthalmology. 26 (3): 233. doi:10.1097/01.wno.0000235584.87674.9d. ISSN 1070-8022.
- ↑ Vellayan Mookan L, Thomas PA, Harwani AA (2018). "Traumatic chiasmal syndrome: A meta-analysis". Am J Ophthalmol Case Rep. 9: 119–123. doi:10.1016/j.ajoc.2018.01.029. PMC 5861742. PMID 29577103.
- ↑ "Internet Scientific Publications".
- ↑ Berkmann, S; Fandino, J; Müller, B; Kothbauer, KF; Henzen, C; Landolt, H (2013). "Reply to the letter to the Editor "Visual outcomes after pituitary surgery"". Swiss Medical Weekly. doi:10.4414/smw.2013.13803. ISSN 1424-7860.
- ↑ Lampropoulos KI, Samonis G, Nomikos P (2013). "Factors influencing the outcome of microsurgical transsphenoidal surgery for pituitary adenomas: a study on 184 patients". Hormones (Athens). 12 (2): 254–64. doi:10.14310/horm.2002.1409. PMID 23933694.
- ↑ Mortini P, Losa M, Barzaghi R, Boari N, Giovanelli M (2005). "Results of transsphenoidal surgery in a large series of patients with pituitary adenoma". Neurosurgery. 56 (6): 1222–33, discussion 1233. doi:10.1227/01.neu.0000159647.64275.9d. PMID 15918938.
- ↑ Tagoe NN, Essuman VA, Bankah P, Dakurah T, Hewlett VK, Akpalu J; et al. (2019). "Visual Outcome of Patients with Pituitary Adenomas Following Surgery and Its Contributory Factors at a Tertiary Hospital in Ghana". Ethiop J Health Sci. 29 (1): 895–902. doi:10.4314/ejhs.v29i1.11. PMC 6341437. PMID 30700957.
- ↑ Katz J, Tielsch JM, Quigley HA, Sommer A (1995). "Automated perimetry detects visual field loss before manual Goldmann perimetry". Ophthalmology. 102 (1): 21–6. doi:10.1016/s0161-6420(95)31060-3. PMID 7831036.
- ↑ Monteiro, Mário Luiz Ribeiro; Moura, Frederico Castelo; Cunha, Leonardo Provetti (2007). "Frequency doubling perimetry in patients with mild and moderate pituitary tumor-associated visual field defects detected by conventional perimetry". Arquivos Brasileiros de Oftalmologia. 70 (2): 323–329. doi:10.1590/S0004-27492007000200024. ISSN 0004-2749.
- ↑ 37.0 37.1 Tsuda M, Takahashi S, Higano S, Kurihara N, Ikeda H, Sakamoto K (1997). "CT and MR imaging of craniopharyngioma". Eur Radiol. 7 (4): 464–9. doi:10.1007/s003300050184. PMID 9204320.
- ↑ New PF, Hesselink JR, O'Carroll CP, Kleinman GM (1982). "Malignant meningiomas: CT and histologic criteria, including a new CT sign". AJNR Am J Neuroradiol. 3 (3): 267–76. PMID 6805276.
- ↑ Krzizok T, Schwerdtfeger G (2006). "[Bitemporal hemianopia in road traffic]". Klin Monbl Augenheilkd. 223 (9): 775–9. doi:10.1055/s-2006-926999. PMID 16986090.
- ↑ Oki Y (2014). "Medical management of functioning pituitary adenoma: an update". Neurol Med Chir (Tokyo). 54 (12): 958–65. PMC 4533360. PMID 25446388.
- ↑ Jackson IM, Norén G (1999). "Role of gamma knife therapy in the management of pituitary tumors". Endocrinol Metab Clin North Am. 28 (1): 133–42. doi:10.1016/s0889-8529(05)70060-8. PMID 10207688.
- ↑ Sheehan JP, Pouratian N, Steiner L, Laws ER, Vance ML (2011). "Gamma Knife surgery for pituitary adenomas: factors related to radiological and endocrine outcomes". J Neurosurg. 114 (2): 303–9. doi:10.3171/2010.5.JNS091635. PMID 20540596.
- ↑ Cohen-Inbar O, Tata A, Moosa S, Lee CC, Sheehan JP (2018). "Stereotactic radiosurgery in the treatment of parasellar meningiomas: long-term volumetric evaluation". J Neurosurg. 128 (2): 362–372. doi:10.3171/2016.11.JNS161402. PMID 28338439.
- ↑ "Surgical Treatment of Pituitary Adenomas - Endotext - NCBI Bookshelf".
- ↑ Ammirati M, Wei L, Ciric I (2013). "Short-term outcome of endoscopic versus microscopic pituitary adenoma surgery: a systematic review and meta-analysis". J Neurol Neurosurg Psychiatry. 84 (8): 843–9. doi:10.1136/jnnp-2012-303194. PMC 3717601. PMID 23243265.