Yellow fever: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
'''For the WikiDoc page for this topic, click [[Yellow fever|here]]''' | '''For the WikiDoc page for this topic, click [[Yellow fever | here]]''' | ||
{{DiseaseDisorder infobox | | {{DiseaseDisorder infobox | | ||
Name = yellow fever | Name = yellow fever | ||
Revision as of 14:48, 1 August 2011
For the WikiDoc page for this topic, click here Template:DiseaseDisorder infobox
| Yellow fever virus | ||||||||
|---|---|---|---|---|---|---|---|---|
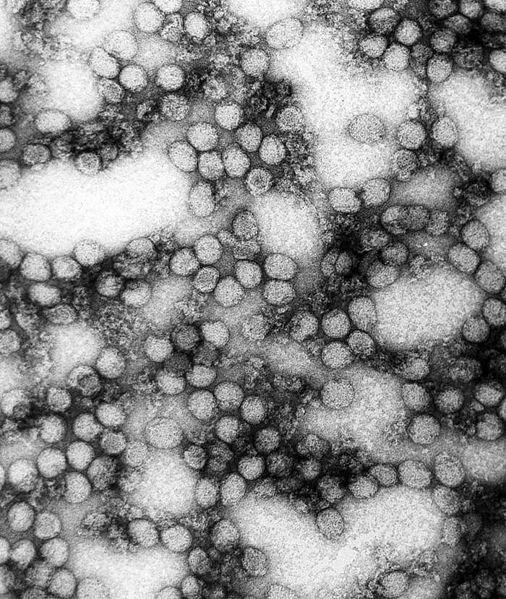 TEM micrograph: Multiple yellow fever virions (234,000x magnification).
| ||||||||
| Virus classification | ||||||||
|
|
WikiDoc Resources for Yellow fever |
|
Articles |
|---|
|
Most recent articles on Yellow fever Most cited articles on Yellow fever |
|
Media |
|
Powerpoint slides on Yellow fever |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Yellow fever at Clinical Trials.gov Clinical Trials on Yellow fever at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Yellow fever
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Yellow fever Discussion groups on Yellow fever Patient Handouts on Yellow fever Directions to Hospitals Treating Yellow fever Risk calculators and risk factors for Yellow fever
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Yellow fever |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Yellow fever (also called yellow jack, black vomit or vomito negro, or sometimes American Plague) is an acute viral disease.[1] It is an important cause of hemorrhagic illness in many African and South American countries despite existence of an effective vaccine. The yellow refers to the jaundice symptoms that affect some patients.[2] Yellow fever has been a source of several devastating epidemics. French soldiers were attacked by yellow fever during the 1802 Haitian Revolution; more than half of the army perished due to the disease.[3] Outbreaks followed by thousands of deaths occurred periodically in other Western Hemisphere locations until research, which included human volunteers (some of whom died), led to an understanding of the method of transmission to humans (primarily by mosquitos) and development of a vaccine and other preventative efforts in the early 20th century. Despite the costly and sacrificial breakthrough research by Cuban physician Carlos Finlay, American physician Walter Reed, and many others over 100 years ago, unvaccinated populations in many developing nations in Africa and Central and South America continue to be at risk.[4] As of 2001, the World Health Organization (WHO) estimates that yellow fever causes 200,000 illnesses and 30,000 deaths every year in unvaccinated populations.[5]
Epidemiology
Yellow fever occurs only in Africa, South and Central America, and the Caribbean.[6] Most outbreaks in South America are to people who work within the tropical rain forests and have direct contact with the organisms within the rainforest. The disease can remain locally unknown in humans for long periods of time and then suddenly break out in an epidemic fashion. In Central America and Trinidad, such epidemics have been due to a form of the disease (jungle yellow fever) that is kept alive in Red Howler monkey populations and transmitted by Haemagogus mosquito species which live only in the canopy of rain forests. The virus is passed to humans when the tall rainforest trees are cut down. Infected woodcutters can then pass on the disease to others via species of Aedes mosquitoes that typically live at low altitudes, thus triggering an epidemic.[7]
Risk Factors
A traveler’s risk of acquiring yellow fever is determined by various factors, including immunization status, location of travel, season, duration of exposure, occupational and recreational activities while traveling, and the local rate of virus transmission at the time of travel. Although reported cases of human disease are the principal indicator of disease risk, case reports may be absent because of a high level of immunity in the population (e.g., due to vaccination campaigns), or because cases are not detected by local surveillance systems (1). Only a small proportion of yellow fever cases is recognized and officially reported because the involved areas are often remote and lack specific diagnostic capabilities. During interepidemic periods, low-level transmission may not be detected by public health surveillance. Such interepidemic conditions may last years or even decades in certain countries or regions. This “epidemiologic silence” does not equate to absence of risk and should not lead to travel without the protection provided by vaccination. Surveys in rural West Africa during “silent” periods have estimated an annual incidence of yellow fever of 1.1-2.4 cases per 1,000 persons and 0.2-0.5 deaths per 1,000 persons. YFV transmission in rural West Africa is seasonal, with elevated risk during the 2-4 months that the rainy season ends and the dry season begins (usually July-October); therefore, the annual incidence reflects incidence during a transmission season of 2-4 months. The incidence of yellow fever in South America is lower than that in Africa because the mosquitoes that transmit the virus between monkeys in the forest canopy do not often come in contact with humans and because immunity in the indigenous human population is high. Urban epidemic transmission has not occurred in South America for many years, although the risk of introduction of the virus into towns and cities is ever present. For travelers, the risks of illness and death due to yellow fever are probably 10 times greater in rural West Africa than in South America; the risk varies greatly according to specific location and season. In West Africa, virus transmission is highest during the late rainy and early dry seasons (July-October). In Brazil, the risk of infection is highest during the rainy season (January-March) (2). The low incidence of yellow fever in South America, generally a few hundred reported cases per year, could lead to complacency among travelers. However, it is important to note that four of the six cases of yellow fever reported among travelers from the United States and Europe in 1996-2002 acquired yellow fever in South America (3-8). All six cases were fatal and occurred among unvaccinated travelers. An increase in enzootic and epizootic yellow fever transmission in South America during the 1990s and the potential for epidemiologic change in the Americas remains a concern (see Chapter 5). The risk of acquiring yellow fever is difficult to predict because of variations in ecologic determinants of virus transmission. As a rough guideline, the risks of illness and death due to yellow fever in an unvaccinated traveler in endemic areas in West Africa during the highest risk season from July to October have been estimated at 100 per 100,000 and 20 per 100,000 per month, respectively; for a 2-week stay, the estimated risks of illness and death were 50 per 100,000 and 10 per 100,000, respectively (2). The risks of illness and death in South America are probably 10 times lower (5 per 100,000 and 1 per 100,000, respectively for a 2-week trip) (2). These estimates are based on risk to indigenous populations and may not accurately reflect the true risk to travelers, who may have a different immunity profile, take precautions against getting bitten by mosquitoes, and have less outdoor exposure. Based on data for U.S. travelers during 1996-2004, the overall risk for serious illness and death due to yellow fever in travelers has been roughly estimated to be 0.05 -0.5 per 100,000 travelers to yellow fever-endemic areas. This range reflects an unvaccinated population of 10-90% and assumes that all travelers visiting holo-endemic countries are at risk and 10% of travelers to non holo-endemic countries are visiting risk areas.
Pathogenesis

Yellow fever is caused by an arbovirus of the family Flaviviridae, a positive single-stranded RNA virus. Human infection begins after deposition of viral particles through the skin in infected arthropod saliva. The mosquitos involved are Aedes simpsaloni, A. africanus, and A. aegypti in Africa, the Haemagogus genus in South America,[5] and the Sasbethes genera in France. Yellow fever is frequently severe but more moderate cases may occur as the result of previous infection by another flavivirus. After infection the virus first replicates locally, followed by transportation to the rest of the body via the lymphatic system.[8] Following systemic lymphatic infection the virus proceeds to establish itself throughout organ systems, including the heart, kidneys, adrenal glands, and the parenchyma of the liver; high viral loads are also present in the blood.[1] Necrotic masses (Councilman bodies) appear in the cytoplasm of hepatocytes.[8],[9] There is a difference between disease outbreaks in rural or forest areas and in towns. Disease outbreaks in towns and non-native people are usually more serious.
History

Yellow fever has had an important role in the history of Africa, the Americas, Europe, and the Caribbean.
Europe 541-549
Fragile after the fall of Rome, Europe was further weakened by "Yellow Plague" (Yellow Fever). The Byzantine Empire suffered as well.[10]
Havana, Cuba: 1762-1763
British and American colonial troops died by the thousands in Havana between 1762-1763. Epidemics struck coastal and island communities throughout the area during the next 140 years.
Philadelphia: 1793
In 1793, the largest yellow fever epidemic in American history killed as many as 5,000 people in Philadelphia, Pennsylvania—roughly 10% of the population.[11] At the time, the port city was the largest in the United States, as well as the seat of U.S. government (prior to establishment of the District of Columbia). Philadelphia had recently seen the arrival of political refugees from the Caribbean. The summer that year was especially hot and dry, leaving many stagnant water areas as ideal breeding grounds for mosquitoes. The yellow fever outbreak began in July and continued through November, when cold weather finally eliminated the breeding ground for mosquitoes, although the connection had not yet then been established. Thousands of Philadelphians, including prominent government officials like George Washington and Alexander Hamilton fled the national capital. Benjamin Rush, the city's leading physician and a signer of the United States Declaration of Independence, advocated the bloodletting of patients to combat the disease, but the treatment was controversial. Stephen Girard also helped supervise a hospital established at Bush Hill, a mansion just outside Philadelphia. Though many high-ranking people of Philadelphia fled, a few officials stayed. Mayor Matthew Clarkson as well as the mayor's committee tried to hold the city together as the death toll increased.[12] Matthew Carey published a fast-selling chronicle of the yellow fever crisis, A short account of the Malignant Fever, Lately Prevalent in Philadelphia that went through four editions. Although other ethnic groups were included, Carey's account failed to include the involvement of the city's African Americans in the community's response and relief efforts, despite the fact that African American leaders Richard Allen and Absalom Jones had rallied their church community to assist victims. Allen and Jones subsequently wrote a pamphlet, Narrative of the Proceedings of the Black People, During the Late Awful Calamity in Philadelphia, which detailed the contributions of the African Americans during the epidemic.[13]
Haiti: 1802
In 1802, an army of forty thousand sent by First Consul Napoleon Bonaparte of France to Haiti to suppress the Haitian Revolution was dwindled out by an epidemic of Yellow Fever (including the expedition's commander and Bonaparte's brother-in-law, Charles Leclerc). Some historians believe Haiti was to be a staging point for an invasion of the United States through Louisiana (then still under French control).
Norfolk, Virginia: 1855
A ship carrying persons infected with the virus arrived in Hampton Roads in southeastern Virginia in June of 1855 .[14] The disease spread quickly through the community, eventually killing over 3,000 people, mostly residents of Norfolk and Portsmouth. The Howard Association, a benevolent organization, was formed to help coordinate assistance in the form of funds, supplies, and medical professionals and volunteers which poured in from many other areas, particularly the Atlantic and Gulf Coast areas of the United States. See also "The Mermaids and Yellow Jack. A NorFolktale." children's historical fiction written by Norfolk Author Lisa Suhay retelling of the event and founding of the Bon Secours DePaul Hospital system in the United States in response to the epidemic. (http://iparentingmediaawards.com/winners/13/20794-2-751.php)
Carlos Finlay and Walter Reed

Carlos Finlay, a Cuban doctor and scientist, first proposed proofs in 1881 that yellow fever is transmitted by mosquitoes rather than direct human contact.[15] Dr.Walter Reed, M.D., (1851-1902) was an American Army surgeon who led a team that confirmed Finlay's theory. This risky but fruitful research work was done with human volunteers, including some of the medical personnel such as Clara Maass and Walter Reed Medal winner surgeon Jesse William Lazear who allowed themselves to be deliberately infected and died of the virus.[16] The acceptance of Finlay's work was one of the most important and far-reaching effects of the Walter Reed Commission of 1900.[17] Applying methods first suggested by Finlay, the elimination of Yellow Fever from Cuba was completed, as well as the completion of the Panama Canal. Lamentably, almost 20 years had passed before Reed's efforts were recognized while most of the scientific community ignored Finlay's methods of mosquito control. Finlay and Reed's work was put to the test for the first time in the United States when a yellow fever epidemic struck New Orleans in 1905; according to the PBS American Experience documentary The Great Fever, houses were fumigated, cisterns for drinking water were inspected, and pools of standing water were treated with kerosene. The result was that the death toll from the epidemic was much lower than that from previous yellow fever epidemics, and that there has not been a major outbreak of the disease in the United States since. Although no cure has yet been discovered, an effective vaccine has been developed, which can prevent and help people recover from the disease.
Symptoms
The virus remains silent in the body during an incubation period of three to six days. There are then two disease phases. While some infections have no symptoms the first, acute phase is normally characterized by fever, muscle pain (with prominent backache), headache, shivers, loss of appetite, and nausea or vomiting. The high fever is often paradoxically associated with a slow pulse (known as Faget's sign). After three or four days most patients improve and their symptoms disappear. Fifteen percent of patients, however, enter a toxic phase within 24 hours. Fever reappears and several body systems are affected. The patient rapidly develops jaundice and complains of abdominal pain with vomiting. Bleeding can occur from the mouth, nose, eyes, and stomach. Once this happens blood appears in the vomit and feces. Kidney function deteriorates; this can range from abnormal protein levels in the urine (proteinuria) to complete kidney failure with no urine production (anuria). Half of the patients in the "toxic phase" die within fourteen days. The remainder recover without significant organ damage. Yellow fever is difficult to recognize, especially during the early stages. It can easily be confused with malaria, typhoid, rickettsial diseases, haemorrhagic viral fevers (e.g. Lassa), arboviral infections (e.g. dengue), leptospirosis, viral hepatitis and poisoning (e.g. carbon tetrachloride). A laboratory analysis is required to confirm a suspect case. Blood tests (serology assays) can detect yellow fever antibodies that are produced in response to the infection. Several other techniques are used to identify the virus itself in blood specimens or liver tissue collected after death. These tests require highly trained laboratory staff using specialized equipment and materials.
Prognosis
Historical reports have claimed a mortality rate of between 1 in 17 (5.8%) and 1 in 3 (33%).[14] The WHO factsheet on yellow fever, updated in 2001, states that 15% of patients enter a "toxic phase" and that half of that number die within ten to fourteen days, with the other half recovering.[18]
Treatment
There is no true cure for yellow fever, therefore vaccination is important. Treatment is symptomatic and supportive only. Fluid replacement, fighting hypotension and transfusion of blood derivates is generally needed only in severe cases. In cases that result in acute renal failure, dialysis may be necessary. A fever victim needs to get lots of rest, fresh air, and drink plenty of fluids.
Prevention
In 1937 Max Theiler working at the Rockefeller Foundation developed a vaccine for yellow fever that gives a ten-year or more immunity from the disease and effectively protects people traveling to affected areas, while at the same time being a means to control the disease. Woodcutters working in tropical areas should be particularly targeted for vaccination. Insecticides, protective clothing, and screening of houses are helpful but not always sufficient for mosquito control; people should always use an insecticide spray while in certain areas. In affected areas mosquito control methods have proven effective in decreasing the number of cases.[19] Recent studies have noted the increase in the number of areas affected by mosquito-borne viral infections and have called for further research and funding for vaccines.[20],[21]
Who should get yellow fever vaccine?
- Persons 9 months of age or older traveling to or living in a country that requires yellow fever vaccination for certain travelers. Check with your health-care provider.
- Persons 9 months of age or older traveling to a country that does not require yellow fever vaccination but is located in an area where the risk of yellow fever is known to exist. Check with your health-care provider.
Information about known or probable infected areas is available from the World Health Organization (http://www.who.int), the Pan American Health Organization (http://www.paho.org), and CDC (http://www.cdc.gov/travel).
If you continue to live or travel in yellow fever-endemic areas, you should receive a booster dose of yellow fever vaccine after 10 years. Yellow fever vaccine may be given at the same time as most other vaccines.
Who should NOT get yellow fever vaccine?
- Persons who have ever had a life-threatening allergic reaction to eggs, chicken, gelatin or to a previous yellow fever vaccine.
- Infants younger than 9 months of age. For infants 6 to 8 months of age who cannot avoid travel to a yellow fever area, discuss vaccination with their doctor. Under no circumstances should infants younger than 6 months of age be vaccinated.
- Pregnant women and nursing mothers should avoid or postpone travel to a yellow fever area. If travel cannot be avoided, discuss vaccination with your doctor.
- Check with your doctor before getting yellow fever vaccine if: you have a history of allergy to eggs, chicken, or gelatin; you have HIV/AIDS or another disease that affects the immune system; you have been under treatment for 2 weeks or longer with drugs that affect the immune system, such as steroids; you have any kind of cancer; you are taking cancer treatment with X-rays or drugs; your thymus gland has been removed, or if you have a history of problems with your thymus, such as myasthenia gravis, DiGeorge syndrome, or thymoma.
- If you are 65 or older, discuss with your physician the risks and benefits of vaccination in the context of your risk for exposure to yellow fever virus based on your destination.
- If you cannot get the vaccine because of a medical reason and proof of yellow fever vaccination is required for your travel, your doctor can give you a waiver letter. When planning to use a waiver letter, you should also obtain specific advice from the embassy of the country or countries you plan to visit.
- If you cannot get the vaccine, discuss with your doctor other ways to prevent yellow fever.
What are the risks from yellow fever vaccine?
A vaccine, like any medicine, is capable of causing serious problems, such as severe allergic reactions. The risk of a vaccine causing serious harm, or death, is extremely small. Reactions are less likely to occur after a booster dose of yellow fever vaccine than after the first dose.
Mild Problems
- soreness, redness, or swelling where the shot was given
- fever
- aches
- If these problems occur, they usually begin soon after the shot and last for 5-10 days. In studies, they occurred in as many as 25% of vaccine recipients.
Severe Problems
- Life-threatening allergic reaction (approximately 1 reported per 131,000 doses).
- Severe nervous system reactions (approximately 1 reported per 150,000-250,000 doses).
- Life-threatening severe illness with major organ system failure (approximately 1 reported per 200,000-300,000 doses, or 1 reported per 40,000-50,000 doses in people 60 years of age and older). More than half of the people who suffer these side effects die.
What if there is a moderate or severe reaction?
What should I look for?
- Look for any unusual condition, such as a high fever, behavior changes, or flu-like symptoms that occur 1-30 days after vaccination. Signs of an allergic reaction can include difficulty breathing, hoarseness or wheezing, hives, paleness, weakness, a fast heartbeat, or dizziness within a few minutes to a few hours after the shot.
What should I do?
- Call a doctor, or get the person to a doctor right away.
- Tell your doctor what happened, the date and time it happened, and when the vaccination was given.
- Ask your health care provider to file a Vaccine Adverse Event Reporting System (VAERS) form if you have any reaction to the vaccine. Or call VAERS yourself at 1-800-822-7967, or visit their website at http://vaers.hhs.gov.
The National Vaccine Injury Compensation Program
In the rare event that you or your child has a serious reaction to a vaccine, a federal program has been created to help pay for the care of those who have been harmed. For details about the National Vaccine Injury Compensation Program, call 1-800-338-2382 or visit the program's website at http://www.hrsa.gov/vaccinecompensation.
How can I learn more?
- Ask your doctor or other health care provider. They can give you the vaccine package insert or suggest other sources of information.
- Call your local or state health department's immunization program.
- Contact the Centers for Disease Control and Prevention (CDC): call 1-800-232-4636 (1-800-CDC-INFO) or visit the National Immunization Program's website at http://www.cdc.gov/nip.
Yellow Fever Vaccine Information Statement. U.S. Department of Health and Human Services/Centers for Disease Control and Prevention National Immunization Program. 11/9/2004.
Current Research
In the hamster model of yellow fever, early administration of the antiviral ribavirin is an effective early treatment of many pathological features of the disease.[22] Ribavirin treatment during the first five days after virus infection improved survival rates, reduced tissue damage in target organs (liver and spleen), prevented hepatocellular steatosis, and normalized alanine aminotransferase (a liver damage marker) levels. The results of this study suggest that ribavirin may be effective in the early treatment of yellow fever, and that its mechanism of action in reducing liver pathology in yellow fever virus infection may be similar to that observed with ribavirin in the treatment of hepatitis C, a virus related to yellow fever.[22] Because ribavirin had failed to improve survival in a virulent primate (rhesus) model of yellow fever infection, it had been previously discounted as a possible therapy.[23] In 2007 the World Community Grid launched a project where by computer modeling of the Yellow Fever Virus (and related viruses) thousands of small molecules are screened for their potential anti-viral properties in fighting Yellow Fever. This is the first project to utilize computer simulations in seeking out medicines to directly attack the virus once a person is infected. This is a distributed process project similar to SETI@Home where the general public downloads the World Community Grid agent and the program (along with thousands of other users) screens thousands of molecules while their computer would be otherwise idle. If the user needs to use the computer the program sleeps. There are several different projects running, including a similar one screening for anti-AIDS drugs. The project covering Yellow Fever is called "Discovering Dengue Drugs – Together." The software and information about the project can be found at:
See also
- Aristides Agramonte
- Dengue fever
- Carlos J. Finlay
- Wilbur Downs
- Lassa fever
- List of epidemics
- Jesse William Lazear
- Clara Maass
- Walter Reed]
- Max Theiler
- Hideyo Noguchi
References
- ↑ 1.0 1.1 Schmaljohn AL, McClain D. (1996). Alphaviruses (Togaviridae) and Flaviviruses (Flaviviridae). In: Baron's Medical Microbiology (Baron S et al, eds.) (4th ed. ed.). Univ of Texas Medical Branch. ISBN 0-9631172-1-1.
- ↑ Anker M, Schaaf D; et al. (2000-01-07). "WHO Report on Global Surveillance of Epidemic-prone Infectious Diseases" (PDF). WHO. p. 11. Retrieved 2007-06-11.
- ↑ Bollet, AJ (2004). Plagues and Poxes: The Impact of Human History on Epidemic Disease. Demos Medical Publishing. pp. pp. 48&ndash, 9. ISBN 188879979X.
- ↑ Tomori O (2002). "Yellow fever in Africa: public health impact and prospects for control in the 21st century". Biomedica. 22 (2): 178–210. PMID 12152484.
- ↑ 5.0 5.1 "Yellow fever fact sheet". WHO—Yellow fever. Retrieved 2006-04-18.
- ↑ "Yellow fever: a current threat". WHO. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help) - ↑ Theiler, Max and Downs, W. G. (1973). The Arthropod-Borne Viruses of Vertebrates: An Account of The Rockefeller Foundation Virus Program 1951-1970. Yale University Press. ISBN 0-300-01508-9.
- ↑ 8.0 8.1 Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. ISBN 0-8385-8529-9.
- ↑ Quaresma JA, Barros VL, Pagliari C, Fernandes ER, Guedes F, Takakura CF, Andrade HF Jr, Vasconcelos PF, Duarte MI (2006). "Revisiting the liver in human yellow fever: virus-induced apoptosis in hepatocytes associated with TGF-beta, TNF-alpha and NK cells activity". Virology. 345 (1): 22–30. PMID 16278000.
- ↑ "The Yellow Plague". Oxford Journals. Retrieved 2006-11-08.
- ↑ "Yellow Fever Attacks Philadelphia, 1793". EyeWitness to History. Retrieved 2007-06-22.
- ↑ "The Death of "Yellow Jack" (Angelo, M)". JEFFline Forum. Retrieved 2006-04-18.
- ↑ Laurie Halse Anderson (2002). Fever 1793. Aladdin. ISBN 0-689-84891-9.
- ↑ 14.0 14.1 Mauer HB. "Mosquito control ends fatal plague of Yellow Fever". etext.lib.virginia.edu. Retrieved 2007-06-11. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help) (undated newspaper clipping) - ↑ Chaves-Carballo E (2005). "Carlos Finlay and yellow fever: triumph over adversity". Mil Med. 170 (10): 881–5. PMID 16435764.
- ↑ "General info on Major Walter Reed". Major Walter Reed, Medical Corps, U.S. Army. Retrieved 2006-05-02.
- ↑ "Phillip S. Hench Walter Reed Yellow Fever Collection". UVA Health Sciences: Historical Collections. Retrieved 2006-05-06.
- ↑ "WHO Yellow Fever Fact Sheet". Retrieved 2007-02-22.
- ↑ "Joint Statement on Mosquito Control in the United States from the U.S. Environmental Protection Agency (EPA) and the U.S. Centers for Disease Control and Prevention (CDC)" (PDF). Environmental Protection Agency. 2000-05-03. Unknown parameter
|accessmonthday=ignored (help); Unknown parameter|accessyear=ignored (|access-date=suggested) (help) - ↑ Pugachev KV, Guirakhoo F, Monath TP (2005). "New developments in flavivirus vaccines with special attention to yellow fever". Curr Opin Infect Dis. 18 (5): 387–94. PMID 16148524.
- ↑ Petersen LR, Marfin AA (2005). "Shifting epidemiology of Flaviviridae". J Travel Med. 12 Suppl 1: S3–11. PMID 16225801.
- ↑ 22.0 22.1 Sbrana E, Xiao SY, Guzman H, Ye M, Travassos da Rosa AP, Tesh RB (2004). "Efficacy of post-exposure treatment of yellow fever with ribavirin in a hamster model of the disease". Am J Trop Med Hyg. 71 (3): 306–12. PMID 15381811.
- ↑ Huggins JW (1989). "Prospects for treatment of viral hemorrhagic fevers with ribavirin, a broad-spectrum antiviral drug". Rev Infect Dis. 11 Suppl 4: S750–61. PMID 2546248.
Further reading
- Downs, Wilbur H.; et al. "Virus diseases in the West Indies". Caribbean Medical Journal. 1965 (XXVI(1-4)): &ndash, .
- Theiler, Max and Downs, W. G. The Anthropod-Borne Viruses of Vertebrates: An Account of the Rockefeller Foundation Virus Program, 1951-1970. Yale University Press, 1973.
External links
- Beth Israel Deaconess Medical Center: Yellow fever
- WHO site on Yellow Fever
- Health Information for International Travel, 2005-2006:from Centers for Disease Control and Prevention
Historical yellow fever information
- The Great Fever on PBS
- PBS website on the 1793 Philadelphia yellow fever epidemic.
- Yellow Fever in Norfolk and Portsmouth 1855 an extensive website
- Interactive Internet article on the 1855 Yellow Fever Epidemic from Pilot Online, Hampton Roads: a detailed story with maps, slides, and quiz
- New Orleans, 1905: Housing Conditions and the Yellow Fever: a case study
- Yellow fever deaths in New Orleans.
- Enzootic transmission of yellow fever virus in Peru.
- World Health Report on Yellow Fever
Vaccine development
- Turning Yellow - article by Christine Soares
ar:حمى صفراء ca:Febre groga da:Gul feber de:Gelbfieber it:Febbre gialla he:קדחת צהובה ht:Lajonis lt:Geltonasis drugys hu:Sárgaláz ms:Demam kuning dewasa nl:Gele koorts no:Gul feber fi:Keltakuume sv:Gula febern