Sandbox 2: Difference between revisions
Aditya Ganti (talk | contribs) No edit summary |
Aditya Ganti (talk | contribs) |
||
| (127 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
Lower GI bleeding is defined as any bleed that occurs distal to the ligament of Treitz. | |||
==Incidence== | |||
*In the United States the incidence of LGIB ranges from 20.5 to 27 per 100,000 persons per year. | |||
==Age== | |||
*There is a greater than 200 fold increase from the third to the ninth decade of life. | |||
==Classification== | |||
== | *Lower GI bleeding can be classified into 3 groups based on the severity of bleeding: | ||
**Occult lower GI bleeding | |||
* | **Moderate lower GI bleeding | ||
**Severe lower GI bleeding | |||
* | |||
== | |||
* | |||
* | |||
* | |||
* | |||
* | |||
* | |||
* | |||
{| class="wikitable" | |||
! | |||
!Severe lower GI bleeding | |||
!Moderate lower GI bleeding | |||
!Occult lower GI bleeding | |||
|- | |||
|Age | |||
|> 65 years | |||
|Occur at any age | |||
|Any age | |||
|- | |||
|Presenting symptoms | |||
|Hematochezia or bright red blood per rectum. | |||
|Hematochezia or melena. | |||
|Symptoms of anemia (fatigue, tirdness) | |||
|- | |||
|Hemodynamics | |||
|Unstable | |||
|Stable | |||
|Stable | |||
|- | |||
|Lab findings | |||
|hemoglobin equal to or less than 6 g/dl. | |||
|Microcytic anemia | |||
|Microcytic hypochromic anemia due to chronic blood loss. | |||
|- | |||
|Differential | |||
|Diverticulosis and angiodysplasias | |||
|Neoplastic disease Inflammatory, <nowiki><br></nowiki> infectious, benign anorectal, and congenital diseases. | |||
|Inflammatory, neoplastic and congenital. | |||
|} | |||
==Blood supply== | |||
* The SMA and IMA are connected by the marginal artery of Drummond. | |||
* This vascular arcade runs in the mesentery close to the bowel. | |||
* As patients age, there is increased incidence of occlusion of the IMA. | |||
* The left colon stays perfused, primarily because of the marginal artery. | |||
{| border="1" cellpadding="5" cellspacing="0" align="center" |class="wikitable" | |||
! colspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" |Lower GI Tract | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" | Arterial Supply | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" |Venous Drainage | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Midgut | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Distal duodenum jejunum | |||
* Ileum | |||
* Appendix | |||
* Cecum | |||
* Ascending colon | |||
* Hepatic flexure | |||
* Proximal transverse colon. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Superior mesenteric artery (SMA) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Portal system. | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Hindgut | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Distal one-third of the transverse colon | |||
* Splenic flexure | |||
* Descending colon, | |||
* Sigmoid colon | |||
* Rectumhu | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Inferior mesenteric artery (IMA) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Portal system '''<sup>ɸ</sup>''' | |||
|- | |||
| colspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="center" |ɸ -Except lower rectum, which drains into the systemic circulation. | |||
|} | |||
[[Image: Colonic blood supply1.gif|thumb|center|300px|Blood supply to the intestines includes the celiac artery, superior mesenteric artery (SMA), inferior mesenteric artery (IMA), and branches of the internal iliac artery (IIA). <br>Source: By Anpol42 (Own work) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons]] | |||
===Pathogenesis=== | |||
Diverticulosis is the most common etiology of lower GI bleeding accounting for 30% of all cases, followed by anorectal disease, ischemia, inflammatory bowel disease (IBD), neoplasia and arteriovenous (AV) malformations. | |||
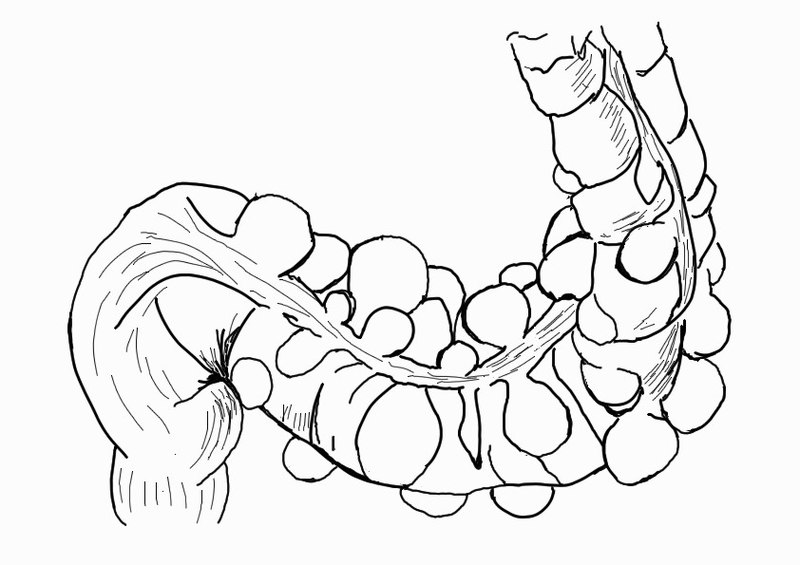
*'''<u>Diverticulosis</u>''' | |||
**The colonic wall weakens with age and results in the formation of saclike protrusions known as diverticula. | |||
**These protrusions generally occur at the junction of blood vessel penetrating through the mucosa and circular muscle fibers of the colon. | |||
**Diverticula are most common in the descending and sigmoid colon. | |||
**Despite the majority of diverticula being on the left side of the colon, diverticular bleeding originates from the right side of the colon in 50% to 90% of instances. | |||
**Most of the time bleeding from diverticulosis stops spontaneously, however, in about 5% of patients, the bleeding can be massive and life-threatening. | |||
[[Image:Sigmoid diverticulum (diagram).jpg|thumb|center|400px|Diagram of sigmoid diverticulum<br>Source:By Anpol42 (Own work) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons]] | |||
*'''<u>Anorectal disease</u>''' | |||
:*Hemorrhoids and anal fissures are the most common disease under anorectal disease responsible for GI bleeding. | |||
:*Hemorrhoids are engorged vessels in the normal anal cushions. When swollen, this tissue is very friable and susceptible to trauma, which leads to painless, bright red bleeding. | |||
:*Anal fissures are defined as a tear in the anal mucosa. With the passage of stool, the mucosa continues to tear and leads to bright red bleeding. | |||
*'''<u>Mesenteric Ischemia</u>''' | |||
:*Mesenteric ischemia results when there is inadequate blood supply at the level of the small intestine. | |||
:*2 or more vessels (celiac, SMA, or IMA) must be involved for symptoms to occur. | |||
:*Non occlusive mesenetric ischemia affects critically ill patients who are vasopressor-dependent. | |||
:*Venous thrombosis of the visceral vessels can also precipitate an acute ischemic event. | |||
*'''<u>Ischemic Colitis</u>''' | |||
:*Ischemic colitis is caused by poor perfusion of the colon, which results in the inability of that area of the colon to meet its metabolic demands. | |||
:*It can be gangrenous or nongangrenous, acute, transient, or chronic. | |||
:*The left colon is predominantly affected, with the splenic flexure having increased susceptibility. | |||
:*Intraluminal hemorrhage occurs as the mucosa becomes necrotic, sloughs, and bleeds. | |||
:*Damage to the tissue is caused both with the ischemic insult as well as reperfusion injury. | |||
*'''<u>Inflammatory Bowel Disease</u>''' | |||
:*In Crohn's disease T cell activation stimulates interleukin (IL)-12 and tumor necrosis factor (TNF)-a, which causes chronic inflammation and tissue injury. | |||
:*Initially, inflammation starts focally around the crypts, followed by superficial ulceration of the mucosa. | |||
:*The deep mucosal layers are then invaded in a noncontinuous fashion, and noncaseating granulomas form, which can invade through the entire thickness of the bowel and into the mesentery and surrounding structures. | |||
:*In ulcerative colitis T cells cytotoxic to the colonic epithelium accumulate in the lamina propria, accompanied by B cells that secrete immunoglobulin G (IgG) and IgE. | |||
:*This results in inflammation of the crypts of Lieberkuhn, with abscesses and pseudopolyps. | |||
:*Ulcerative colitis generally begins at the rectum and is a continuous process confined exclusively to the colon. | |||
*'''<u>Neoplasia</u>''' | |||
:*Colon carcinoma follows a distinct progression from polyp to cancer. | |||
:*Mutations of multiple genes are required for the formation of adenocarcinoma, including the APC gene, Kras, DCC, and p53. | |||
:*Certain hereditary syndromes are also classified by defects in DNA mismatch repair genes and microsatellite instability. | |||
:*These tumors tend to bleed slowly, and patients present with hemocult positive stools and microcytic anemia. | |||
:*Although cancers of the small bowel are much less common than colorectal cancers, they should be ruled out in cases of lower GI bleeding in which no other source is identified. | |||
*'''<u>AV Malformation/Angiodysplasia</u>''' | |||
:*In AV malformation direct connections between arteries and veins occur in the colonic submucosa. | |||
:*The lack of capillary buffers causes high pressure blood to enter directly into the venous system, making these vessels at high risk of rupture into the bowel lumen. | |||
:*In Angiodysplasia over time, previously healthy blood vessels of the cecum and ascending colon degenerate and become prone to bleeding. | |||
:*Although 75% of angiodysplasia cases involve the right colon, they are a significant cause of obscure bleeding and the most common cause of bleeding from the small bowel in the elderly. | |||
==Epidemiology== | |||
===Prevalence=== | |||
*Approximately 20 patients/100,000 population in the U.S. | |||
===Incidence=== | |||
*The estimated annual incidence of lower GI bleeding is approximately 0.03% in the adult population as a whole. | |||
==Demographics== | |||
===Gender=== | |||
*More common in men than women | |||
===Age=== | |||
*Rare in children | |||
*The incidence of lower GI bleeding increases with age with a 200-fold increase from the second to eighth decades of life la. | |||
**Largely due to the increase in the prevalence of diverticular disease and angiodysplasia with age. | |||
==Symptoms== | |||
*Occult LGIB may present with symptoms of iron deficiency anemia such as fatigue, palpitations, and dyspnea. | |||
*Patients with intussusception may present with pallor and vomiting in addition to LGIB | |||
*Associated symptoms, such as abdominal pain or change in bowel habits, may also aide in the diagnosis | |||
*Bloody diarrhea associated with abdominal pain may suggest an infectious cause or IBD in a younger patient and ischemic colitis in an older patient with vascular disease | |||
*Painless bleeding usually suggests angiodysplasia, diverticular disease, or internal hemorrhoids | |||
*Perianal pain suggests a perianal fissure or fistula | |||
==History== | |||
*A detailed description of the nature of the blood loss can help in pinpointing the likely source of bleeding. | |||
===Past Medical History=== | |||
*The clinical history should identify whether this is a recurrent bleed. | |||
*Bleeding from angiodysplasia is usually recurrent and chronic, but severe bleeding resulting in hemodynamic instability can occur. | |||
*Associated weight loss suggests malignancy. | |||
*The presence of systemic diseases such as atherosclerotic disease, IBD, coagulopathies, and HIV, and a history of pelvic irradiation for malignancy should be considered | |||
===Past Surgical History=== | |||
*A history of recent colonic polypectomy or biopsy indicates iatrogenic bleeding. | |||
**This is usually low grade and limited, although it can be severe if an underlying artery is involved or if there is an inadequate coagulation of the polypectomy stalk. | |||
**In 1.5% of polypectomies bleeding occurs immediately. However, delayed bleeding can occur several hours or days following the procedure | |||
*It is essential to establish the presence of comorbid diseases, as these not only help in diagnosis but may also influence treatment. | |||
===Family history=== | |||
*A family history of diseases such as IBD or colorectal malignancy is relevant. | |||
==Symptoms== | |||
*The clinical presentation of LGIB varies with the anatomic source of the bleeding. | |||
*Commonly, LGIB from the right side of the colon can manifest as maroon stools, whereas a left-sided bleeding source may be evidenced by bright red blood per rectum. | |||
*The presentation of LGIB can also vary depending on the etiology. | |||
**A young patient may present with fever, dehydration, abdominal cramps, and hematochezia caused by infectious or noninfectious (idiopathic) colitis. | |||
**An older patient may present with painless bleeding and minimal symptoms caused by diverticular bleeding or angiodysplasia. | |||
**LGIB can be mild and intermittent, as often is the case with angiodysplasia, or it may be moderate or severe, as may be the situation in diverticula-related bleeding. | |||
**Young patients may present with abdominal pain, rectal bleeding, diarrhea, and mucous discharge that may be associated with IBD. | |||
** Elderly patients presenting with abdominal pain, rectal bleeding, and diarrhea may have ischemic colitis. | |||
** Elderly patients with atherosclerotic heart disease may present with intermittent LGIB and syncope that may be due to angiodysplastic lesions. | |||
** Stools streaked with blood, perianal pain, and blood drops on the toilet paper or in the toilet bowl may be associated with perianal pathology, such as anal fissure or hemorrhoidal bleeding. | |||
** The passage of maroon stools or bright red blood from the rectum is usually indicative of massive lower GI hemorrhage. | |||
* Massive LGIB is a life-threatening condition in which patients present with a systolic blood pressure (SBP) of below 90 mm Hg and a hemoglobin (Hb) level of 6 g/dL or less. | |||
{| class="wikitable" | |||
! colspan="2" |Disease | |||
!Symptoms | |||
|- | |||
| colspan="2" |Diverticular bleeding | |||
|Painless bleeding | |||
Mild abdominal cramping | |||
If the bleeding is brisk and voluminous, patients may be hypotensive and display signs of shock | |||
|- | |||
| colspan="2" |Angiodysplasia | |||
|Painless, hematochezia or melena (slow but repeated bleeding episodes) | |||
Syncope | |||
|- | |||
| rowspan="4" |Colitis | |||
|Ischemic colitis | |||
| rowspan="4" |Fever | |||
Abdominal pain | |||
Bloody diarrhea | |||
Dehydration | |||
Hypotension in severe cases | |||
Weight loss | |||
|- | |||
|Infectious colitis | |||
|- | |||
|Radiation-induced colitis | |||
|- | |||
|Ulcerative colitis | |||
|- | |||
| colspan="2" |Colon cancer | |||
|Right-sided bleeding (Maroon stools or melena) | |||
Insidious | |||
Patients presents with iron-deficiency anemia and syncope | |||
== | Whereas left-sided colonic neoplasms can present as bright red blood per rectum | ||
|- | |||
* | | colspan="2" |Hemorrhoids | ||
* | |Painless, whereas bleeding secondary to fissures tends to be painful. | ||
Can also present with strangulation, hematochezia, and pruritus. | |||
|} | |||
===Common causes=== | |||
*Colonic diverticulosis | |||
**Colonic diverticulosisis the most common cause of acute LGIB in the western world, accounting for 15% to 55% of all LGIB | |||
**Diverticula can occur anywhere in the gastrointestinal tract, but are most common in the sigmoid colon. However, approximately 60% of diverticular bleeds arise from diverticula in the right colon, highlighting a tendency for right-sided diverticula to bleed | |||
**Hemorrhage results from rupture of the intramural branches (vasa recta) of the marginal artery at the dome of a diverticulum and can give rise to a massive, life-threatening LGIB | |||
**This is by far the most common cause of bleeding in the elderly, as the prevalence of diverticular disease increases with age, being as high as 85% by the age of 85 years | |||
* Obesity has recently been recognized as a risk factor in the development of diverticular disease, and the risk of diverticular bleeding in this group of patients is higher than that in patients who are not obese | |||
The | * Vascular ectasias (angiodysplasias/angioectasias): | ||
=== | ** Tortuous dilated submucosal vessels that account for approximately 10% of LGIB. | ||
* | ** They appear endoscopically as small, flat lesions (5-10 mm) with ectatic capillaries radiating from a central vessel (Fig. 1) | ||
* | ** The prevalence of angiodysplasia in the gastrointestinal tract is not well known, but a pooled analysis of three colonoscopic cancer screening studies detected angiodysplasia in 0.8% of the patients The prevalence of angiodysplasia is higher in older populations and, in the past, has been linked to certain conditions such as end-stage renal disease, Von Willebrand disease , and aortic stenosis In one series, 37% of colonic dysplasias were found in the cecum, 17% in the ascending colon, 7% in the transverse colon, 7% in the descending colon, and 32% in rectosigmoid area | ||
=== | ** Angiodysplasia can also be found throughout the small bowel and is responsible for up to 40% of small intestinal bleeding in patients older than 40 years. | ||
* | ** Angiodysplasia of the stomach and duodenum is responsible for up to 7% of UGIB I | ||
* | * Iatrogenic: | ||
* | ** Bleeding is recognized as the most common complication of colonoscopy and polypectomy, occurring in 0.3% to 6.1% of polypectomies | ||
** Risk factors for bleeding include polyp size greater than 1 cm, patient age older than 65 years, presence of comorbid disease, and polypectomy using the cutting mode of current | |||
** The risk is also greater in patients taking anticoagulant or antiplatelet agents | |||
* Ischemic colitis: | |||
** Ischemic colitis accounts for approximately 20% of LGIB | |||
** Ischemia results from a sudden reduction in blood flow to the mesenteric vessels as a result of hypotension, occlusion, or spasm of the mesenteric vessels | |||
** Nonocclusive disease typically affects the watershed areas of the bowels, such as the splenic flexure and adjacent transverse colon due to the poor blood supply from the marginal artery. | |||
** Occlusive disease is rarer but can occur as a result of thrombus formation or embolus. | |||
** It is a recognized complication of aortic surgery | |||
** Elderly patients with comorbid disease are at higher risk of developing ischemic colitis. | |||
** There may be a history of ischemic heart disease | |||
** The majority of patients with ischemic colitis improve following conservative management; however, approximately 20% will progress to develop colonic gangrene | |||
** Other complications include chronic colitis and stricture formation | |||
** Diagnosis requires a high index of suspicion | |||
* Colorectal malignancy: | |||
** Colorectal cancer accounts for approximately 10% of bleeds, either as occult bleeding presenting with anemia or as frank blood loss per rectum | |||
** A family history of colorectal cancer is important to establish | |||
* Anorectal abnormalities: | |||
** Hemorrhoids, fissures, fistulae, and polyps can all present with bright red rectal bleeding, which may be intermittent in nature | |||
** Hemorrhoids are the most common cause of rectal bleeding in adults younger than 50 years | |||
** The finding of hemorrhoids in older patients with LGIB should not preclude further investigation, as hemorrhoids are an extremely common finding and may not be the cause of bleeding | |||
* Inflammatory bowel disease (IBD): | |||
** IBD refers to both Crohn disease and ulcerative colitis Accounts for 5% to 10% of bleeds. | |||
** It is by far the most common cause of LGIB in Asian populations in whom the prevalence of diverticular disease is much lower | |||
** A previous history of IBD in patients with LGIB is important, as these patients have a higher risk of developing colorectal malignancy than do the general population | |||
* Infectious colitis: | |||
** The most common organisms in the U.S. are species ofSalmonella,Campylobacter,Shigella, andYersinia | |||
=== Rare causes === | |||
* Colonic polyps: | |||
** These can occur in isolation or as part of an inherited polyposis syndrome | |||
** Can cause occult or overt LGIB | |||
* Radiation proctitis: | |||
** This usually occurs a few months following ionizing radiation for pelvic malignancies (Fig. 2). In one study of patients with radiation proctitis following pelvic irradiation, 69% presented with bleeding within 1 year and 96% within 2 years | |||
* Rectal varices: | |||
** Associated with portal hypertension; may result in massive bleeding | |||
** Stercoral ulceration: | |||
** Can cause significant fresh rectal bleeding in elderly constipated patients | |||
* Meckel diverticulum: | |||
** These small bowel diverticula may contain ectopic gastric mucosa that can ulcerate and cause bleeding | |||
** They are the most common cause of massive LGIB in young children, and can be diagnosed with angiography, Meckel scans, and radionuclide imaging | |||
* Intussusception : | |||
** More common in children, with the highest incidence between the ages of 6 months and 2 years | |||
* Henoch-Schönlein purpura (HSP): | |||
** Most commonly affects children | |||
** Bleeding may be a direct result of vasculitis or secondary to intussusception, which is associated with HSP | |||
* Aortoenteric fistula: | |||
* Abdominal aortic aneurysms, especially those of the inflammatory type, may fistulate into the small bowel, giving rise to a massive, life-threatening hemorrhage | |||
* Peutz-Jeghers syndrome: | |||
** Polyps may give rise to frank or occult bleeding | |||
* Klippel-Trenaunay-Weber syndrome: | |||
** Hemangiomas in the colon can cause significant bleeding | |||
* Hereditary hemorrhagic telangiectasia: | |||
** Blood loss from mucosal telangiectasia can be chronic or acute | |||
* Neurofibromatosis : | |||
** Neurofibromas within the lumen of the bowel can ulcerate, causing bleeding | |||
* Blue rubber bleb syndrome: | |||
** Bleeding can arise from hemangiomas in the bowel Usually occult in nature | |||
** | |||
=== Risk factors === | |||
Common risk factors in the development of lower GI bleeding include:<ref name="pmid23997409">{{cite journal |vauthors=Navuluri R, Kang L, Patel J, Van Ha T |title=Acute lower gastrointestinal bleeding |journal=Semin Intervent Radiol |volume=29 |issue=3 |pages=178–86 |year=2012 |pmid=23997409 |pmc=3577586 |doi=10.1055/s-0032-1326926 |url=}}</ref><ref name="pmid16303575">{{cite journal |vauthors=Strate LL |title=Lower GI bleeding: epidemiology and diagnosis |journal=Gastroenterol. Clin. North Am. |volume=34 |issue=4 |pages=643–64 |year=2005 |pmid=16303575 |doi=10.1016/j.gtc.2005.08.007 |url=}}</ref><ref name="pmid17131153">{{cite journal |vauthors=Ríos A, Montoya MJ, Rodríguez JM, Serrano A, Molina J, Ramírez P, Parrilla P |title=Severe acute lower gastrointestinal bleeding: risk factors for morbidity and mortality |journal=Langenbecks Arch Surg |volume=392 |issue=2 |pages=165–71 |year=2007 |pmid=17131153 |doi=10.1007/s00423-006-0117-6 |url=}}</ref><ref name="pmid12695275">{{cite journal |vauthors=Strate LL, Orav EJ, Syngal S |title=Early predictors of severity in acute lower intestinal tract bleeding |journal=Arch. Intern. Med. |volume=163 |issue=7 |pages=838–43 |year=2003 |pmid=12695275 |doi=10.1001/archinte.163.7.838 |url=}}</ref> | |||
* Advancing age | |||
* Previous history of gastrointestinal bleed | |||
* Chronic constipation | |||
* Hematologic disorders | |||
* Anticoagulants medications | |||
* Nonsteroidal anti-inflammatory drugs | |||
* Human immunodeficiency virus | |||
{| class="wikitable" | |||
|Chronic constipation | |||
|Results in colonic diverticula and predispose patients to anal fissures and hemorrhoid formation | |||
|- | |||
|Hematologic disorders | |||
|Deficiencies in clotting factors, such as factor VII and factor VIII, predispose persons to LGIB | |||
|- | |||
|Anticoagulants medications | |||
|Patients taking warfarin and heparin, aspirin, and platelet inhibitors are at increased risk of bleeding in general | |||
|- | |||
|Nonsteroidal anti-inflammatory drugs | |||
|NSAIDs cause ulceration in the terminal ileum and proximal colon, and can exacerbate IBD | |||
|- | |||
|Human immunodeficiency virus | |||
|In patients with HIV, bleeding is caused by opportunistic infections, cytomegalovirus colitis, Kaposi sarcoma, or lymphoma | |||
|} | |||
==Management== | |||
===Initial Evaluation=== | |||
*In patients with acute lower gastrointestinal bleeding who are unstable rapid assessment and resuscitation should be initiated even before diagnostic evaluation. | |||
*The initial steps in the management of a patient with lower gastrointestinal bleeding are to assess the severity of bleeding, and then institute fluid and blood resuscitation as needed. | |||
*Once hemodynamic stability is achieved, nasogastric lavage should be performed to rule of upper GI source. | |||
*Equilibration between the intravascular and extravascular volumes cannot be achieved until 24 to 72 hours after bleeding has occurred. | |||
===Role of Nasogastric tube (NGT)=== | |||
*Nasogastric tube (NGT) lavage is recommended in all patients with lower gastrointestinal bleeding once the patient is stabilized. | |||
*A carefully placed nasogastric tube (NGT) with irrigation and aspiration of bile is necessary to ensure sampling of duodenal contents. | |||
*If there is a bloody NGT aspirate then an esophagogastroduodenoscopy (EGD) is warranted (11 to 15% of patients despite “negative” NGT aspirates are due to upper GI bleeding). | |||
*Obtaining clear fluid favors a lower GI source of bleeding. | |||
{| border="1" cellpadding="5" cellspacing="0" align="center" |class="wikitable" | |||
! colspan="2" style="background:#efefef;" | Workup and Initial Management | |||
|- | |||
|I'''nitial Evaluation''' | |||
| | |||
* Airway Breathing, Circulation | |||
|- | |||
|'''Supportive Therapy''' | |||
| | |||
* Ensure patent and protected airway | |||
* [[Intubation|Intubate]] if needed | |||
* Consider [[mechanical ventilation]] | |||
* 2 large-bore, peripheral intravenous lines | |||
* Can consider [[Central venous catheter|large-bore central venous catheter]] or intraosseous line if rapid transfuser will be needed | |||
|- | |||
|'''Blood transfusion''' | |||
| | |||
* Resuscitate with 1:1:1 of packed red blood cells (PRBCs) to fresh frozen plasma (FFP) to platelets. | |||
* Consider massive transfusion protocol | |||
* Res:Low riskto a target hemoglobin of 7 mg/dL. | |||
* Consider Sengstaken-Blakemore tube for control of immediately life-threatening upper GI bleeding | |||
|} | |||
===Assessment of severity of bleeding=== | |||
{| border="1" cellpadding="5" cellspacing="0" align="center" |class="wikitable" | |||
! colspan="1" style="background:#efefef;" | Bleeding severity | |||
! colspan="1" style="background:#efefef;" | Vital signs | |||
! colspan="1" style="background:#efefef;" | Blood loss | |||
|- | |||
|Minor | |||
|Normal | |||
|<10% | |||
|- | |||
|Moderate | |||
|Postural hypotension | |||
|10-20% | |||
|- | |||
|Severe | |||
|Shock | |||
|>25% | |||
|} | |||
===Fluid resuscitation=== | |||
*Two large caliber (16-gauge) peripheral catheters or a [[Central venous catheter|central venous line]] should be inserted in patients who are [[hemodynamically unstable]]. | |||
*The rate of fluid resuscitation is proportional to the severity of [[bleeding]] with the goal of restoring and maintaining the patient’s [[blood pressure]]. | |||
*Infusion of 500 mL of [[normal saline]] or lactated [[Ringer's lactate|Ringer's solution]] over 30 minutes is preferred treatment for patients with [[Bleeding|active bleeding]] before [[Blood type|blood type matching]] and blood [[transfusion]]. | |||
*Intensive monitoring with a [[pulmonary artery catheter]] is recommended to monitor the response of initial resuscitation efforts and any complications of fluid overload. | |||
*If the blood pressure fails to respond to initial resuscitation, the rate of fluid administration should be increased and urgent intervention (eg, angiography) considered. | |||
===Blood transfusion=== | |||
*Patients with severe [[bleeding]] need to be transfused.<ref name="pmid24063362">{{cite journal |vauthors=Al-Jaghbeer M, Yende S |title=Blood transfusion for upper gastrointestinal bleeding: is less more again? |journal=Crit Care |volume=17 |issue=5 |pages=325 |year=2013 |pmid=24063362 |pmc=4056793 |doi=10.1186/cc13020 |url=}}</ref><ref name="pmid23281973">{{cite journal |vauthors=Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C, Graupera I, Poca M, Alvarez-Urturi C, Gordillo J, Guarner-Argente C, Santaló M, Muñiz E, Guarner C |title=Transfusion strategies for acute upper gastrointestinal bleeding |journal=N. Engl. J. Med. |volume=368 |issue=1 |pages=11–21 |year=2013 |pmid=23281973 |doi=10.1056/NEJMoa1211801 |url=}}</ref> | |||
*[[Fresh frozen plasma|Fresh frozen plasma,]] [[platelets]], or both should be given to patients with [[coagulopathy]] who are actively bleeding and to those who have received more than 10 units of packed [[erythrocytes]]. | |||
{| border="1" cellpadding="5" cellspacing="0" align="center" |class="wikitable" | |||
! colspan="2" style="background:#efefef;" |Indications for transfusion | |||
|- | |||
! colspan="1" style="background:#efefef;" |Age | |||
! colspan="1" style="background:#efefef;" |Target Hematocrit | |||
|- | |||
|Elderly patient ( >45) | |||
|30% | |||
|- | |||
|Younger patient (<45) | |||
|25% | |||
|- | |||
|Patients with portal hypertension | |||
|28% | |||
|} | |||
===Triage and consultations === | |||
*All patients with visible rectal bleeding warrants an immediate evaluation in all cases. The timing and setting of the evaluation depends upon the severity of bleeding and the patient's comorbid illnesses. | |||
*A gastroenterology consultation should be obtained early in the hospital course of patients with acute lower GI bleeding. | |||
{| border="1" cellpadding="5" cellspacing="0" align="center" |class="wikitable" | |||
! colspan="1" style="background:#efefef;" |Evaluation setting | |||
! colspan="1" style="background:#efefef;" |Patient catagories | |||
|- | |||
|ICU | |||
|Patients with high-risk features. | |||
|- | |||
|Outpatient | |||
|Patients with low-risk features.<sup>†</sup> | |||
|- | |||
|Regular Ward | |||
|Most other patients can be admitted to a regular medical ward.<sup>♦</sup> | |||
|- | |||
| colspan="2" style="background:#efefef;" | | |||
* '''†''': Low-risk features include a young, otherwise healthy patient with minor, self-limited rectal bleeding suspected to be from an anal source) | |||
* ♦: Requires continuous electrocardiogram monitoring and pulse oximetry. | |||
|} | |||
===Risk stratification=== | |||
Clinical features can predict the risk of complications in patients with presumed acute lower GI bleeding. These features can also be used to categorize patients as either low or high risk. The number of high-risk features present correlates with the likelihood of a poor outcome. | |||
High-risk features include: | |||
{| border="1" cellpadding="5" cellspacing="0" align="center" |class="wikitable" | |||
! colspan="1" style="background:#efefef;" |High-risk features | |||
|- | |||
| | |||
*Hemodynamic instability (hypotension, tachycardia, orthostasis, syncope) | |||
*Persistent bleeding | |||
*Significant comorbid illnesses | |||
*Advanced age | |||
*Bleeding that occurs in a patient who is hospitalized for another reason | |||
*A prior history of bleeding from diverticulosis or angiodysplasia | |||
*Current aspirin use | |||
*Prolonged prothrombin time | |||
*A non-tender abdomen | |||
*Anemia | |||
*An elevated blood urea nitrogen level | |||
*An abnormal white blood cell count | |||
|} | |||
==Pharmacotherapy== | |||
Epinephrine is used alone or in conjunction with other surgical techniques to treat a variety of causes of LGIB. Local injection of epinephrine stops bleeding by both pressure tamponade and the vasoconstrictor effect. In patients with rebleeding, surgery should be considered. Pharmacotherapy is only used as an adjuvant therapy for all patients with LGIB. | |||
:*Preferred regimen (1): Local injection of 1:10,000 to 20,000 solution (Intra-arterial vasopressin infusions begin at a rate of 0.2 U/min. If the bleeding persists, the rate of the infusion is increased to 0.4-0.6 U/min). | |||
:*Note:- The bleeding stops in about 91% of patients receiving intra-arterial vasopressin but recurs in up to 50% of patients when the infusion is stopped. | |||
===Major contraindications=== | |||
*Closed-angle glaucoma | |||
*Labor | |||
*Shock | |||
*Sulfite hypersensitivity | |||
*CAD, PAD | |||
===Complications=== | |||
During vasopressin infusion, monitor patients for: | |||
*Recurrent hemorrhage | |||
*Myocardial ischemia (Nitroglycerine drip can be used to overcome cardiac complications). | |||
*Arrhythmias | |||
*Hypertension | |||
*Volume overload with hyponatremia. | |||
==Colonoscopy== | |||
*Colonoscopy is considered as the initial diagnostic modality of choice in patients presenting with lower GI bleeding. Colonoscopy can identify the origin of severe LGI bleeding in 74% to 82% of patients. | |||
*As long as patients remain stable during the bowel preparation and sedation, colonoscopy has the advantage of not only localizing the source of bleeding, but also allowing intervention via clips, epinephrine injection, thermoregulation, or laser photocoagulation. | |||
*In patients with massive lower GI bleeding, colonoscopic hemostasis is an effective means of controlling bleeding from a diverticular source when appropriately skilled providers are available. | |||
*In cases in which no source of bleeding is seen on colonoscopy, esophagogastroduodenoscopy should be undertaken, as occasionally, brisk UGIB increases transit time and presents as blood per rectum. | |||
*If a patient has pain associated with bleeding, ischemic bowel disease should be considered. CTA may be a more appropriate first-line investigation in patients with abdominal pain or suspected peritonitis. | |||
===Timing of colonoscopy=== | |||
*In patients with ongoing bleeding or high-risk clinical features, a colonoscopy should be performed within 24 hours of presentation after adequate colon preparation to potentially improve diagnostic and therapeutic yield. | |||
===Bowel preparation=== | |||
*In a patient who is not actively bleeding, rapid bowel preparation can be administered with 3 to 4 L of polyethylene glycol. | |||
*This can be administered orally or via a nasogastric tube to avoid nausea and reduce the potential risk of aspiration. | |||
*However, there is the potential risk of fluid overload in the acutely ill patient receiving rapid bowel preparation this way. | |||
*Metoclopramide, 10 to 20 mg, can be administered with the bowel preparation as a prokinetic agent to facilitate gastric emptying and reduce the risk of vomiting. | |||
*Some have advocated colonoscopy following limited bowel preparation using polyethylene glycol purges supplemented with rectal enemas. | |||
*Blood is cathartic to the colon and tends to facilitate the emptying of colonic residue. | |||
===Complications=== | |||
*Perforation of the luminal wall, resulting in peritonitis and sepsis. | |||
*Poor visualization in an unprepared colon. | |||
===Non surgical options=== | |||
*Once the bleeding site is localized, therapeutic options include coagulation and injection with vasoconstrictors or sclerosing agents. | |||
*In cases of diverticular bleeding, bipolar probe coagulation, epinephrine injection, and metallic clips may be used. | |||
*If recurrent bleeding is present, the affected bowel segment can be resected. | |||
*In cases of angiodysplasia, thermal therapy, such as electrocoagulation or argon plasma coagulation, is generally successful. | |||
*Angiodysplastic lesions may be missed at colonoscopy if the lesions are small or covered with blood clots. | |||
*Endoscopic hemostasis therapy is a safe and effective method to control high-risk indications of hemorrhage: active bleeding, nonbleeding visible vessel, or adherent clot. | |||
*It is also effective for diverticular bleeding, angioectasia bleeding, and post-polypectomy bleeding. | |||
*In patients with brisk, active lower gastrointestinal bleeding, obtain a surgical consultation. | |||
{| class="wikitable" | |||
! | |||
! | |||
! | |||
! | |||
|- | |||
|Diverticulosis | |||
| | |||
| | |||
| | |||
|- | |||
|Angiodysplasia | |||
| | |||
| | |||
| | |||
|- | |||
|Hemmrohoids | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
| | |||
| | |||
| | |||
|} | |||
===CXXX=== | |||
*Diverticula are most common in the descending and sigmoid colon. | |||
*Most of the time bleeding from diverticulosis stops spontaneously, however, in about 5% of patients, the bleeding can be massive and life-threatening. | |||
==References== | |||
{{reflist|2}} | |||
Latest revision as of 19:13, 13 December 2017
Lower GI bleeding is defined as any bleed that occurs distal to the ligament of Treitz.
Incidence
- In the United States the incidence of LGIB ranges from 20.5 to 27 per 100,000 persons per year.
Age
- There is a greater than 200 fold increase from the third to the ninth decade of life.
Classification
- Lower GI bleeding can be classified into 3 groups based on the severity of bleeding:
- Occult lower GI bleeding
- Moderate lower GI bleeding
- Severe lower GI bleeding
| Severe lower GI bleeding | Moderate lower GI bleeding | Occult lower GI bleeding | |
|---|---|---|---|
| Age | > 65 years | Occur at any age | Any age |
| Presenting symptoms | Hematochezia or bright red blood per rectum. | Hematochezia or melena. | Symptoms of anemia (fatigue, tirdness) |
| Hemodynamics | Unstable | Stable | Stable |
| Lab findings | hemoglobin equal to or less than 6 g/dl. | Microcytic anemia | Microcytic hypochromic anemia due to chronic blood loss. |
| Differential | Diverticulosis and angiodysplasias | Neoplastic disease Inflammatory, <br> infectious, benign anorectal, and congenital diseases. | Inflammatory, neoplastic and congenital. |
Blood supply
- The SMA and IMA are connected by the marginal artery of Drummond.
- This vascular arcade runs in the mesentery close to the bowel.
- As patients age, there is increased incidence of occlusion of the IMA.
- The left colon stays perfused, primarily because of the marginal artery.
| Lower GI Tract | Arterial Supply | Venous Drainage | |
|---|---|---|---|
| Midgut |
|
|
|
| Hindgut |
|
|
|
| ɸ -Except lower rectum, which drains into the systemic circulation. | |||

Source: By Anpol42 (Own work) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons
Pathogenesis
Diverticulosis is the most common etiology of lower GI bleeding accounting for 30% of all cases, followed by anorectal disease, ischemia, inflammatory bowel disease (IBD), neoplasia and arteriovenous (AV) malformations.
- Diverticulosis
- The colonic wall weakens with age and results in the formation of saclike protrusions known as diverticula.
- These protrusions generally occur at the junction of blood vessel penetrating through the mucosa and circular muscle fibers of the colon.
- Diverticula are most common in the descending and sigmoid colon.
- Despite the majority of diverticula being on the left side of the colon, diverticular bleeding originates from the right side of the colon in 50% to 90% of instances.
- Most of the time bleeding from diverticulosis stops spontaneously, however, in about 5% of patients, the bleeding can be massive and life-threatening.
Source:By Anpol42 (Own work) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons
- Anorectal disease
- Hemorrhoids and anal fissures are the most common disease under anorectal disease responsible for GI bleeding.
- Hemorrhoids are engorged vessels in the normal anal cushions. When swollen, this tissue is very friable and susceptible to trauma, which leads to painless, bright red bleeding.
- Anal fissures are defined as a tear in the anal mucosa. With the passage of stool, the mucosa continues to tear and leads to bright red bleeding.
- Mesenteric Ischemia
- Mesenteric ischemia results when there is inadequate blood supply at the level of the small intestine.
- 2 or more vessels (celiac, SMA, or IMA) must be involved for symptoms to occur.
- Non occlusive mesenetric ischemia affects critically ill patients who are vasopressor-dependent.
- Venous thrombosis of the visceral vessels can also precipitate an acute ischemic event.
- Ischemic Colitis
- Ischemic colitis is caused by poor perfusion of the colon, which results in the inability of that area of the colon to meet its metabolic demands.
- It can be gangrenous or nongangrenous, acute, transient, or chronic.
- The left colon is predominantly affected, with the splenic flexure having increased susceptibility.
- Intraluminal hemorrhage occurs as the mucosa becomes necrotic, sloughs, and bleeds.
- Damage to the tissue is caused both with the ischemic insult as well as reperfusion injury.
- Inflammatory Bowel Disease
- In Crohn's disease T cell activation stimulates interleukin (IL)-12 and tumor necrosis factor (TNF)-a, which causes chronic inflammation and tissue injury.
- Initially, inflammation starts focally around the crypts, followed by superficial ulceration of the mucosa.
- The deep mucosal layers are then invaded in a noncontinuous fashion, and noncaseating granulomas form, which can invade through the entire thickness of the bowel and into the mesentery and surrounding structures.
- In ulcerative colitis T cells cytotoxic to the colonic epithelium accumulate in the lamina propria, accompanied by B cells that secrete immunoglobulin G (IgG) and IgE.
- This results in inflammation of the crypts of Lieberkuhn, with abscesses and pseudopolyps.
- Ulcerative colitis generally begins at the rectum and is a continuous process confined exclusively to the colon.
- Neoplasia
- Colon carcinoma follows a distinct progression from polyp to cancer.
- Mutations of multiple genes are required for the formation of adenocarcinoma, including the APC gene, Kras, DCC, and p53.
- Certain hereditary syndromes are also classified by defects in DNA mismatch repair genes and microsatellite instability.
- These tumors tend to bleed slowly, and patients present with hemocult positive stools and microcytic anemia.
- Although cancers of the small bowel are much less common than colorectal cancers, they should be ruled out in cases of lower GI bleeding in which no other source is identified.
- AV Malformation/Angiodysplasia
- In AV malformation direct connections between arteries and veins occur in the colonic submucosa.
- The lack of capillary buffers causes high pressure blood to enter directly into the venous system, making these vessels at high risk of rupture into the bowel lumen.
- In Angiodysplasia over time, previously healthy blood vessels of the cecum and ascending colon degenerate and become prone to bleeding.
- Although 75% of angiodysplasia cases involve the right colon, they are a significant cause of obscure bleeding and the most common cause of bleeding from the small bowel in the elderly.
Epidemiology
Prevalence
- Approximately 20 patients/100,000 population in the U.S.
Incidence
- The estimated annual incidence of lower GI bleeding is approximately 0.03% in the adult population as a whole.
Demographics
Gender
- More common in men than women
Age
- Rare in children
- The incidence of lower GI bleeding increases with age with a 200-fold increase from the second to eighth decades of life la.
- Largely due to the increase in the prevalence of diverticular disease and angiodysplasia with age.
Symptoms
- Occult LGIB may present with symptoms of iron deficiency anemia such as fatigue, palpitations, and dyspnea.
- Patients with intussusception may present with pallor and vomiting in addition to LGIB
- Associated symptoms, such as abdominal pain or change in bowel habits, may also aide in the diagnosis
- Bloody diarrhea associated with abdominal pain may suggest an infectious cause or IBD in a younger patient and ischemic colitis in an older patient with vascular disease
- Painless bleeding usually suggests angiodysplasia, diverticular disease, or internal hemorrhoids
- Perianal pain suggests a perianal fissure or fistula
History
- A detailed description of the nature of the blood loss can help in pinpointing the likely source of bleeding.
Past Medical History
- The clinical history should identify whether this is a recurrent bleed.
- Bleeding from angiodysplasia is usually recurrent and chronic, but severe bleeding resulting in hemodynamic instability can occur.
- Associated weight loss suggests malignancy.
- The presence of systemic diseases such as atherosclerotic disease, IBD, coagulopathies, and HIV, and a history of pelvic irradiation for malignancy should be considered
Past Surgical History
- A history of recent colonic polypectomy or biopsy indicates iatrogenic bleeding.
- This is usually low grade and limited, although it can be severe if an underlying artery is involved or if there is an inadequate coagulation of the polypectomy stalk.
- In 1.5% of polypectomies bleeding occurs immediately. However, delayed bleeding can occur several hours or days following the procedure
- It is essential to establish the presence of comorbid diseases, as these not only help in diagnosis but may also influence treatment.
Family history
- A family history of diseases such as IBD or colorectal malignancy is relevant.
Symptoms
- The clinical presentation of LGIB varies with the anatomic source of the bleeding.
- Commonly, LGIB from the right side of the colon can manifest as maroon stools, whereas a left-sided bleeding source may be evidenced by bright red blood per rectum.
- The presentation of LGIB can also vary depending on the etiology.
- A young patient may present with fever, dehydration, abdominal cramps, and hematochezia caused by infectious or noninfectious (idiopathic) colitis.
- An older patient may present with painless bleeding and minimal symptoms caused by diverticular bleeding or angiodysplasia.
- LGIB can be mild and intermittent, as often is the case with angiodysplasia, or it may be moderate or severe, as may be the situation in diverticula-related bleeding.
- Young patients may present with abdominal pain, rectal bleeding, diarrhea, and mucous discharge that may be associated with IBD.
- Elderly patients presenting with abdominal pain, rectal bleeding, and diarrhea may have ischemic colitis.
- Elderly patients with atherosclerotic heart disease may present with intermittent LGIB and syncope that may be due to angiodysplastic lesions.
- Stools streaked with blood, perianal pain, and blood drops on the toilet paper or in the toilet bowl may be associated with perianal pathology, such as anal fissure or hemorrhoidal bleeding.
- The passage of maroon stools or bright red blood from the rectum is usually indicative of massive lower GI hemorrhage.
- Massive LGIB is a life-threatening condition in which patients present with a systolic blood pressure (SBP) of below 90 mm Hg and a hemoglobin (Hb) level of 6 g/dL or less.
| Disease | Symptoms | |
|---|---|---|
| Diverticular bleeding | Painless bleeding
Mild abdominal cramping If the bleeding is brisk and voluminous, patients may be hypotensive and display signs of shock | |
| Angiodysplasia | Painless, hematochezia or melena (slow but repeated bleeding episodes)
Syncope | |
| Colitis | Ischemic colitis | Fever
Abdominal pain Bloody diarrhea Dehydration Hypotension in severe cases Weight loss |
| Infectious colitis | ||
| Radiation-induced colitis | ||
| Ulcerative colitis | ||
| Colon cancer | Right-sided bleeding (Maroon stools or melena)
Insidious Patients presents with iron-deficiency anemia and syncope Whereas left-sided colonic neoplasms can present as bright red blood per rectum | |
| Hemorrhoids | Painless, whereas bleeding secondary to fissures tends to be painful.
Can also present with strangulation, hematochezia, and pruritus. | |
Common causes
- Colonic diverticulosis
- Colonic diverticulosisis the most common cause of acute LGIB in the western world, accounting for 15% to 55% of all LGIB
- Diverticula can occur anywhere in the gastrointestinal tract, but are most common in the sigmoid colon. However, approximately 60% of diverticular bleeds arise from diverticula in the right colon, highlighting a tendency for right-sided diverticula to bleed
- Hemorrhage results from rupture of the intramural branches (vasa recta) of the marginal artery at the dome of a diverticulum and can give rise to a massive, life-threatening LGIB
- This is by far the most common cause of bleeding in the elderly, as the prevalence of diverticular disease increases with age, being as high as 85% by the age of 85 years
- Obesity has recently been recognized as a risk factor in the development of diverticular disease, and the risk of diverticular bleeding in this group of patients is higher than that in patients who are not obese
- Vascular ectasias (angiodysplasias/angioectasias):
- Tortuous dilated submucosal vessels that account for approximately 10% of LGIB.
- They appear endoscopically as small, flat lesions (5-10 mm) with ectatic capillaries radiating from a central vessel (Fig. 1)
- The prevalence of angiodysplasia in the gastrointestinal tract is not well known, but a pooled analysis of three colonoscopic cancer screening studies detected angiodysplasia in 0.8% of the patients The prevalence of angiodysplasia is higher in older populations and, in the past, has been linked to certain conditions such as end-stage renal disease, Von Willebrand disease , and aortic stenosis In one series, 37% of colonic dysplasias were found in the cecum, 17% in the ascending colon, 7% in the transverse colon, 7% in the descending colon, and 32% in rectosigmoid area
- Angiodysplasia can also be found throughout the small bowel and is responsible for up to 40% of small intestinal bleeding in patients older than 40 years.
- Angiodysplasia of the stomach and duodenum is responsible for up to 7% of UGIB I
- Iatrogenic:
- Bleeding is recognized as the most common complication of colonoscopy and polypectomy, occurring in 0.3% to 6.1% of polypectomies
- Risk factors for bleeding include polyp size greater than 1 cm, patient age older than 65 years, presence of comorbid disease, and polypectomy using the cutting mode of current
- The risk is also greater in patients taking anticoagulant or antiplatelet agents
- Ischemic colitis:
- Ischemic colitis accounts for approximately 20% of LGIB
- Ischemia results from a sudden reduction in blood flow to the mesenteric vessels as a result of hypotension, occlusion, or spasm of the mesenteric vessels
- Nonocclusive disease typically affects the watershed areas of the bowels, such as the splenic flexure and adjacent transverse colon due to the poor blood supply from the marginal artery.
- Occlusive disease is rarer but can occur as a result of thrombus formation or embolus.
- It is a recognized complication of aortic surgery
- Elderly patients with comorbid disease are at higher risk of developing ischemic colitis.
- There may be a history of ischemic heart disease
- The majority of patients with ischemic colitis improve following conservative management; however, approximately 20% will progress to develop colonic gangrene
- Other complications include chronic colitis and stricture formation
- Diagnosis requires a high index of suspicion
- Colorectal malignancy:
- Colorectal cancer accounts for approximately 10% of bleeds, either as occult bleeding presenting with anemia or as frank blood loss per rectum
- A family history of colorectal cancer is important to establish
- Anorectal abnormalities:
- Hemorrhoids, fissures, fistulae, and polyps can all present with bright red rectal bleeding, which may be intermittent in nature
- Hemorrhoids are the most common cause of rectal bleeding in adults younger than 50 years
- The finding of hemorrhoids in older patients with LGIB should not preclude further investigation, as hemorrhoids are an extremely common finding and may not be the cause of bleeding
- Inflammatory bowel disease (IBD):
- IBD refers to both Crohn disease and ulcerative colitis Accounts for 5% to 10% of bleeds.
- It is by far the most common cause of LGIB in Asian populations in whom the prevalence of diverticular disease is much lower
- A previous history of IBD in patients with LGIB is important, as these patients have a higher risk of developing colorectal malignancy than do the general population
- Infectious colitis:
- The most common organisms in the U.S. are species ofSalmonella,Campylobacter,Shigella, andYersinia
Rare causes
- Colonic polyps:
- These can occur in isolation or as part of an inherited polyposis syndrome
- Can cause occult or overt LGIB
- Radiation proctitis:
- This usually occurs a few months following ionizing radiation for pelvic malignancies (Fig. 2). In one study of patients with radiation proctitis following pelvic irradiation, 69% presented with bleeding within 1 year and 96% within 2 years
- Rectal varices:
- Associated with portal hypertension; may result in massive bleeding
- Stercoral ulceration:
- Can cause significant fresh rectal bleeding in elderly constipated patients
- Meckel diverticulum:
- These small bowel diverticula may contain ectopic gastric mucosa that can ulcerate and cause bleeding
- They are the most common cause of massive LGIB in young children, and can be diagnosed with angiography, Meckel scans, and radionuclide imaging
- Intussusception :
- More common in children, with the highest incidence between the ages of 6 months and 2 years
- Henoch-Schönlein purpura (HSP):
- Most commonly affects children
- Bleeding may be a direct result of vasculitis or secondary to intussusception, which is associated with HSP
- Aortoenteric fistula:
- Abdominal aortic aneurysms, especially those of the inflammatory type, may fistulate into the small bowel, giving rise to a massive, life-threatening hemorrhage
- Peutz-Jeghers syndrome:
- Polyps may give rise to frank or occult bleeding
- Klippel-Trenaunay-Weber syndrome:
- Hemangiomas in the colon can cause significant bleeding
- Hereditary hemorrhagic telangiectasia:
- Blood loss from mucosal telangiectasia can be chronic or acute
- Neurofibromatosis :
- Neurofibromas within the lumen of the bowel can ulcerate, causing bleeding
- Blue rubber bleb syndrome:
- Bleeding can arise from hemangiomas in the bowel Usually occult in nature
Risk factors
Common risk factors in the development of lower GI bleeding include:[1][2][3][4]
- Advancing age
- Previous history of gastrointestinal bleed
- Chronic constipation
- Hematologic disorders
- Anticoagulants medications
- Nonsteroidal anti-inflammatory drugs
- Human immunodeficiency virus
| Chronic constipation | Results in colonic diverticula and predispose patients to anal fissures and hemorrhoid formation |
| Hematologic disorders | Deficiencies in clotting factors, such as factor VII and factor VIII, predispose persons to LGIB |
| Anticoagulants medications | Patients taking warfarin and heparin, aspirin, and platelet inhibitors are at increased risk of bleeding in general |
| Nonsteroidal anti-inflammatory drugs | NSAIDs cause ulceration in the terminal ileum and proximal colon, and can exacerbate IBD |
| Human immunodeficiency virus | In patients with HIV, bleeding is caused by opportunistic infections, cytomegalovirus colitis, Kaposi sarcoma, or lymphoma |
Management
Initial Evaluation
- In patients with acute lower gastrointestinal bleeding who are unstable rapid assessment and resuscitation should be initiated even before diagnostic evaluation.
- The initial steps in the management of a patient with lower gastrointestinal bleeding are to assess the severity of bleeding, and then institute fluid and blood resuscitation as needed.
- Once hemodynamic stability is achieved, nasogastric lavage should be performed to rule of upper GI source.
- Equilibration between the intravascular and extravascular volumes cannot be achieved until 24 to 72 hours after bleeding has occurred.
Role of Nasogastric tube (NGT)
- Nasogastric tube (NGT) lavage is recommended in all patients with lower gastrointestinal bleeding once the patient is stabilized.
- A carefully placed nasogastric tube (NGT) with irrigation and aspiration of bile is necessary to ensure sampling of duodenal contents.
- If there is a bloody NGT aspirate then an esophagogastroduodenoscopy (EGD) is warranted (11 to 15% of patients despite “negative” NGT aspirates are due to upper GI bleeding).
- Obtaining clear fluid favors a lower GI source of bleeding.
| Workup and Initial Management | |
|---|---|
| Initial Evaluation |
|
| Supportive Therapy |
|
| Blood transfusion |
|
Assessment of severity of bleeding
| Bleeding severity | Vital signs | Blood loss |
|---|---|---|
| Minor | Normal | <10% |
| Moderate | Postural hypotension | 10-20% |
| Severe | Shock | >25% |
Fluid resuscitation
- Two large caliber (16-gauge) peripheral catheters or a central venous line should be inserted in patients who are hemodynamically unstable.
- The rate of fluid resuscitation is proportional to the severity of bleeding with the goal of restoring and maintaining the patient’s blood pressure.
- Infusion of 500 mL of normal saline or lactated Ringer's solution over 30 minutes is preferred treatment for patients with active bleeding before blood type matching and blood transfusion.
- Intensive monitoring with a pulmonary artery catheter is recommended to monitor the response of initial resuscitation efforts and any complications of fluid overload.
- If the blood pressure fails to respond to initial resuscitation, the rate of fluid administration should be increased and urgent intervention (eg, angiography) considered.
Blood transfusion
- Patients with severe bleeding need to be transfused.[5][6]
- Fresh frozen plasma, platelets, or both should be given to patients with coagulopathy who are actively bleeding and to those who have received more than 10 units of packed erythrocytes.
| Indications for transfusion | |
|---|---|
| Age | Target Hematocrit |
| Elderly patient ( >45) | 30% |
| Younger patient (<45) | 25% |
| Patients with portal hypertension | 28% |
Triage and consultations
- All patients with visible rectal bleeding warrants an immediate evaluation in all cases. The timing and setting of the evaluation depends upon the severity of bleeding and the patient's comorbid illnesses.
- A gastroenterology consultation should be obtained early in the hospital course of patients with acute lower GI bleeding.
| Evaluation setting | Patient catagories |
|---|---|
| ICU | Patients with high-risk features. |
| Outpatient | Patients with low-risk features.† |
| Regular Ward | Most other patients can be admitted to a regular medical ward.♦ |
| |
Risk stratification
Clinical features can predict the risk of complications in patients with presumed acute lower GI bleeding. These features can also be used to categorize patients as either low or high risk. The number of high-risk features present correlates with the likelihood of a poor outcome. High-risk features include:
| High-risk features |
|---|
|
Pharmacotherapy
Epinephrine is used alone or in conjunction with other surgical techniques to treat a variety of causes of LGIB. Local injection of epinephrine stops bleeding by both pressure tamponade and the vasoconstrictor effect. In patients with rebleeding, surgery should be considered. Pharmacotherapy is only used as an adjuvant therapy for all patients with LGIB.
- Preferred regimen (1): Local injection of 1:10,000 to 20,000 solution (Intra-arterial vasopressin infusions begin at a rate of 0.2 U/min. If the bleeding persists, the rate of the infusion is increased to 0.4-0.6 U/min).
- Note:- The bleeding stops in about 91% of patients receiving intra-arterial vasopressin but recurs in up to 50% of patients when the infusion is stopped.
Major contraindications
- Closed-angle glaucoma
- Labor
- Shock
- Sulfite hypersensitivity
- CAD, PAD
Complications
During vasopressin infusion, monitor patients for:
- Recurrent hemorrhage
- Myocardial ischemia (Nitroglycerine drip can be used to overcome cardiac complications).
- Arrhythmias
- Hypertension
- Volume overload with hyponatremia.
Colonoscopy
- Colonoscopy is considered as the initial diagnostic modality of choice in patients presenting with lower GI bleeding. Colonoscopy can identify the origin of severe LGI bleeding in 74% to 82% of patients.
- As long as patients remain stable during the bowel preparation and sedation, colonoscopy has the advantage of not only localizing the source of bleeding, but also allowing intervention via clips, epinephrine injection, thermoregulation, or laser photocoagulation.
- In patients with massive lower GI bleeding, colonoscopic hemostasis is an effective means of controlling bleeding from a diverticular source when appropriately skilled providers are available.
- In cases in which no source of bleeding is seen on colonoscopy, esophagogastroduodenoscopy should be undertaken, as occasionally, brisk UGIB increases transit time and presents as blood per rectum.
- If a patient has pain associated with bleeding, ischemic bowel disease should be considered. CTA may be a more appropriate first-line investigation in patients with abdominal pain or suspected peritonitis.
Timing of colonoscopy
- In patients with ongoing bleeding or high-risk clinical features, a colonoscopy should be performed within 24 hours of presentation after adequate colon preparation to potentially improve diagnostic and therapeutic yield.
Bowel preparation
- In a patient who is not actively bleeding, rapid bowel preparation can be administered with 3 to 4 L of polyethylene glycol.
- This can be administered orally or via a nasogastric tube to avoid nausea and reduce the potential risk of aspiration.
- However, there is the potential risk of fluid overload in the acutely ill patient receiving rapid bowel preparation this way.
- Metoclopramide, 10 to 20 mg, can be administered with the bowel preparation as a prokinetic agent to facilitate gastric emptying and reduce the risk of vomiting.
- Some have advocated colonoscopy following limited bowel preparation using polyethylene glycol purges supplemented with rectal enemas.
- Blood is cathartic to the colon and tends to facilitate the emptying of colonic residue.
Complications
- Perforation of the luminal wall, resulting in peritonitis and sepsis.
- Poor visualization in an unprepared colon.
Non surgical options
- Once the bleeding site is localized, therapeutic options include coagulation and injection with vasoconstrictors or sclerosing agents.
- In cases of diverticular bleeding, bipolar probe coagulation, epinephrine injection, and metallic clips may be used.
- If recurrent bleeding is present, the affected bowel segment can be resected.
- In cases of angiodysplasia, thermal therapy, such as electrocoagulation or argon plasma coagulation, is generally successful.
- Angiodysplastic lesions may be missed at colonoscopy if the lesions are small or covered with blood clots.
- Endoscopic hemostasis therapy is a safe and effective method to control high-risk indications of hemorrhage: active bleeding, nonbleeding visible vessel, or adherent clot.
- It is also effective for diverticular bleeding, angioectasia bleeding, and post-polypectomy bleeding.
- In patients with brisk, active lower gastrointestinal bleeding, obtain a surgical consultation.
| Diverticulosis | |||
| Angiodysplasia | |||
| Hemmrohoids | |||
CXXX
- Diverticula are most common in the descending and sigmoid colon.
- Most of the time bleeding from diverticulosis stops spontaneously, however, in about 5% of patients, the bleeding can be massive and life-threatening.
References
- ↑ Navuluri R, Kang L, Patel J, Van Ha T (2012). "Acute lower gastrointestinal bleeding". Semin Intervent Radiol. 29 (3): 178–86. doi:10.1055/s-0032-1326926. PMC 3577586. PMID 23997409.
- ↑ Strate LL (2005). "Lower GI bleeding: epidemiology and diagnosis". Gastroenterol. Clin. North Am. 34 (4): 643–64. doi:10.1016/j.gtc.2005.08.007. PMID 16303575.
- ↑ Ríos A, Montoya MJ, Rodríguez JM, Serrano A, Molina J, Ramírez P, Parrilla P (2007). "Severe acute lower gastrointestinal bleeding: risk factors for morbidity and mortality". Langenbecks Arch Surg. 392 (2): 165–71. doi:10.1007/s00423-006-0117-6. PMID 17131153.
- ↑ Strate LL, Orav EJ, Syngal S (2003). "Early predictors of severity in acute lower intestinal tract bleeding". Arch. Intern. Med. 163 (7): 838–43. doi:10.1001/archinte.163.7.838. PMID 12695275.
- ↑ Al-Jaghbeer M, Yende S (2013). "Blood transfusion for upper gastrointestinal bleeding: is less more again?". Crit Care. 17 (5): 325. doi:10.1186/cc13020. PMC 4056793. PMID 24063362.
- ↑ Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C, Graupera I, Poca M, Alvarez-Urturi C, Gordillo J, Guarner-Argente C, Santaló M, Muñiz E, Guarner C (2013). "Transfusion strategies for acute upper gastrointestinal bleeding". N. Engl. J. Med. 368 (1): 11–21. doi:10.1056/NEJMoa1211801. PMID 23281973.