Medical ventilator
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
A medical ventilator may be defined as an automatic machine designed to mechanically move breatheable air into and out of the lungs, to provide respiration for a patient who is physically unable to breathe, or breathing insufficiently.
Ventilators are chiefly used in intensive care medicine, home care, and emergency medicine (as standalone units) and in anesthesia (as a component of an anesthesia machine).
Function
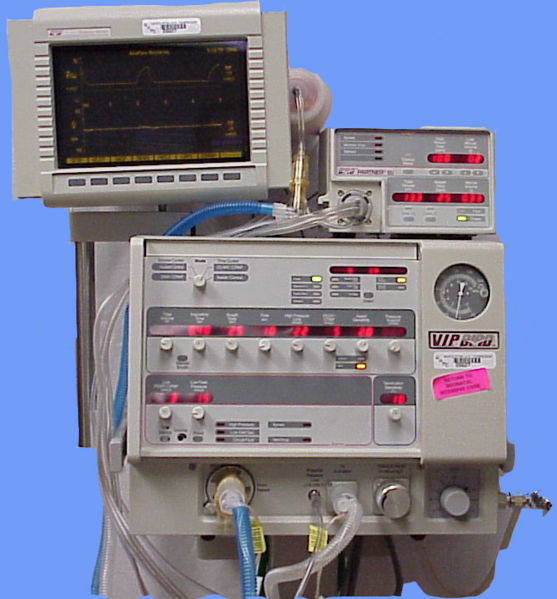
In its simplest form, a modern positive pressure ventilator consists of a compressible air reservoir, air and oxygen supplies, a set of valves and tubes, and a disposable or reusable "patient circuit". The air reservoir is pneumatically compressed several times a minute to deliver room-air, or in most cases, an air/oxygen mixture to the patient. When overpressure is released, the patient will exhale passively due to the lungs' elasticity, the exhaled air being released usually through a one-way valve within the patient circuit. The oxygen content of the inspired gas can be set from 21 percent (ambient air) to 100 percent (pure oxygen). Pressure and flow characteristics can be set mechanically or electronically.
Ventilators may also be equipped with monitoring and alarm systems for patient-related parameters (e.g. pressure, volume, and flow) and ventilator function (e.g. air leakage, power failure, mechanical failure), backup batteries, oxygen tanks, and remote control. The pneumatic system is nowadays often replaced by a computer-controlled turbopump.
Modern ventilators are electronically controlled by a small embedded system to allow exact adaptation of pressure and flow characteristics to an individual patient's needs. Fine-tuned ventilator settings also serve to make ventilation more tolerable, and comfortable for the patient. In Germany, Canada, and the United States, respiratory therapists are responsible for tuning these settings.
The patient circuit usually consists of a set of three durable, yet lightweight plastic tubes, separated by function (e.g. inhaled air, patient pressure, exhaled air). Determined by the type of ventilation needed, the patient-end of the circuit may be either noninvasive or invasive.
Noninvasive methods, which are adequate for patients who require a ventilator only while sleeping and resting, mainly employ a nasal mask. Invasive methods require intubation, which for long-term ventilator dependence will normally be a tracheotomy canula, as this is much more comfortable and practical for long-term care than is larynx or nasal intubation.
Life-critical system
Because the failure of a mechanical ventilation system may result in death, it is classed as a life-critical system, and precautions must be taken to ensure that mechanical ventilation systems are highly reliable. This includes their power-supply provision.
Mechanical ventilators are therefore carefully designed so that no single point of failure can endanger the patient. They usually have manual backup mechanisms to enable hand-driven respiration in the absence of power. Some systems are also equipped with compressed-gas tanks and backup batteries to provide ventilation in case of power failure or defective gas supplies, and methods to operate or call for help if their mechanisms or software fails.
Ventilator history
The early history of mechanical ventilation begins with various versions of what was eventually called the iron lung, a form of noninvasive negative pressure ventilator widely used during the polio epidemics of the 20th century after the introduction of the "Drinker respirator" in 1928, and the subsequent improvements introduced by John Haven Emerson in 1931. Other forms of noninvasive ventilators, also used widely for polio patients, include Biphasic Cuirass Ventilation, the rocking bed, and rather primitive positive pressure machines.
In 1949, John Haven Emerson developed a mechanical assister for anesthesia with the cooperation of the anesthesia department at Harvard University. Mechanical ventilators began to be used increasingly in anesthesia and intensive care during the 1950's. Their development was stimulated both by the need to treat polio patients and the increasing use of muscle relaxants during anesthesia. Relaxant drugs paralyze the patient and improve operating conditions for the surgeon, but also paralyze the respiratory muscles and stop breathing.
In the United States, the Bird ventilator was an early gas driven model, it required no electrical power source. In the United Kingdom, the East Radcliffe and Beaver models were early examples, the later using an automotive wiper motor to drive the bellows used to inflate the lungs. Electric motors were, however, a problem in the operating theatres of that time, as their use caused an explosion hazard in the presence of flammable anesthetics such as ether and cyclopropane. In 1952, Roger Manley of the Westminster Hospital, London, developed a ventilator which was entirely gas driven, and became the most popular model used in Europe. It was an elegant design, and became a great favourite with European anesthetists for four decades, prior to the introduction of models controlled by electronics. It was independent of electrical power, and caused no explosion hazard. The original Mark I unit was developed to become the Manley Mark II in collaboration with the Blease company, who manufactured many thousands of these units. Its principle of operation was very simple, an incoming gas flow was used to lift a weighted bellows unit, which fell intermittently under gravity, forcing breathing gases into the patient's lungs. The inflation pressure could be varied by sliding the movable weight on top of the bellows. The volume of gas delivered was adjustable using a curved slider, which restricted bellows excursion. Residual pressure after the completion of expiration was also configurable, using a small weighted arm visible to the lower right of the front panel. This was a robust unit and its availability encouraged the introduction of positive pressure ventilation techniques into mainstream European anesthetic practice.
High frequency percussive ventilation
High-frequency percussive ventilation (HFPV) began to be used in selected centres in the 1980's. It is a hybrid of conventional mechanical ventilation and high-frequency oscillatory ventilation. It has been used to salvage patients with persistent hypoxemia when on conventional mechanical ventilation or, in some cases, used as a primary modality of ventilatory support from the start. [1] [2]
External links
- Simulation of an anesthesia machine with a piston ventilator
- International Ventilator Users Network (IVUN), a subsidiary of Post-Polio Health International. Information about home mechanical ventilation.
References
- ↑ Eastman A, Holland D, Higgins J, et al. "High-frequency percussive ventilation improves oxygenation in trauma patients with acute respiratory distress syndrome: a retrospective review" Am J Surg (2006) 192(2): 191-195
- ↑ http://ccforum.com/content/7/5/342
See also
da:Respirator de:Beatmungsgerät no:Respirator nn:Respirator sv:Respirator