Wide complex tachycardias examples
| Resident Survival Guide |
| File:Physician Extender Algorithms.gif |
|
Wide complex tachycardia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Wide complex tachycardias examples On the Web |
|
American Roentgen Ray Society Images of Wide complex tachycardias examples |
|
Risk calculators and risk factors for Wide complex tachycardias examples |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
There are several EKG criteria that may help differentiate ventricular tachycardia (VT) from supraventricular tachycardia (SVT) with aberrancy in the patient with a wide complex tachycardia. The diagnosis of VT is more likely if the electrical axis is -90 to -180 degrees (a “northwest” or “superior” axis), if the QRS is > 140 msec, if there is AV dissociation, if there are positive or negative QRS complexes in all the precordial leads, and if the morphology of the QRS complexes resembles that of a previous premature ventricular contraction (PVC).
EKG Examples
Shown below is an EKG demonstrating VT with right bundle branch block.
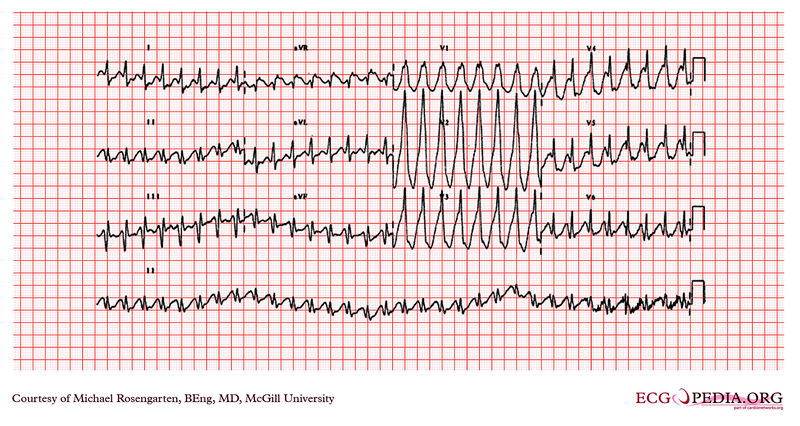
Copyleft images obtained courtesy of ECGpedia.[1]
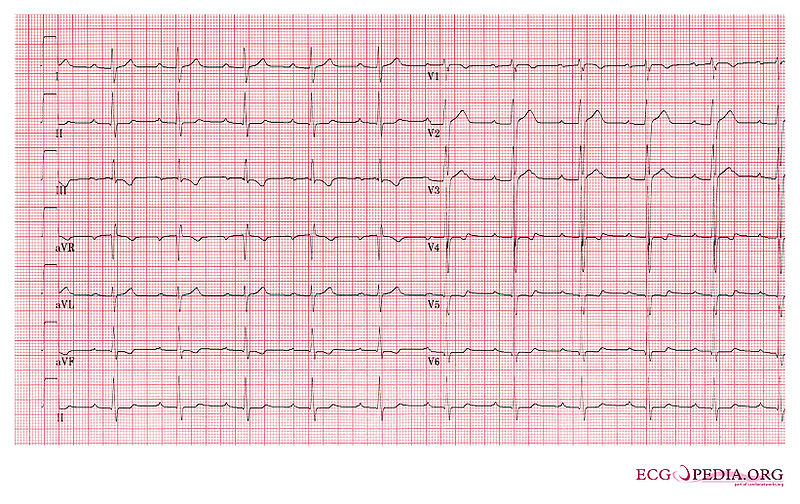
Shown below is an EKG demonstrating sinus tachycardia and WPW which mimics VT.
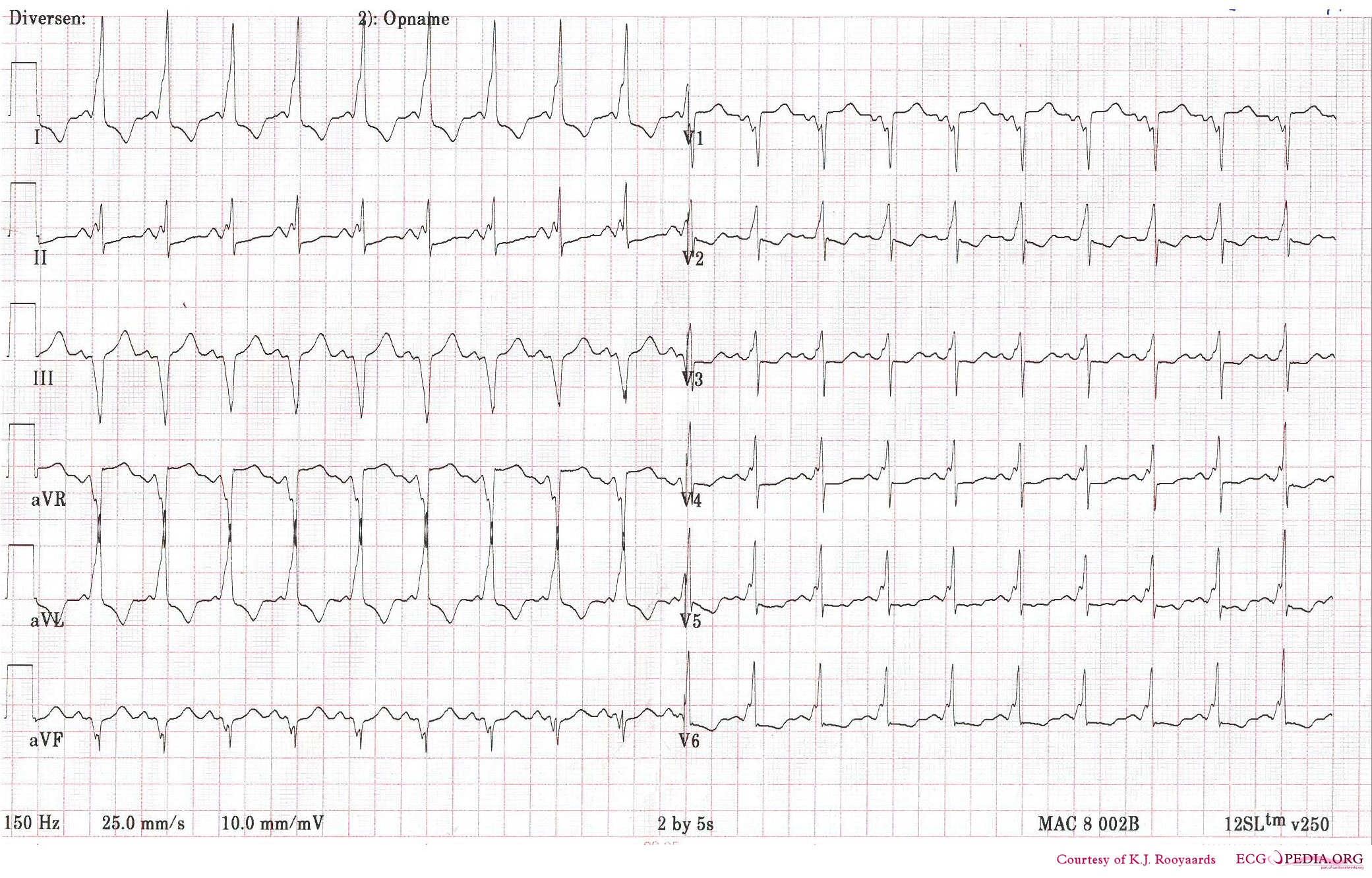
Interpretation of the Previous ECG
Rhythm
- This is a regular rhythm and every QRS complex is preceded by a p wave. The p wave is positive in II,III, and AVF and thus originates from the sinus node. Conclusion: sinus rhythm.
Rate
- Use the 'count the squares' method (a bit less than 3 large squares ~> 300-150-100), thus about 110 bpm and thus sinustachycardia.
Conduction (PQ,QRS,QT)
- PQ-interval=0.10sec (2.5 small squares), QRS duration=0.10sec, QT interval=320ms
Axis
- Positive in I, II, negative in III and AVF. Thus a horizontal (normal) heart axis.
P wave morphology
- The p wave is rather large in II, but does not fulfill the criteria for right atrial dilatation.
QRS morphology
- The QRS shows a slurred upstroke or delta wave.
ST morphology
- Negative T wave in I and AVF. Flat ST in V3-V5.[1]
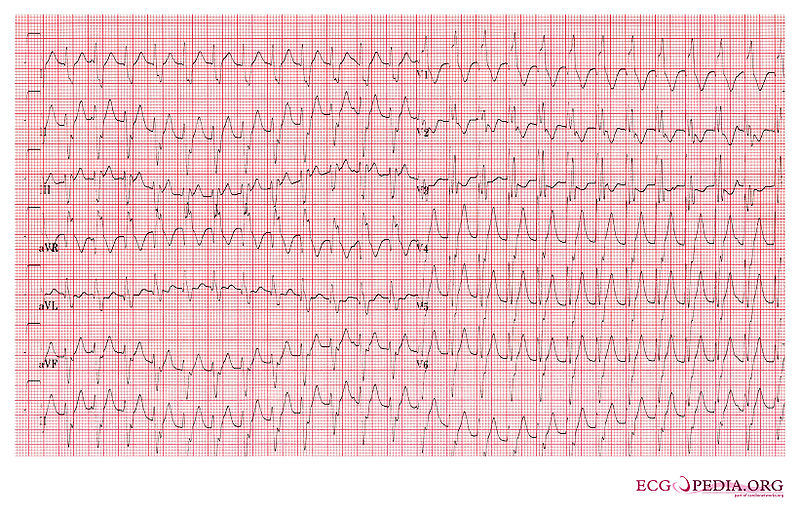
Shown below is an EKG demonstrating wide complex tachycardia at a rate of 160/min with a RBBB, AV disassociation, and extreme right axis deviation as both leads I and aVF are directed downwards. These findings favor VT.
Shown below is an EKG of the same patient after 7.5 mg verapamil was administered, which slowed the VT and caused the AV dissociation to become more apparent.
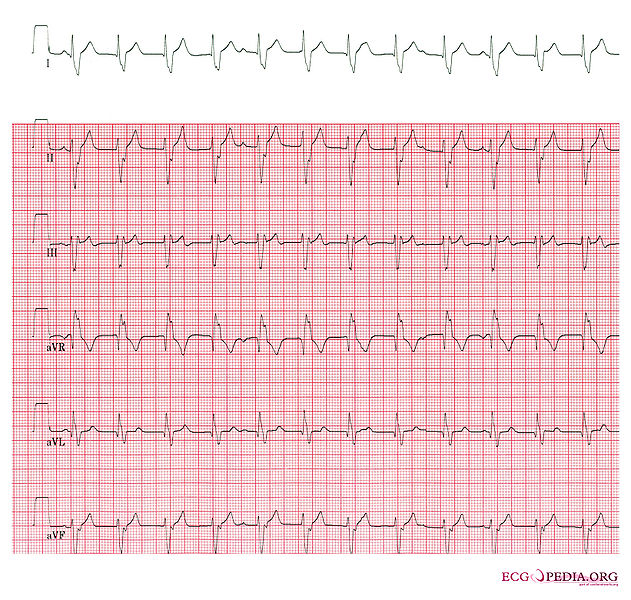
Shown below is an EKG of the same patient who ultimately converted to sinus rhythm.
Copyleft images obtained courtesy of ECGpedia.[1]